In recent years, scleral lens popularity has grown tremendously, with fits and refits up to 16% in 2017 compared with 13% in 2016.1 Although these lenses are problem solvers that can correct for anything from irregular astigmatism and severe ocular surface disease to refractive error and mild-to-moderate dry eye disease, they also present some unique challenges.2
For many scleral lens wearers, the fit may be pristine, the patient may report excellent vision and comfort and handling may be smooth, but poor anterior lens surface wetting hampers comfortable long-term wear (Figure 1). This common issue can cause suboptimal or “cloudy” vision, diminished lens comfort and increased chair time and cost for both the patient and practitioner.3
Also, minimal tear exchange exists during scleral lens wear, causing the potential for fogging in the post-lens fluid reservoir.4-6 Debris accumulation between the scleral lens and cornea can cause lens fogging either rapidly after insertion (sometimes even during the diagnostic lens fitting) or more slowly, worsening throughout the day.7,8
This article discusses the causes of these two frustrating complications in scleral lens wear—and how you can combat them in your practice.
What’s Behind the Curtain
Understanding the risk factors and underlying mechanisms at play can help you better understand why a patient is struggling with wettability, fogging or both.
Wettability refers to how easily a liquid spreads over the surface of a contact lens. It is determined by the wetting angle or contact angle. The contact angle is the angle formed when a drop of liquid is placed on a surface. This angle determines the ability of moisture to spread. Small contact angles are associated with an increased ability of the tears to spread over the surface of a contact lens, leading to a more stable tear film.9-11 A contact angle of zero degrees is a completely wettable surface.12,13
Patients with certain ocular surface diseases are especially at risk for poor surface wettability. Poor tear film quality and stability, lens surface deposits, eyelid disease, allergies, environmental factors and medications can all impede successful contact lens wear.14
This includes those with meibomian gland dysfunction (MGD), ocular rosacea, atopic conditions, graft-versus-host disease, Stevens-Johnson syndrome, Sjögren’s syndrome and other severe ocular surface diseases or filamentary keratitis.
Other culprits for poor surface wettability include excessive lipids in the tear film, exposure from eyelid surgery such as ptosis repair or blepharoplasty, a history of stroke or nerve palsy, poor scleral lens plunger hygiene and use of makeup or oil-based skincare products such as lotions, makeup removers and hand soaps with moisturizing agents. Occasionally, older blocking compounds used during lens manufacturing such as blocking pitch or wax may be the culprit. Exposed silicone on gas permeable lenses, which are innately hydrophobic, inhibits lenses from wetting completely. Low-melt wax is recommended for gas permeable materials due to the polymers being sensitive to heat that could impact the on-eye performance of the material.
Fogging. Risk factors for, and causes of, this complication are not so easily identified. Even with an ideal scleral lens fit and a thorough lens care regimen, fogging may still occur. Factors that have been linked to scleral fogging include increased accumulation of tear debris in the lens reservoir, minimal tear exchange, increased mucin production from conjunctival tissue rubbing, accumulation of protein and lipid deposits on the front surface of the lens and corneal edema.15
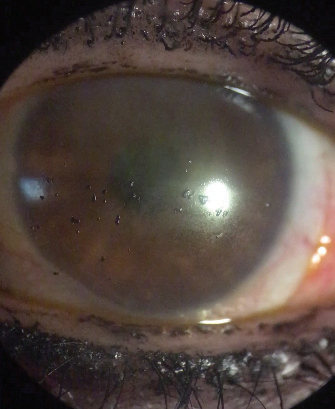 |
| Fig. 1. A scleral lens with front surface debris, as seen here, could cause wettability issues or fogging, both of which complicate comfortable lens wear. Image: Karen Lee, OD |
Finding Clarity
Today, practitioners dealing with poor wettability or lens fogging in their scleral lens wearers have a number of management strategies at their disposal. Here’s how to approach these tricky complications:
Wettability. The first strategy to improve surface wettability in scleral lens patients is simply lens removal, manual cleaning to eliminate deposits (and improve the lens surface), rinsing and reapplication. However, this may be time consuming and inconvenient.
For patients concerned about finding the time and a clean location to perform these steps, on-eye surface cleaning using a saline moistened cotton swab, moistened eye shadow applicator or wet DMV applicator can be used to remove surface debris. Using preservative-free artificial tears throughout the day to increase lubrication over the lens may also be beneficial.
Treating the patient’s underlying condition will yield the best outcome for lens surface wettability. For example, when dealing with poor surface wettability due to MGD, aggressive treatment is critical. If ocular surface disease is not properly managed, the scleral lens surface may continue to be compromised despite changes in lens material and designs.4
Management strategies for these patients include commercial eyelid cleaners, warm compresses, topical eye drops, oral antibiotics and topical antibiotic ointment in the evening. Clinicians should ensure patients using topical antibiotic ointment are educated on the need to remove the ointment using a warm compress on a closed eye prior to scleral lens application. Dietary changes such as omega fatty acid supplementation and reducing fried and fatty foods may help reduce anterior surface debris by creating a more stable and healthier tear film.
Residue left on scleral lens plungers can compromise front surface wettability, and daily disinfection with alcohol may disrupt the hydrophilic lens surface, cause cracks and prevent good suction on the lens. As such, plungers eventually need to be replaced. Some practitioners recommend replacement every three to six months, similar to contact lens case replacement, or sooner if the plunger edges become rough and uneven or if suction is insufficient.16,17
A material with a low wetting angle may improve lens wettability and reduce hydrophobic areas that can attract deposits. In one study, GP materials with a lower wetting angle (less than 90 degrees) may have improved on-eye wettability.18
Plasma treatment may be a unique option to combat lens surface wettability issues. During this process, a finished GP lens surface is bombarded with high frequency radio waves in an ionized gas chamber. This makes hydrophobic surfaces more hydrophilic. Once treated, the lens surface will become ionized, increasing its ability to attract liquids. This results in a decreased (and thus improved) wetting angle, surface tension and deposition of lipids, proteins and bacteria.19 Additionally, this improves wettability and resistance to protein and bacterial deposits. In addition, patients will experience less lens awareness and improved comfort.
Fogging. When dealing with this issue, it is first important to distinguish between anterior surface fogging and post-lens tear reservoir fogging. To do this, note whether the appearance of the presenting fog is more like oil on water or whether it looks milk-like. The former points to anterior surface fogging while the latter represents post-lens tear reservoir fogging.
Clinicians should also rule out corneal edema before assuming the issue is scleral lens fogging. If the patient has hazy vision and sees rainbows around lights, it is critical to evaluate the cornea for microcystic edema, also known as Sattler’s veil. If this is present, scleral lens removal and reapplication will not resolve symptoms—instead, the patient needs medical management for the underlying condition. In these cases, scleral lens wear may need to be discontinued completely or may be worn on a limited wear basis. Instruct patients to monitor how many hours scleral lenses are worn prior to experiencing hazy vision or rainbows around lights. Be sure to specify prescribed scleral lens wearing time for each eye.
If patients are otherwise healthy, management for lens fogging due to debris varies depending on the type of debris you’re dealing with.20
Opaque, white, fluffy, small debris in the post-lens fluid reservoir is known as mucin debris. For these cases, practitioners should first evaluate the scleral lens fit and look for any signs of giant papillary conjunctivitis (GPC) or peripheral edge lift of the lens.
If GPC is present, try prescribing mast cell stabilizer antihistamine drops, reducing lens wearing time and deep cleaning the lens with sodium hypochlorite-potassium bromide-based system, alcohol based cleaners and enzymatic cleaners. If the lens is treated with Tangible Hydra-PEG (Tangible Science), however, only the first two options are recommended, as deep cleaning will remove the coating.
If peripheral edge lift of the lens is present, the lens edge to eyelid interaction may be the source of the papillary reaction. From there, management strategies include eliminating peripheral edge lift by tightening the peripheral curves or adding toric peripheries, reducing lens wearing time, removing and reapplying the lens, cleaning the lens with an enzymatic cleaner or a sodium hypochlorite-potassium bromide-based system and eliminating preservatives in the cleaning or soaking solution.
The second type of debris has to do with an association between atopic disease and keratoconus.21 These patients present with a diluted milk-like fogging in the post-lens fluid reservoir under the lens. Here, treatment options include reducing excessive edge lift, reducing toric peripheries (if the lens has meridional edge lift), topical mast cell stabilizers, topical (soft) steroids in extreme cases and lens removal and reapplication. Practitioners should also carefully monitor intraocular pressures and rule out infection for patients on daily steroids is strongly advised due to the risk for increased intraocular pressure, cataracts and glaucoma.22 Soft steroids generally come with fewer risks.
Lastly, meibomian debris, caused by MGD or blepharitis, is semi-transparent and looks like olive oil floating on water. Often, it can be refractile and a yellowish color. Aggressively treating the eyelids can reduce this debris. Reducing excessive tear exchange by altering the peripheral curves of the scleral lens can also be beneficial for these patients. If issues with meibomian debris persist, try removing and reapplying the lens.
It’s worth noting that these three types of debris can occur in combination.20 As a result, multiple management strategies may be needed.
Knowing where front surface debris is coming from can also steer your management. A murky lens surface may be due to external sources such as oil-based lotions, makeup or face and hand soaps. In these cases, verify that the patient washes their hands with mild hand soaps such as contact lens or acne treatment hand soaps before handling their lenses and make sure they apply face cream or makeup after lens application. Patients should also avoid using oil-based moisturizers on the eyelids and applying makeup to the inside area of the eyelid margin or meibomian gland orifices, as this increases the risk for MGD or obstruction.23
For patients who regularly wear makeup, using eyeliner pencils and sharpening them before every application can help avoid debris issues.23 Some additional tips for makeup-wearing patients include:23
- Replace moist cosmetics such as mascara monthly.
- Clean makeup brushes regularly.
- Remove makeup daily with a makeup remover or eyelid hygiene product.
- Avoid use of facial cleansers or hand soap to remove eye makeup.
- Remove makeup after removing scleral lenses to prevent lens surface residue.
Keeping it Spick and Span
Many strategies can help improve both lens surface wettability and lens fogging. Hydrogen peroxide can be helpful in eradicating lens surface deposits, and according to the Scleral Lenses in Current Ophthalmic Practice study, it is the most commonly recommended disinfection system for this modality.24 Hydrogen peroxide-based solutions are effective for all scleral lenses, especially if the patient has a sensitivity to chemicals or preservatives.
The majority of scleral lenses fit in a standard hydrogen peroxide lens case. However, since these cases were not designed for scleral lens use, some larger diameter lenses may require a larger case. Make sure your patients avoid using tap or distilled water when cleaning their lenses or storage cases due to a risk of Acanthamoeba keratitis.25,26 By the same token, patients should not store their scleral lenses in saline due to a risk of microbial keratitis.27
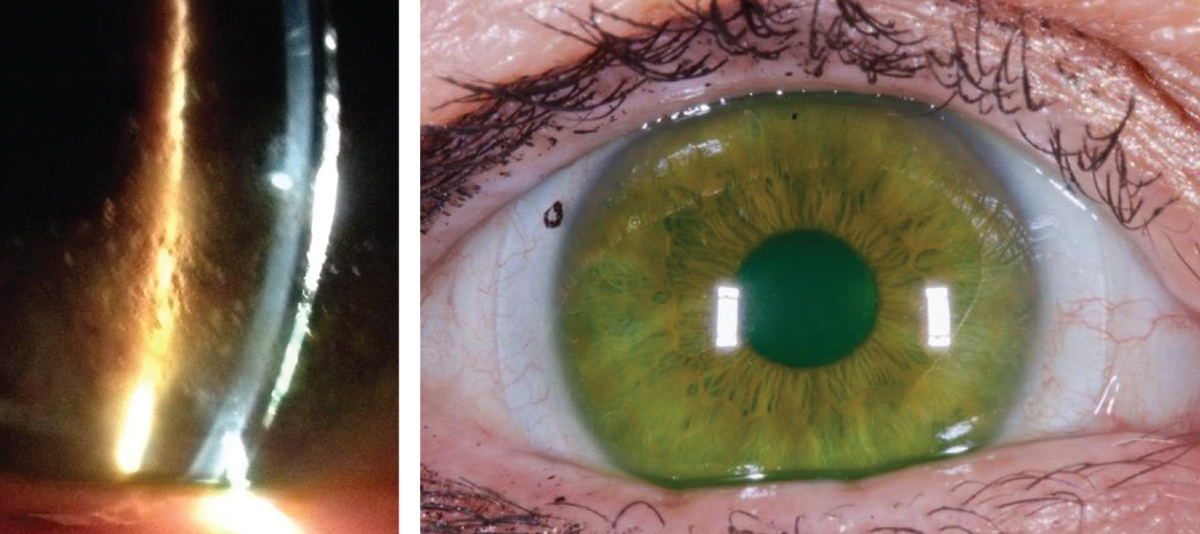 |
| Figs. 2a and 2b. At left, significant surface debris on the lens surface before Hydra-PEG treatment. At right, improved surface wettability after Hydra-PEG treatment. Images: Tom Arnold, OD |
Traditional gas permeable (GP) contact lens disinfection solutions are thick and viscous, which could result in chamber debris and lens surface fogging. As such, some patients may require additional cleaners. Here, alternating between a daily GP lens cleaner and an extra strength or alcohol-based daily cleaner could be helpful.
Patients can add proteolytic enzymes in liquid form such as Opti-free Supraclens (Alcon) and Boston One Step Liquid Enzymatic Cleaner (Bausch + Lomb) directly to hydrogen peroxide or other GP disinfection solutions to remove protein. Some effective alcohol-based cleaners with manual rubbing, meanwhile, include MiraFlow or Optimum extra strength cleaner (Lobob Laboratories).
Another option is Menicon Progent, a chemical biweekly cleaner with a 30-minute soak. This contains sodium hypochlorite and potassium bromide, which serve to loosen and remove surface protein, deposits, bacteria, fungus, molds and yeasts after a 30-minute soak without manual rubbing.28
Treat the Lens, Not the Patient
Tangible Hydra-PEG is a newly FDA-approved treatment option that can help address both wettability and lens fogging concerns. It consists of a 90% water polyethylene glycol-based polymer mixture that permanently encapsulates the lens. This creates a mucin-like wetting surface that shields the lens from the ocular surface and tear film. Hydra-PEG may be used on any type of contact lens to achieve optimal wettability, lubricity, tear film stability and resistance to deposits, so it is no surprise that the treatment has been effective for scleral lens wearers (Figures 2a and 2b).29
Although Hydra-PEG can be used by any contact lens patient, good candidates include scleral lens wearers with a heavy amount of deposits, those experiencing dry eye or discomfort with their lenses and those experiencing lens fogging. Further, Hydra-PEG has no contraindications and requires no lens design changes.
As always, patient education on lens handling remains imperative, especially considering Hydra-PEG treatment results in a more slippery scleral lens. Patients should be instructed to clean their lenses daily with a multi-purpose or hydrogen peroxide solution and to avoid tap water and abrasive or alcohol-based solutions.
Scleral lenses can be a great option for any number of patients, even if wettability and fogging enter the clinical picture. These management strategies, along with proper lens care, can go a long way to ensure healthy life-long scleral lens wear for your patients.
Dr. Barnett is a principal optometrist at the University of California Davis Eye Center in Sacramento, Calif. and Past President of the Scleral Lens Education Society. She is a fellow of the American Academy of Optometry, a diplomate of the American Board of Certification in Medical Optometry and a fellow of the British Contact Lens Association.
1. Nichols J. Contact lenses 2017. CL Spectrum. January 1, 2018. www.clspectrum.com/issues/2018/january-2018/contact-lenses-2017. Accessed March 22, 2018. |


