 A common theme of this column has been effectively keeping patients in contact lenses by making sure to pay attention to those factors likely to erode the experience if not addressed aggressively. Compliance is certainly a pivotal component to that effort. We know that non-compliance can result in uncomfortable lenses as well as more serious complications, including corneal infiltrates and conjunctival injection.1,2
A common theme of this column has been effectively keeping patients in contact lenses by making sure to pay attention to those factors likely to erode the experience if not addressed aggressively. Compliance is certainly a pivotal component to that effort. We know that non-compliance can result in uncomfortable lenses as well as more serious complications, including corneal infiltrates and conjunctival injection.1,2
This month, we discuss the differential diagnosis for contact lens wearers who present with corneal opacities. Keep in mind that other conditions can mimic contact lens–induced complications and need to be ruled out first if we are to bring these patients back to baseline and ultimately allow them to successfully wear lenses long term.
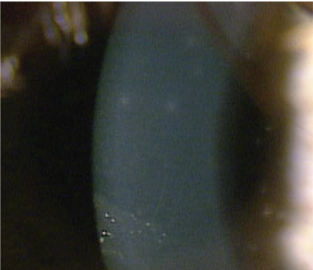 |
| 1. Multiple focal infiltrates characteristic of non-infectious CLAIK. |
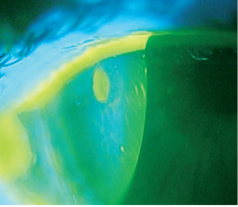 |
| 2. Corneal edema typically accompanies
infectious infiltrate. |
• Infiltrates in Contact Lens Wearers. Infiltrates can occur for a variety of reasons in our contact lens wearers. There are two main categories of infiltrates: non-infectious and infectious. The former tend to occur in multiple areas over the cornea (figure 1). They can be located around the limbus or diffusely seen over the cornea.3 There will usually be minimal or no corneal staining. Symptoms are usually mild to moderate for these patients. Risk factors for non-infectious infiltrates include non-compliance, non-daily disposable lens use, extended wear and silicone hydrogel lenses.2,4
Although these risk factors should be considered, clinically the incidence of symptomatic non-infectious infiltrative keratitis is low—just 0.5-3.3% of those wearing daily wear contact lenses.2,5
Infectious infiltrates usually present as a much more painful event. There is typically one large area that stains with fluorescein, representing the area invaded by the infecting organism, usually surrounded by corneal edema (figure 2). Additionally, these patients often have an anterior chamber reaction.6
• Thygeson’s Superficial Punctate Keratitis. This is a poorly understood condition of unclear etiology.7 Originally described as a transient, bilateral disease, having coarse corneal epithelial opacities and no associated stromal involvement, there is now research that suggests that it may be an anterior stromal condition with manifestations in the epithelium.8 If so, it can involve the subepithelial stroma and presents with small stellate opacities with overlying areas of corneal staining (figure 3). Presenting symptoms are highly variable, with some patients very symptomatic and others asymptomatic.9
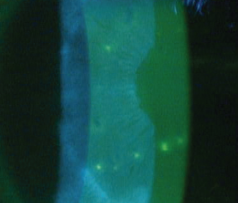 |
| 3. Stellate opacities with overyling areas of
staining in Thygeson’s SPK. |
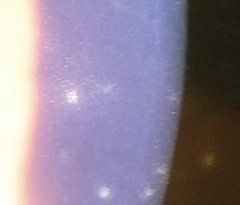 |
| 4. High-magnification view of Thygeson’s SPK
is useful in differential diagnosis. |
The ultimate differentiating factor is the appearance of the corneal lesions. They have a classic stellate pattern that is much more reflective when viewed with a slit lamp. Under low magnification view, they may appear similar to diffuse corneal infiltrates in lens wearers. On high magnification, however, it becomes evident that these lesions are much different than a non-infectious infiltrate (figure 4). It should certainly be considered in the differential diagnosis for those patients with irregular infiltrates.
• Epidemic keratoconjunctivitis. EKC, caused by specific serotypes of adenovirus, is highly contagious and usually associated with significant conjunctival injection.10 It can cause a corneal infiltrative response and should be ruled out whenever patients present with corneal infiltrates.11 Clinically, we have been surprised several times by patients presenting with a diffuse infiltrative keratitis who have been diagnosed with EKC. The ultimate question becomes: How do you distinguish between non-infectious lens-induced infiltrative keratitis and one associated with EKC?
The recently introduced AdenoPlus test (Nicox), which detects all known serotypes of adenovirus, can be used in-office to determine whether the virus is present. With this test, a sample is collected by dabbing and dragging the applicator along the lower palpebral conjunctiva of the worse eye. The sample collector is then snapped into the test cassette and dipped into a buffered solution for 20 seconds. In 10 minutes, the test will yield a result on whether or not the patient is positive for adenovirus.12
This test may prove to be invaluable for clinicians; it ultimately gives us true diagnostic certainty in the exam room and helps differentiate adenoviral keratoconjunctivitis from contact lens infiltrates or CLAIK. In our office, it is performed by our technicians for every patient entering the office with a non-obvious reason for the red eye (i.e., someone who complains of a known incident of foreign body presence in their eye would not need the test performed).
• Adult Inclusion Conjunctivitis. AIC is the clinical manifestation of chlamydial infection. Most often, these patients will have an injected, red eye of varying severity. The palpebral conjunctiva will have a mixed papillary and follicular response.13 Although less common, these patients may have infiltrates present as well. In a contact lens wearer, this can often be confused for an acute red eye or a solution sensitivity. This condition, although usually monocular, can present bilaterally. It is important to rule out AIC if subepithelial opacities are noted.
Conclusion
We must always be attuned to all conditions that cause ocular redness and inflammation, making sure we keep these in our differential diagnosis as we examine contact lens wearers who seemingly present with lens-induced complications. Ultimately, the cause may be unrelated to contact lens wear at all. With corneal opacities present, too much is at stake not to pursue certainty whenever possible.
1. Doubleton KA, Woods CA, Jones LW, Fonn D. The relationship between compliance with lens replacement and contact lens-related problems in silicone hydrogel wearers.Cont Lens Anterior Eye. 2011; Apr 12 34(5);216-222.
2. Stapleton F, Keay L, Jalbert I, Cole N. The epidemiology of contact lens related infiltrates. Optom Vis Sci. 2007 Apr;84(4):257-72.
3. Baum J, Dabezies OH Jr. Pathogenesis and treatment of "sterile" midperipheral corneal infiltrates associated with soft contact lens use. Cornea. 2000 Nov;19(6):777-81.
4. Chalmers RL, Keay L, McNally J, Kern J. Multicenter case-control study of the role of lens materials and care products on the development of corneal infiltrates. Optom Vis Sci. 2012 Mar;89(3):316-25.
5. Szczotka-Flynn L, Chalmers R. Incidence and epidemiologic associations of corneal infiltrates with silicone hydrogel contact lenses. Eye Contact Lens. 2013 Jan;39(1):49-52.
6. Diagnostic and Treatment Algorithims for Ocular Surface Disease States; Supplement. To Review of Optometry; Oct 2009.
7. Connell PP, O'Reilly J, Coughlan S, Collum LM, Power WJ. The role of common viral ocular pathogens in Thygeson's superficial punctate keratitis. Br J Ophthalmol. 2007 Aug;91(8):1038-41. Epub 2007 Mar 27.
8. Fite SW, Chodosh J. Photorefractive keratectomy for myopia in the setting of Thygeson's superficial punctate keratitis. Cornea. 2001 May;20(4):425-6.
9. v an Bijsterveld OP, Mansour KH, Dubois FJ. Thygeson's superficial punctate keratitis. Ann Ophthalmol. 1985 Feb;17(2):150-3.
10. Schneider HA, Dohlman CH. Diffuse subepithelial infiltrates of epidemic keratoconjunctivitis. Arch Ophthalmol. 1973 Nov;90(5):407.
11. Dosso AA, Rungger-Brändle E. Clinical course of epidemic keratoconjunctivitis: evaluation by in vivo confocal microscopy. Cornea. 2008 Apr;27(3):263-8.
12.
http://www.nicox.com/index.
13. Rolf Ronnerstam, Kenneth Persson, Holger Hanson, and Kay Renmarker. Prevalence of chlamydial eye infection in patients attending an eye clinic, a VD clinic, and in healthy persons. British Journal of Ophthalmology. 1985;69:385-388.


