There is no lack of information on fitting and troubleshooting scleral lenses, as well as advertisements for new soft contact lens materials and parameters. But the same cannot be said for specific gas permeable (GP) materials. ODs also have a wide array of lens materials at their disposal in this modality, but many may not know how to select the best option for their scleral lens patients, especially with the significant increase in their use for both irregular and normal corneas. This article discusses how ODs can improve their scleral lens fittings with a better understanding of lens material choices.
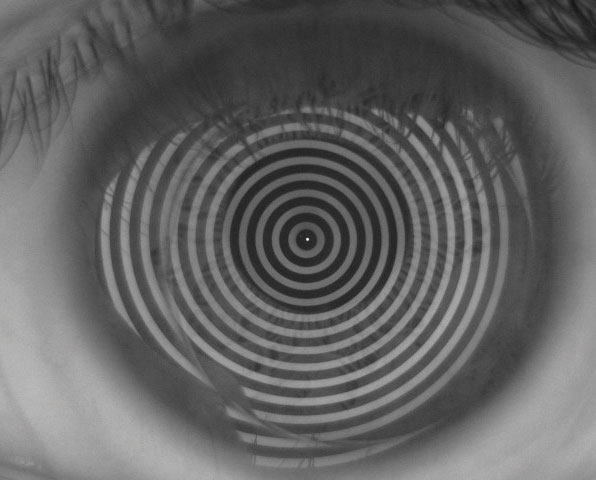 |
| Fig. 1. Passive topographical analysis of tear break-up time shows a well-maintained tear layer over an untreated roflufocon scleral lens after more than 15 seconds. |
General Principles
Compared with corneal GPs, scleral lenses create a semi-seal around the conjunctiva and sclera, which limits tear exchange underneath the lens. This can result in reservoir fogging, a primary complication of an improperly fit scleral lens.1 Because of the limited tear exchange, oxygen to the cornea must come via transmission through the lens and the tear reservoir itself. Thus, one of the most important lens parameters is the material’s oxygen permeability, or Dk value. For scleral lenses, a high Dk lens material is required, with greater than 100 to 150 being ideal.2,3
When it comes to oxygen transmission, high Dk is only one piece of the puzzle. We can also control oxygen transmissibility through adjusting the center thickness of the scleral lens. Thicker lenses hinder oxygen transmission across the lens, while thinner lenses make oxygen transmission easier. According to theoretical models, a center thickness between 250µm to 400µm is ideal to prevent or limit corneal hypoxia.3 When designing center thickness, we must be careful to avoid lens flexure and the induction of residual astigmatism in a lens that is too thin. High oxygen transmissibility is especially important in more advanced corneal ectasias and in patients with corneal grafts. These compromised corneas require high levels of oxygen to prevent further endothelial degradation and risk of graft rejection. In addition, we also must be cognizant of oxygen transmission in older patients due to natural endothelial loss with age.
Other important characteristics in the consideration of scleral lens materials include wetting angle and refractive index. Many ways to measure wetting angle exist, making comparison across lens materials difficult. Generally speaking, a lower wetting angle corresponds to better lens wettability, although this does not always correspond to better lens wetting when on the eye. In theory, better wetting results in less transient dry spots on the contact lens surface. This increases the risk for anterior surface deposition, especially in patients with dry eye disease.
Anterior surface deposition must be differentiated from deposition on the back surface of the lens, which is most prevalent when an incomplete seal around the scleral haptic exists. This is also more common in patients with dry eye.
To help prevent anterior surface fogging and deposition, clinicians should consider the wetting angle when selecting a contact lens material. In general, we start patients in lens materials that have a good balance between high Dk and low wetting angle to provide consistent oxygen transmissibility and low risk of anterior surface deposition.
The refractive index of most lens materials ranges from 1.3 to 1.5, which typically matters more in large prescriptions for patients with corneal complications such as severe keratoconus. Just as in a pair of glasses, clinicians should consider a higher refractive index in higher plus or minus prescriptions to keep the lens thinner.4
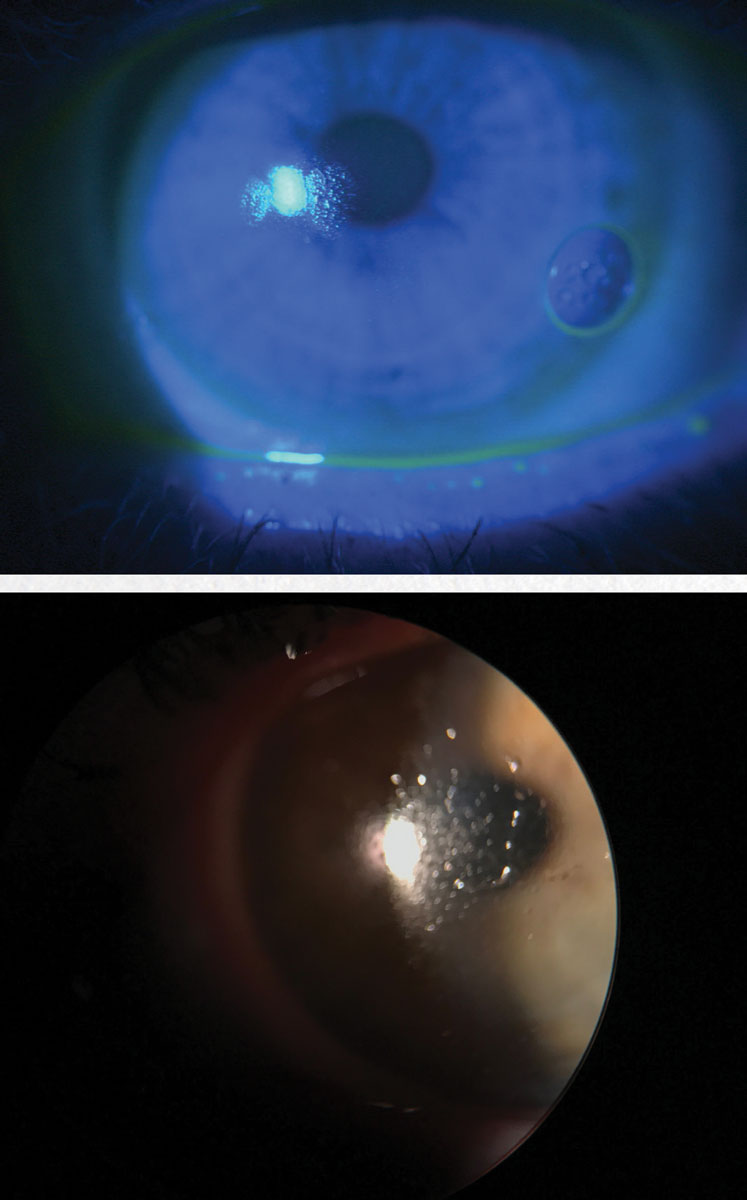 |
| Fig. 2. This patient had anterior surface fogging and deposition while wearing hofocon A lenses. The deposition resolved after switching the patient to an onsifocon A lens. |
Today's Lens Options
Many new GP lens materials have made their way into clinical practice in recent years, all of which provide certain benefits to scleral lens patients:
Roflufocon A-E (Optimum, Contamac) is a family of low- to high-Dk lens materials made of fluorosilicone acrylate (Figure 1). Roflufocon A and C are not used in scleral lens wear due to their low Dk values of 26 and 65, respectively. Roflufocon D, marketed as Optimum Extra, is a good starting material for most scleral lens patients, with its low wetting angle of 3 degrees (Dynamic Contact Angle) and high Dk of 100. Roflufocon E, labeled Optimum Extreme, has a Dk of 125 and a wetting angle of 6, making it a better choice for higher prescriptions or lenses requiring greater center thicknesses.5
Roflufocon can also be paired with the Hydra-PEG (Tangible Science) coating to help improve comfort for patients with dry eye disease, surface wettability problems and those with significant lipid and protein depositions.
Hexafocon A (Acuity 100, Acuity Polymers; Boston XO, Bausch + Lomb) has a higher wetting angle than roflucon at 23 and may potentially be less wettable, but is still a good choice for any scleral lens wearer due to its high DK of 111.6
While not pertaining directly to scleral lens wear, a 2015 study in rabbits showed the lack of inflammation, epithelial or stromal thickening and neovascularization of hexafocon A when used as a stromal inlay.7
Hexafocon B (Boston XO2, Bausch + Lomb) is a well-known GP material with a Dk of 141, making it a good option for scleral lens wear. However, it has a high wetting angle of 38 degrees.8
A recent case series of overnight wear of Prose lenses in Boston XO2 for persistent epithelial defects showed complete resolution of the defects and the oxygen permeability had no negative effects on corneal health.9
For patients with higher oxygen needs, Boston XO2 should among the first considered. Its higher wetting angle may pose a greater challenge for those with dry eye disease compared with roflufocon D and E or hexafocon A, although this may be mitigated through the addition of Hydra-PEG.10
Hofocon A (TYRO-97, Lagado Corporation) is a go-to material for patients with wetting and depositing issues. It has a slightly lower Dk at 97 and a wetting angle of 23 degrees. According to the company, the surface of the fluorosilicone acrylate material is hydrophilic, which increases wettability and lubricity beyond other materials with similar wetting angles.11
Despite having a Dk lower than 100, a study of new miniscleral lens wearers showed an average corneal edema of 1.51% after five hours of wear. Interestingly, this lack of edema was independent of post-lens tear thickness.12 Switching patients that have a tendency to deposit to a hofocon A lens material is often a quick fix while managing their dry eye and anterior surface disease.
Tisilfocon A (Menicon Z, Menicon) was the first GP material FDA approved for continuous wear up to 30 days. It has the highest Dk of all GP materials at 163 and a polymer structure of siloxanylstyrene, fluoromethacrylate and benzotriazol UV blocker, makes it different than most fluorosilicone acrylate GP materials.13
It has a slightly higher wetting angle than others of 24 degrees after soaking the lens. Tisilfocon A is used extensively in overnight wear for orthokeratology and corneal GPs. In corneal lenses, an evaluation of 21 rigid GP wearers showed no corneal endothelial morphology changes after a year of nearly continuous wear.14
While overnight scleral lens wear is still not recommended, it is showing significant potential for the treatment of ocular surface diseases such as persistent corneal epithelial erosion, Stevens Johnson disease, exposure keratitis and post-radiotherapy keratopathy.15 One study found no adverse affects of overnight wear of GP scleral lens in four healthy volunteers on four different occasions. Corneal edema ranged from 4.9% to 17.5% and was highly correlated with endothelial count density.16
When considering overnight scleral lens wear, clinicians must first weigh the risk of hypoxia against the benefit of the 24-hour hydration of the anterior segment. If overnight scleral use for ocular surface disease management is the chosen management strategy, tisilfocon A is the best lens material due to its hyper Dk properties.
Honorable Mention
Onsifocon A (ONSI-56, Lagado Corporation) is a fluorosilicone acrylate rigid silicone hydrogel material with a low Dk of 56. Clinicians should follow patients fit with this material closely to ensure they do not show any signs of corneal hypoxia or edema. Onsifocon A does, however, have a much lower wetting angle than many other GP lens materials at 7.2 degrees, making it an ideal lens material for dry eye sufferers and heavy anterior surface depositors.17
Some patients motivated to wear scleral lenses continue to deposit heavily on their lenses despite efforts to improve the quality of their lid margins, resulting in poor vision. In these situations, a lower Dk material such as onsifocon A may help patients resist deposition.
Extra ProtectionHydra-PEG is a potential game changer in the specialty contact lens industry by significantly improving the wettability of a scleral lens on the eye, especially in bigger and more stationary lenses. The polyethlene glycol (PEG)-based polymer layer is covalently bonded to the lens surface—completely surrounding the front and back surface of the lens—and resists degradation often seen in plasma coatings. The PEG polymer acts as a mucin-like surface on the contact lens, significantly increasing the binding of the natural tear layers to the lens and maintaining a more intact lipid layer.18 Research shows Hydra-PEG can significantly improve wettability, lubricity and comfort in silicone hydrogel lenses. One study compared end-of-day comfort and surface quality of untreated silicone hydrogel lenses and lenses treated with Hydra-PEG. Those treated with the Hydra-PEG had both significant improvements in end-of-day comfort and improved lens surface quality after eight hours of wear.19 Research continues to evaluate Hydra-PEG-treated lenses.18 The first double-blind, randomized study of Hydra-PEG use in scleral lens wear began in January 2018. Thirty participants were randomized into wearing Hydra-PEG treated or untreated scleral lenses and were evaluated for contact lens discomfort and dry eye symptoms.20 Results are currently under review. The Optimum materials have been approved for use with Hydra-PEG for several years, and Bausch + Lomb recently announced a licensing agreement to use Hydra-PEG with its GP materials. Hydra-PEG will soon be available with Boston XO, XO2, EO and ES in GP and scleral lenses.10 Because our practice is located nearly 7,000 feet above sea level and has an average daily humidity below 50%, Hydra-PEG greatly benefits our scleral lens patients who also have significant dry eye disease and depositing issues. |
Materials Matter: Examples
A high Dk material is ideal to reduce the risk of corneal hypoxia and edema due to scleral lens wear. However, some patients are such strong depositors that even the best high-Dk materials deposit quickly. In this patient’s case, aggressive dry eye and ocular surface management coupled with scleral lens material changes were key to decreasing the chance of depositing.
A 46-year-old female presented to the clinic with visual distortion, secondary to corneal trauma, so severe that it caused intractable nausea. In the clinic, a GP lens trial removed the distortion. She was then fit in a 16.8mm Custom Stable Elite scleral by Valley Contax with a front surface toric.
This scleral contact lens design can be ordered in a multitude of materials, and we started with Optimum Extra for its balance of wettability and oxygen transmissibility. She deposited heavily on the anterior surface—an issue that improved when the lens was remade in TYRO-97. Despite manual cleaning and hydrogen peroxide-based solution, she continued to deposit on the new material within one to two days. The depositing improved significantly when switched to ONSI-56, improving the quality and stability of her vision (Figure 2).
Another patient, a 62-year-old keratoconic female sought a second opinion in our clinic due to poor success in scleral fitting at another local practice. She was refit into a 15.8mm Custom Stable Elite lens. Despite aggressive dry eye management, she deposited heavily by the end of the day in Optimum Extra lens material. She was switched to the ONSI-56, which allowed her three weeks of wear before the deposition returned. A biweekly Progent (Menicon) treatment regimen was added to resist further deposition.
Due to the material’s low Dk, clinicians must pay close attention to the corneal health in patients wearing lenses of this material. Reservoir depth should be kept below 150µm whenever possible. Regular follow-ups are needed, and clinicians should educate patients to remove the lenses more often during the day to replenish the saline reservoir.
Monitoring endothelial health and corneal thickness as an indicator of corneal swelling is also important in patients wearing these lower Dk materials. Despite the added benefit of reduced anterior surface deposition, this lens material would not be recommended for those patients requiring higher oxygen needs.
Scleral lenses have become popular for the visual correction of those with irregular astigmatism, high astigmatism and normal corneas, and clinicians must be prepared to choose the right lens material for each patient. While the first fit is usually a high Dk lens with a good wettability profile, not all patients will do well with this choice. This is where a better understanding of the various lens materials on the market becomes crucial. Arming ourselves with material knowledge will improve the success of our scleral lens fits and superior patient comfort.
Dr. Manning is the founder and optometric medical director of the Keratoconus and Scleral Lens Institute at Bettner Vision, a specialty contact lens practice in Colorado Springs, CO. He has a passion for fitting scleral lenses and has taught internationally in contact lenses.
1. Johns L. Scleral lenses 601: Advanced applications. Contact Lens Spectrum. October 31, 2016:28-30. 2. DeNaeyer GW. Today’s scleral lens. RCCL. 2012 June;18-22. 3. Michaud L, van der Worp E, Brazeau D, et al. Predicting estimates of oxygen transmissibility for scleral lenses. Cont Lens Ant Eye. 2012;5(6):266-71. 4. Coronis T. Winning the high-index numbers game. 20/20 Magazine. 2009 July. www.2020mag.com/article/winning-the-high-index-numbers-game. Accessed July 11, 2018. 5. Contamac. Tried, tested, and proven. www.contamac.com/sites/default/files/documents/documents/Optimum %7C Brochure.pdf. Accessed August 9, 2017. 6. Acuity Polymers. Package insert for daily wear corneal and semi-scleral lenses. www.acuitypolymers.com/images/pdf/AC100_PackageInsertweb.pdf. Accesed August 9, 2017. 7. Salamatrad A, Jabbarvand M, Hashemian H, et al. Histological and confocal changes in rabbit cornea produced by an intrastromal inlay made of hexafocon A. Cornea. 2015;34(1):78-81. 8. Bausch + Lomb. Boston XO2. www.bausch.com/ecp/our-products/contact-lenses/gp-lens-materials/boston-xo2. Accessed July 5, 2018. 9. He X, Donaldson KE, Perez VL, Sotomayor P. Case series: Overnight wear of scleral lens for persistent epithelial defects. Optom Vis Sci. 2018;95(1):70-5. 10. Bausch + Lomb. Bausch + Lomb announces licensing agreement with tangible science for use of hydra-peg custom contact lens coating. Eyewire News. June 27, 2018. eyewire.news/articles/bausch-lomb-announces-licensing-agreement-with-tangible-science-for-use-of-hydra-peg-custom-contact-lens-coating. Accessed July 5, 2018. 11. Lagado Corporation. Premium GP materials. www.lagadocorp.co/en/products/premium-gp-materials. Accessed July 11, 2018. 12. Tan B, Zhou Y, Yuen TL, et al. Effects of scleral-lens tear clearance on corneal edema and post-lens tear dynamics: a pilot study. Optom Vis Sci. 2018;95(6):481-90. 13. Menicon. Menicon Z. www.menicon.com/pro/our-products/gp-lens/menicon-z. Accessed August 9, 2017. 14. Barr JT, Pall B, Szczotka LB, et al. Corneal endothelial morphology results in the Menicon Z 30-day continuous-wear contact lens clinical trial. Eye Contact Lens. 2003;29(1):14-6. 15. Tappin MJ, Pullum K, Buckley RJ, Pullum KW. Scleral contact lenses for overnight wear in the management of ocular surface disorders. Eye. 2001;15(2):168-72. 16. Smith G, Mireskandari K, Pullum K. Corneal swelling with overnight wear of scleral contact lens. Cornea. 2004;23(1):29-34. 17. GP Lens Institute. GP materials list. www.gpli.info/materials. Accessed July 11, 2018. 18. Sindt CW. Tangible Hydra-PEG: A novel custom contact lens coating technology designed to improve patient comfort and satisfaction. Tangible Science White Paper. 2016. docs.wixstatic.com/ugd/dd2daf_6d730c1482f6450396c734d74c3017b6.pdf. Accessed July 11, 2018. 19. Caroline PJ, André MP. Hydra-PEG: a solution to contact lens discomfort? Poster presented at Global Specialty Lens Symposium, Las Vegas; 2015. 20. ClinicalTrials.gov. Tangible Hydra-PEG: a promising solution for scleral lens wearers with dry eye. clinicaltrials.gov/ct2/show/NCT03417505. Accessed July 5, 2018. |


