Many of our contact lens patients suffer from gritty, burning, watery and irritated eyes after a day of contact lens wear. In fact, about 30% to 50% of contact lens wearers report symptoms of dryness.1-4 Dry eye syndrome is typically classified into two main categories: aqueous deficient and evaporative. It has been found that contact lens wear is associated with a decrease in the number of functional meibomian glands, which may be a cause of dry eye in contact lens patients.5 Although many of our contact lens patients have both types of dry eye, this article focuses on patients with meibomian gland dysfunction (MGD), a primary cause of evaporative dry eye.
As eye care practitioners, it is vital to be able to properly diagnose and manage ocular surface disease in our contact lens patients in order to retain our patients and to reduce contact lens dropout.
Make the Diagnosis
Meibomian gland dysfunction—also referred to as posterior blepharitis—is an inflammation that affects the inner portion of the eyelids including the meibomian glands. Meibomian glands are sebaceous glands that secrete the oily layer of the tear film. Abnormalities in the production of oils by the meibomian and Zeiss and Moll glands can lead to evaporative dry eye, ocular surface inflammation and contact lens intolerance.
MGD, traditionally, is characterized by blocked meibomian glands and is the most common cause of evaporative dry eye.6 A recent survey found that between 37% to 47% of patients reporting to eye care practitioner’s offices have blepharitis.7 The traditional definitions of meibomian gland dysfunction and its classification are currently being modified. A forthcoming report from International Workshop on Meibomian Gland Dysfunction will provide classification of MGD based on based upon pathophysiological changes.8 During a presentation at the 2010 Association for Research in Vision and Ophthalmology, Daniel Nelson, M.D., defined meibomian gland dysfunction as a “chronic, diffuse abnormality of the meibomian glands, commonly characterized by terminal duct obstruction and/or qualitative/quantitative changes in the glandular secretion. This may result in alteration of the tear film, symptoms of eye irritation, clinically apparent inflammation and ocular surface disease.”9 The report also distinguishes between MGD, posterior blepharitis and meibomitis.8 (The full report from the International Workshop on Meibomian Gland Dysfunction will be available this year and discussions on MGD will continue.)
Symptoms of MGD include foreign body sensation, burning, itching, watering and fluctuating or decreased vision. The diagnosis of MGD is difficult because many of the symptoms mirror the everyday complaints by contact lens wearers.
A systematic evaluation of the eyelids, the tear film, the ocular surface and the lacrimal gland is the best method to determine the etiology of the patient’s symptoms. A biomicroscopic evaluation of the closed eye—including the eyelids—should include the examination of the puncta for appropriate positioning and patency. A stenosed punctum, or an improperly positioned punctum due to entropion or ectropion, may be the causative factor for tearing in a contact lens patient with acquired epiphora.
Next, evaluate the tear film and tear meniscus. Look closely at the volume of the tear lake because this may indicate the severity of the dry eye.10 A normal tear meniscus should rise about 0.34mm above the lower lid margin.11 Several studies have found that optical coherence tomography is an effective method to measure tear meniscus height.12,13 A significantly decreased tear volume may signify problems with tear production by the lacrimal gland. A Schirmer Tear Test (without anesthetic) or a Basic Secretion Tear Test (with anesthetic) may be performed to determine adequacy of tear production. The interpretation of results varies, but generally less than 10mm of wetting over five minutes suggests a decrease in aqueous production by the lacrimal gland, or an aqueous deficiency. Alternatively, the phenol red thread test can be performed; less than 10mm wetting in 15 seconds is considered abnormal.
In addition to the tear film volume, the quality of the tear film should be inspected. The tears should not include excessive debris or mucous strands, which may also be indicative of aqueous deficiency. Patients with aqueous deficiency may also have increased tear osmolarity. Tear osmolarity can be measured quickly in-office with the TearLab Osmolarity System. This CLIA-waived tear assay can give a quantitative measurement of the quality of the tear film and may help with classification of your dry eye patients.
The eyelid margins in contact lens patients with reduced wear time must also be carefully inspected for signs of irritation due to contact lens wear. Evaluate the anterior and posterior eyelid margins for signs of inflammation, such as hyperemia, thickening and telangiectasia.
Carefully inspect the orifices of the meibomian glands for evidence of chronic disease, such as atrophy of the ducts—exhibited by lid margin recession—and obstruction of the openings of the meibomian glands—identified by clear or opaque domes over the gland openings.10 In patients with MGD, clogging of the meibomian glands by desquamated epithelial cells is associated with inflammation of the eyelid margins and disruption of the tear film.14 The openings of the meibomian glands are located on the posterior edge of the lid margin and, when expressed, should emit a small amount of clear oily fluid. Decreased quantities of oil or abnormal oil composition in the tear film cause increased evaporation of the tears and decreased ability of the tears to properly protect the ocular surface.
In addition to the clogged meibomian glands and thickened eyelid margins, patients with MGD may have ocular signs such as a reduced tear break-up time (less than 10 seconds), thickened secretions from the meibomian glands and frothing. Frothing of the tears along the eyelid margin suggests overproduction of oils by the meibomian glands.
Assess the stability of the tear film by performing a tear break-up test (TBUT). A TBUT can be performed noninvasively using a Keeler Tearscope, a non-automated keratomoter or a topographer, or it can be performed invasively using NaFL and a cobalt blue filter at the slit lamp. A TBUT of greater than 10 seconds is considered normal and anything less than 10 seconds may indicate instability of the tear film. If these signs are present in contact lens patients complaining of reduced wear time or contact lens intolerance, the patient may be suffering from meibomian gland dysfunction.
Create a Treatment Plan
Once you have concluded that your patient is suffering from MGD, then you must determine whether the patient has meibomian seborrhea and/or meibomitis.
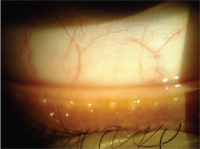
Clogged meibomian glands in a contact lens patient complaining of contact lens intolerance.
Patients with meibomian seborrhea have abnormalities in their meibomian gland secretions, resulting in excessive secretions or meibum that is too easily expressed. These patients may exhibit frothing of their secretions, and these secretions are typically toxic to the cornea.
Patients with meibomitis have an obstruction of the meibomian gland orifices, which may be due to keratinized epithelial cells or alterations in the meibum secreted causing inspissated secretions that block the glands.
• Expression and lid massage: The most effective treatment of any form of MGD with blocked orifices is gland expression and lid massage.15 Meibomian gland expression may relieve chronic meibomitis, as well as open isolated clogged glands. The glands can be expressed initially in the office using a sterile cotton-tipped applicator or a Mastrota paddle. Utilization of a Mastrota Meibomian Paddle (OcuSoft) eases the expression of the meibomian glands.
Donald Korb, O.D., of Boston, and Caroline Blackie, O.D., Ph.D., of Burlington, Mass., have investigated a custom instrument designed to test expressibility of meibomian glands and quantify the force utilized with gland expression.16 Normal glands express clear fluid; in MGD, the expressed material may be a thicker, yellow-white material.17 These thickened secretions require more force than normal to express. Dr. Korb and Antonio Henriquez, M.D., Ph.D., found that even glands that expressed clear fluid with gentle meibomian gland expression may secrete thicker material when increased force is applied.16 An alternate in-office procedure is meibomian gland probing with the Maskin Meibomian Gland Intraductal Probes (Rhein Medical). This probe may be used at the slit lamp to reestablish the patency of the meibomian glands and reduce symptoms of obstructive-MGD.18
Although in-office meibomian gland expression may offer immediate relief for patients, it must be followed with an at-home treatment regimen of warm compresses and digital massage with meibomian gland expression. Normal meibomian gland secretions have a melting point that is less than or equal to the temperature of the ocular surface, around 32° to 34° Celsius.19,20 Inspissated meibomian glands have a melting point that is higher than that of normal secretions.21 Start with the warm compresses because they help warm the eyelids and promote liquefaction of the gland contents prior to expression. The MG Expressor Kit (Gulden Ophthalmics) may assist patients with their home regimen. This meibomian gland expression kit includes a gel mask to warm the eyelids and a Gutierrez Meibomian Gland Expressor. Warm compresses and meibomian gland expression may be prescribed two to four times a day for several weeks, with a reduction in the frequency as the symptoms decrease. Please recall that meibomian gland expression is contraindicated in patients with an acute internal hordeolum.
• Tetracycline or doxcycline: Bacterial lipases present on the ocular surface release free fatty acids, which irritate the ocular surface and promote inflammation. Tetracycline and doxycycline significantly reduce lipase production, causing decreased amounts of free fatty acids and resulting in tear film stabalization.15
Oral tetracycline 250mg q.i.d., or derivatives like doxycycline 100mg b.i.d. and minocycline 50mg b.i.d., can be prescribed for meibomian seborrhea or moderate to severe cases of meibomitis. Tetracycline and doxycycline may be tapered down to a maintenance dosage of 250mg and 20 to 50mg q.i.d. over two to three months. Some patients may be able to discontinue the medication for months at a time, but they usually become symptomatic over time and have to be placed on the medication again.
Expressions of thickened secretions from the clogged meibomian glands of a symptomatic contact lens patient.
Since these medications can irritate the stomach, recommend that they be taken with food. Antacids and dairy products can affect the efficacy of the medication—particularly the absorption of tetracycline. Erythromycin, rather than oral tetracycline, doxycycline or minocycline, should be prescribed to women who are either pregnant or nursing, or to children under age 12.
Lower doses of tetracyclines can also be used as a treatment for MGD. Periostat (doxycycline hyclate, CollaGenex Pharmaceuticals) is a once-a-day tablet originally formulated to treat periodontal disease, but also used off-label to treat MGD. Today, this medication is generically available.
• All-in-one kits: Alodox (Cynacon/OcuSoft) and NutriDox (Advanced Vision Research) convenience kits are becoming a popular option in the treatment of MGD. The Alodox kit includes 20mg doxycycline hyclate tablets, OcuSoft Lid Scrub Plus Extra Strength Pre-Moistened Pads, OcuSoft Lid Scrub Original Formula Foaming Eyelid Cleanser and Tranquileyes Moist Heat Therapy Goggles. Similarly, the NutriDox kit contains 75mg doxycycline monohydrate capsules, the iHeat Warm Compress System and TheraTears Nutrition (omega-3 supplement with vitamin E) oral supplements.
• Azithromycin: Several recent studies evaluating the efficacy of the off-label use of AzaSite (azithromycin ophthalmic solution 1%, Inspire Pharmaceuticals) to treat MGD have suggested an improvement in patient symptoms.22-24 In addition to its other anti-inflammatory properties, azithromycin has been found to inhibit matrix metalloproteinase-9 (MMP-9) activity. MMP-9 is an enzyme that recruits inflammatory cells at sites of inflammation.25
• Nutritional supplements: Nutritional supplements are an important but often-underutilized component of MGD therapy. Omega-3 fatty acids—fatty acids not produced naturally by the body—dampen the inflammatory effects of omega-6 fatty acids, exhibit an anti-inflammatory effect and augment the lipid layer in patients with MGD. Omega-3 can be found in foods such as salmon, flax seed and oil, fish oil, walnuts and sardines. However, many patients find it difficult to ingest adequate amounts of omega-3s through diet alone, so nutritional supplements can be a beneficial addition. Several commercially available supplements formulated specifically for dry eye therapy include HydroEye (Science Based Health), Tears Again Hydrate (Cynacon/OcuSoft) and TheraTears Nutrition (Advanced Vision Research).
Keep the Eye Lubricated
In addition to treating the MGD, it is important to keep the ocular surface properly lubricated. Since the tear components most affected by MGD are the tear lipid layer and the tear film stabilization, it is helpful to prescribe artificial tears designed to stabilize the tear film. FreshKote (Focus Laboratories) is a prescription artificial tear designed to supplement all three layers of the tear film and can be used as needed; it is most commonly recommended for use three to six times a day. A study presented at the 2010 American Academy of Optometry meeting in San Francisco found that using FreshKote four times a day while wearing lotrafilcon A contact lenses (CIBA Vision Night & Day) did not cause a decrease in lens wear time, visual acuity or any visible lens soiling.26 Restoration of the tear’s lipid layer with artificial tear supplementation reduces tear film evaporation and helps alleviate the symptoms of MGD.
Final Instructions
Once a patient with MGD is properly diagnosed and therapy is initiated, additional specific recommendations about contact lens materials, replacement schedules, cleaning products and environmental factors may further improve the outcome.
The water content of a hydrogel lens may be a factor to consider when prescribing contact lenses for patients with MGD. Since these patients tend to have a decreased tear film quality, a lower water content lens may be less likely to dry out on the eye than a higher water content contact lens. In my experience, the two exceptions to this rule are Proclear Compatibles (CooperVision; 62%) and Extreme H20 (Hydrogel Vision; 59% and 54%). Both of these lenses work well with dry eye patients, despite their high water content. The lens material and replacement schedule must be considered.
Silicone hydrogel contact lenses may be more comfortable for some patients with dry eye disorders than hydrogel contact lenses. Daily disposable contact lenses are an excellent choice for patients with MGD. Since these lenses are disposed of on a daily basis, the patient will have minimal interaction with contact lens solutions, which can be an irritant in patients with MGD.
Preservatives in multipurpose contact lens solutions may also contribute to discomfort in MGD patients, so consider hydrogen peroxide-based cleaning systems in this population.
Lastly, don’t forget environmental factors when making recommendations to your patients. Incorporating the use of humidifiers, especially in the winter, can help increase the moisture level of the air and decrease dryness symptoms. Also, recommend that patients discontinue the use of ceiling fans and encourage them to turn their car vents away from their face, as both of these sources of airflow can dry out the ocular surface.
Although MGD is prevalent in many of the patients in our practices, careful evaluation of their eyes, appropriate diagnosis, and targeted treatments and recommendations can greatly improve the contact lens success rate of patients with this disorder.
Dr. Elder is an associate professor at the University of Alabama at Birmingham School of Optometry. She serves as an attending in the Cornea and Contact Lens Service at UAB Eye Care.
1. Nichols JJ, Mitchell GL, Nichols KK, et al. The performance of the contact lens dry eye questionnaire as a screening survey for contact lens-related dry eye. Cornea. 2002 Jul; 21(5):469-75.
2. Begley CG, Chalmers RL, Mitchell GL, et al. Characterization of ocular surface symptoms from optometric practice in North America. Cornea. 2001 Aug;20(6):610-8.
3. Doughty MJ, Fonn D, Richter D, et al. A patient questionnaire approach to estimating the prevalence of dry eye symptoms in patients presenting to optometric practices across Canada. Optom Vis Sci. 1997 Aug;74(8):624-31.
4. Begley CG, Caffery B, Nichols KK, Chalmers R. Responses of contact lens wearers to a dry eye survey. Optom Vis Sci. 2000 Jan;77(1):40-6.
5. Arita R, Itoh K, Inoue K, et al.Contact lens wear is associated with decrease of meibomian glands. Opthalmology. 2009; Mar 116:379–84.
6. Research in dry eye: report of the Research Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007 Apr;5(2):179-93.
7. Luchs J. Azithromycin in DuraSite for the treatment of blepharitis. Clin Ophthalmol. 2010 Jul;4:681-8.
8. Committee aims to hone meibomian gland dysfunction diagnosis, treatment. Ocular Surgery News U.S. Edition. June 10, 2010. Available at:
www.osnsupersite.com/view. aspx?rid=63946 (Accessed February 2011).
9. International Workshop Previews MGD Report.Rev Ophthalmology. 2010 Jun;17(6/1).
10. Krachmer JH, Mannis MJ, Holland EJ, eds. Cornea. 2nd ed. Philadelphia: Elsevier Mosby; 2005:185-90.
11. Bartlett JD, Jannus SD. Clinical Ocular Pharmacology. 5th ed. St. Louis: Butterworth Heinemann; 2008:415-35.
12. Ibrahim OM, Dogru M, Takano Y, et al. Application of visante optical coherence tomography tear meniscus height measurement in the diagnosis of dry eye disease. Ophthalmology. 2010 Oct;117(10):1923-9.
13. Zhou S, Li Y, Lu AT, et al. Reproducibility of tear meniscus measurement by Fourier-domain optical coherence tomography: a pilot study. Ophthalmic Surg Lasers Imaging. 2009 Sep-Oct;40(5):442-7.
14. Henriquez AS, Korb DR. Meibomian glands and contact lens wear. Br J Ophthalmol. 1981 Feb;65(2):108-11.
15. Bartlett JD, Jannus SD. Clinical Ocular Pharmacology. 5th ed. St. Louis: Butterworth Heinemann; 2008:381-413.
16. Korb DR, Blackie CA. Meibomian gland diagnostic expressibility: Correlation with dry eye symptoms and gland location. Cornea. 2008 Dec;27(10):1142-7.
17. DePaolis MD, Gnadt GR, Shovlin JP, Thomann KH. Atlas of Primary Eyecare Procedures. Stanford, CA: Appleton & Lange; 1997:102-5.
18. Maskin SL. Intraductal meibomian gland probing relieves symptoms of obstructive meibomian gland dysfunction. Cornea. 2010 Oct;29(10):1145-52.
19. Shine WE, McCulley JP. Meibomian gland triglyceride fatty acid differences in chronic blepharitis patients. Cornea. 1996; Jul:15(4):340-46.
20. McCulley JP, Shine WE. Meibomian secretions in chronic blepharitis. Adv Exp Med Biol. 1998;438:319-28.
21. Krachmer JH, Mannis MJ, Holland EJ, eds. Cornea. 2nd ed. Philadelphia: Elsevier Mosby; 2005:486-91.
22. Optiz DL, Tyler KF. Efficacy of azithromycin 1% ophthalmic solution for treatment of ocular surface disease from posterior blepharitis. Clin Exp Optom. 2010 Nov. [Epub ahead of print]
23. Haque RM, Torkildsen GL, Brubaker K, et al. Multicenter open-label study evaluating the efficacy of azithromycin ophthalmic solution 1% on the signs and symptoms of subjects with blepharitis. Cornea. 2010 Aug;29(8):871-7.
24. Luchs J. Efficacy of topical azithromycin ophthalmic solution 1% in the treatment of posterior blepharitis. Adv Ther. 2008 Sep;25(9):858-70.
25. Lee YC, Lee HB, Rhee YK, et al. The involvement of matrix metalloproteinase-9 in airway inflammation of patients with acute asthma. Clin Exp Allergy. 2001. Oct;31(10):1623-30.
26. Fuller DG, Connor CG. Safety and efficacy of FreshKote used as a rewetting agent in lotrafilcon-A contact lens wearers. Poster presented at American Academy of Optometry Meeting, November 19, 2010: San Francisco.


