 |
Not much has changed in the management of anterior uveitis over the last several decades. However, researchers have been studying the pathophysiology of the condition to better understand what could alter the disease course. New imaging techniques and drug delivery systems, as well as supplementation and a different class of pharmaceutical, may all one day revolutionize our management strategy for uveitis.
While all of the newer studies have a small sample size, their findings are significant enough to warrant larger studies and further investigation. Here is a look at the latest science enriching our understanding of uveitis.
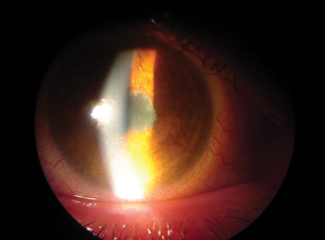 |
| Patients with anterior uveitis are often treated with a potent topical steroid, which can cause an increase in intraocular pressure. New treatments under investigation may avoid this potential adverse effect. Photo: Paul C. Ajamian, OD |
Leaky Vessels
In one study, researchers used ultra-widefield angiography to evaluate 65 eyes in 33 patients diagnosed with anterior uveitis. At the time of angiography, 42% still had active uveitis, while the remaining 58% were classified as inactive and treatment had been discontinued for two weeks to six months (average of 2.4 months). Inactivity was based on no or rare cells in the anterior chamber at the time of imaging.1
Ultra-widefield angiography has the capability to image 150° to 200°, allowing for peripheral retinal evaluation. Traditional fluorescein angiography typically images only 30° to 55°. This study found that 42% (27 eyes) had peripheral vessel leakage, including 12 of the eyes that had been classified as inactive.1,2 These findings altered the management strategy, as those inactive with peripheral leakage were restarted on traditional anterior uveitis treatment.
These findings challenge the classical thinking that the inflammation is limited to the anterior uvea and our ability to determine if it is truly quiescent. The detection of such vascular changes may alter the assessment of disease activity and management decisions.1
Vitamin Deficiency
Research demonstrates vitamin D can reverse uveitis in animal models by inhibiting uveal T-lymphocytes, and a small study evaluated serum vitamin D levels in 20 patients with anterior uveitis and 20 controls.3 Vitamin D helps to regulate the immune system, and a deficiency is linked to cardiovascular disease, cancer, allergies and autoimmune disorders, to name a few.3,4 In this study, fasting venous blood was collected from 20 patients with active anterior uveitis classified as either idiopathic or HLA-B27 positive. Their vitamin D levels were compared with 20 age-matched controls. The researchers found statistically significant lower levels of vitamin D in the group with acute anterior uveitis compared with the vitamin D levels of controls.
Although not an outcome measure of the study, once vitamin D supplementation was initiated, the patients had no recurrence of uveitis.3 Further studies are needed, but these findings suggest vitamin D supplementation may play a role in future management of anterior uveitis.
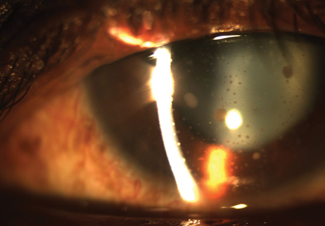 |
| Electronic stimulation of ocular tissues to improve drug penetration—called iontophoresis—may soon be available for anterior uveitis. |
Medical Management
Statins, commonly used in the management of hypercholesterolemia, have been shown in animal models to have anti-inflammatory effects on induced uveoretinitis and rheumatoid arthritis.5 Additionally, a retrospective study in humans showed a decreased risk of uveitis in patients taking statins.6 To further explore this possible association, researchers enrolled 50 patients with uveitis in a prospective, open-label, randomized study. Of the 50 patients, 45 (90%) had anterior uveitis. All patients received traditional management consisting of local and, when necessary, systemic steroids prescribed at the provider’s discretion. Patients were randomized to receive either a placebo or 40mg/day of simvastatin for eight weeks.5 The researchers found those receiving simvastatin had significantly higher rates of steroid-free inflammation control, greater decrease in anterior chamber inflammation and better visual acuity. The simvastatin was well tolerated and no serious adverse events were reported.5 Statins exhibit anti-inflammatory properties and modulate the immune system by inhibiting transcription factors and suppressing production of various pro-inflammatory cytokines such as IL-6, IL-8 and TNF-α.5 Statins are reported to also inhibit leukocyte function antigen-1 from binding, limiting the production of ocular inflammation.5
The authors conclude that statins may be beneficial for the management of anterior uveitis.5 If this does become part of the treatment regimen, eye care providers will need to be reminded of the serious side effects of this class of medications, which includes myopathy, rhabdomyolysis and liver dysfunction.7
Drug Delivery
The EyeGate II drug delivery system, which uses transscleral iontophoresis to deliver controlled therapeutic levels of a drug to the targeted ocular tissue, is currently under investigation and is showing promise. This technology was developed at Bascom Palmer Eye Institute and has been used in over 2,000 clinical trials.8 A low-level electrical current is used to deliver a specific amount of an ionizable drug to the targeted ocular tissue.8
One such drug currently under investigation with this delivery system is EGP-437, which administers dexamethasone phosphate 40mg/mL.8-10 In a Phase III study, patients with anterior uveitis were managed either with traditional therapy or iontophoresis—consisting of two treatments of three minutes/eye. The researchers noted the same rate of response with a total of six minutes of drug delivery vs. traditional drop therapy. This method avoids the shortcomings of traditional eye drop therapy such as poor bioavailability, rapid clearance and poor patient compliance.8 The researchers did notice the incidence of elevated intraocular pressure was less with the iontophoresis group.8
While larger clinical trials are needed, the future for novel yet simplified treatments for anterior uveitis looks bright. These studies may one day lead to actionable management strategies to improve uveitis care.
1. Chi Y, Guo C, Peng Y, et al. A prospective, observational study on the application of ultra-wide-field angiography in the evaluation and management of patients with anterior uveitis. PLoS One. 2015;10(3):e0122749. |


