 |
When an irregular cornea patient no longer achieves optimal vision with standard soft contact lenses, it’s time to take a step back and consider all of the options, including rigid gas permeable (RGP), scleral and specialty soft lenses.
However, long-time soft lens wearers can sometimes be difficult to convert to RGP lenses. They can often struggle with the adaptation period, given that conventional soft lenses are comfortable from the start. This case highlights the challenges of converting a soft lens wearer with pellucid marginal degeneration (PMD) to a rigid lens modality—and what to do when the patient simply can’t adapt.
The Case
A 44-year-old male with PMD was referred to the clinic with complaints of poor vision with his soft toric contact lenses. According to his records, he tried both RGPs and a piggyback system 10 years ago, both without success. Two months ago, his optometrist tried to refit his soft lenses with an updated prescription, but could not get good results. His previous contact lens Rx provided him the best vision, but it was still unsatisfactory.
His presenting contact lens Rx was toric 8.4/-0.50 -4.00x070/14.5 OD, which provided a visual acuity (VA) of 20/30, and toric 8.4/-0.50 -4.75x090 /14.5 OS, with a VA of 20/25-. His manifest refraction was -7.00 +6.25x175 (20/20-) OD and -8.75 +7.00x008 (20/25-) OS.
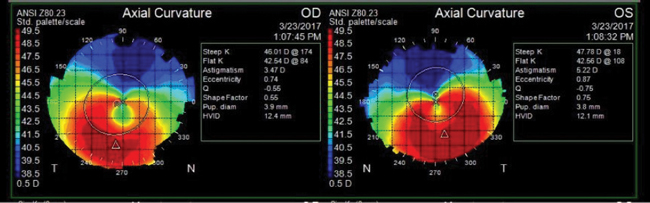 |
| Fig. 1. The patient’s topography exhibits a “kissing dove” pattern typical of pellucid marginal degeneration. |
Slit lamp exam revealed clear lids, lashes and conjunctiva and deep and quiet anterior chambers OU. Inferior central corneal thinning was noted OU. The iris was normal with clear lenses OU. Intraocular pressures (IOPs) were 10mm Hg OD and 11mm Hg OS. Topographical imaging revealed a “kissing dove” pattern characteristic of PMD with simulated K readings of 46.01/42.54D OD and 47.78/45.56D OS (Figure 1).
I discussed the contact lens options available, and the patient said he would try whatever lens would provide him the best vision and comfort. I first chose scleral lenses and started with a 45/-1.50/16.0 Europa (Visionary Optics) lens on the patient’s right eye and a 46/-2.00/16.0 lens for the left. Centrally, the right lens exhibited 200μm of clearance estimated using an optic section through slit lamp, and the left exhibited 250μm of clearance. Both lenses had minor limbal touch 360° OU. Blanching was noted on the landing zone of both scleral haptics. An over-refraction of -4.00 gave 20/20 OD and -3.75 gave 20/20 OS. The patient was thrilled with the comfort and the vision. The following lenses were ordered:
- 45/-5.50/16.2 1 flat edge OD
- 45/-4.75/16.2 1 flat edge OS
The lenses were ordered with a larger diameter to vault the limbus. Because increasing the diameter also increased the apical clearance, the base curve of the left lens was adjusted to lower the vault, and the landing zone was flattened one step in both lenses.
Dispensing Visit
When the patient returned for the lenses, he had a difficult time inserting them. On both eyes, the lenses exhibited an optimal fit: 250μm of apical clearance, 360° limbal clearance and lens alignment with the conjunctiva with no blanching. His vision was 20/20 OU. The patient was able to remove the lenses easily, but because he was not used to inserting lenses face down with fluid and could not keep his eyes open, insertion remained a challenge. As he had no problems with removal, he was sent home to practice.
Week One Follow-Up
The patient presented with complaints that he was not able to wear the lenses. He had a busy schedule and couldn’t find the time to sit and practice insertion and removal. He declined more training. He came to return the lenses and discuss other options. He already had a history of RGP and piggyback lens failure due to inability to adapt to the lenses, and he was opposed to hybrid lenses because of their similar insertion method to sclerals. That left us with specialty soft lenses. After discussing the modality, the patient decided to move forward with that option for its ease of insertion and adaptability.
Fitting, Round Two
I started with a NovaKone (Alden) diagnostic set. Using the fitting guidelines, I put a 8.2/8.6/-5.00/ 15.0, increased thickness (IT) factor 1 lens on the patient’s right eye. I performed manual keratometry over the lens, and the mires were not distorted. An over-refraction of plano +3.50x178 brought the vision to 20/20-.
With the same lens on the left eye, manual keratometry revealed distorted mires -5.00. A lens with the same parameters but with an IT of 2 exhibited more distinct and clear mires. An over-refraction of -1.50 +4.75x007 brought the vision to 20/20-.
Both lenses exhibited good movement and centration with clearance over the apex of the cone. The following lenses were ordered:
- 8.2/8.6/15.0, -1.25, -3.75, 088, IT:1 OD
- 8.2/8.6/15.0, -1.50, -4.75, 097, IT:2 OS
Soft Lens Dispense
When the lenses were placed on the patient’s eyes and evaluated, they exhibited good movement and centration. Vision measured 20/20- OU with no over-refraction. The patient was happy with his vision, but he felt the thickness of the lens was uncomfortable. He was advised to build wearing time and see how the lenses felt in a few weeks.
Two Weeks Later
The patient presented with no complaints, though it took him a week to adjust to lens wear. He also said his vision was not as clear as with the scleral lenses, but was significantly better than the vision provided by his initial soft toric lenses.
Discussion
Patients with an irregular cornea—caused by keratoconus or PMD, for example—who correct relatively well in spectacles (e.g., about 20/30) can often benefit from specialty soft lenses. Although standard toric lenses can sometimes help irregular cornea patients with good spectacle acuity, the final lens power parameters can be difficult to predict through a spectacle Rx due to the draping effects over the irregular corneal surface.
For irregular cornea patients used to standard soft lens who want better vision but are hesitant to convert to an RGP, specialty soft lenses are a good option. Depending on the brand, these lenses have additional parameters such as thickness or size to drape over the cornea to mask irregular astigmatism. They are also more customized than a soft toric lens, providing more control of the way the lens fits over an irregular surface and often leading to slightly more predictable vision. Diagnostic fitting sets and spherocylindrical over-refractions are quite valuable in these cases.
While beneficial in many instances, specialty soft lenses come with a few concerns to be on the lookout for. For one, clinicians must consider the wearing time of these lenses, as they do not provide the same high oxygen permeability as standard soft lenses. Many manufacturers use lens thickness to compensate for the lack of lens rigidity, which can make adaptation more challenging for patients. The higher the IT factor, the thicker the lens: an IT of 0 is 350μm thick, while a lens with an IT of 4 is 750μm. This, combined with a lens material with a dk of 21, can lead to hypoxia if the lens is overworn.1 Patients should be advised to limit their wearing time to prevent corneal neovascularization. This is especially important for patients with keratoconus or other thinning disorders with irregular astigmatism who may one day need a corneal transplant.2
The easy adaptation and superior optics of scleral RGP lenses has made them the go-to choice for hard-to-fit patients. However, one type of lens does not fit all. Every patient is different, and contact lenses must be tailored to their lifestyle and visual needs. In this case, while vision was superior with an RGP lens modality, the patient was happier with a specialty soft lens that was easier to insert and remove, despite slightly reduced vision.
1. Tyler’s quarterly soft contact lens parameters guide. http://tylersq.com. Accessed Feb. 13, 2018. |


