Using an oral omega-3 fatty acid supplement to manage dry eye disease (DED) signs and symptoms offers no improvement over a placebo, a new study found.
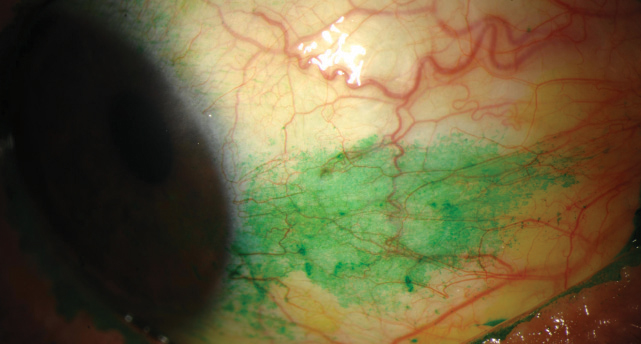 |
| DREAM Study results show no notable difference in conjunctival staining score between patients treated with omega-3 and those given a placebo. Photo: Michelle Hessen, OD |
The Dry Eye and Assessment Management (DREAM) Study, a randomized clinical trial, set out to gauge the long-term safety and efficacy of omega-3 fatty acids for DED treatment. “Many clinicians recommend, and many patients take, dietary supplements of n-3 fatty acids (often called omega-3 fatty acids), because they have anti-inflammatory activity and are not associated with substantial side effects,” the study said.
Researchers randomly assigned 535 patients with moderate to severe DED to receive a daily oral dose of either 3000mg of fish-derived n−3 eicosapentaenoic and docosahexaenoic acids or an olive oil placebo. They primarily looked at mean change in Ocular Surface Disease Index (OSDI) score at six and 12 months, but they also monitored mean changes in conjunctival staining score, corneal staining score, tear film break-up time (TBUT) and Schirmer’s test score to assess supplement efficacy. The results were less than encouraging for use of omega-3 supplementation as a possible dry eye solution, however.
After one year of supplementation, the mean OSDI score change was not significantly different between the omega-3 group and placebo. There was also no significant difference in conjunctival staining score, corneal staining score, TBUT and Schirmer’s test score between the groups.
These results come as a surprise to those who have followed recent positive reports associated with omega-3 fatty acids. “Given the number of other studies that support fish oil, it’s definitely a surprise to hear this outcome,” says Jeffrey Anshel, OD, of Encinitas, CA. “However, I am one who agrees that fish oil does not represent the ‘whole story’ on treating DED.” Instead, Dr. Anshel uses a product with “some fish oil in addition to other ingredients to address the anterior ocular structures.”
Additionally, Dr. Anshel notes that this study may not represent the omega-3 fatty acids as a whole. “Given that many of the trial participants were already using other treatments upon recruitment and continued to use them throughout the study, this was not a study of omega-3 alone,” he says. According to the study, many patients were also treated using included artificial tears, cyclosporine drops, warm lid soaks, lid scrubs or baby shampoo and ‘other’ treatments. “Although the study was well designed, this is a curious aspect to consider,” Dr. Anshel says.
| The Dry Eye Assessment and Management Study Research Group. n−3 fatty acid supplementation for the treatment of dry eye disease. N Engl J Med. April 13, 2018. [Epub ahead of print]. |
Multifocal CL Acuity Similar to Spectacles for Myopic Kids
A center-distance soft multifocal contact lens with an over-refraction provides children with myopia the same visual acuity a spectacle lens, according to research published in the April issue of Optometry and Vision Science.
 |
| A new study shows fitting myopic kids with a +2.50D add center-distance soft multifocal contact lens provides similar visual acuity as spectacles. Photo: Daniel J. Press, OD |
“There is increasing interest in the ophthalmic industry in slowing myopia progression, and early evidence suggests that multifocal contact lenses may be an effective option,” says Daniel J. Press, OD, director of Pediatric Eye Care, Binocular Vision and Vision Therapy Services at North Suburban Vision Consultants in Illinois.
However, “Practitioners fitting contact lenses for myopia control frequently ask whether a myopic child sees well with a high-add multifocal,” says study author Krystal Schulle, OD, of the University of Houston College of Optometry. Her research team decided to find out.
The study enrolled 294 children, ages seven to 11, with myopia of -0.75D to -5.00D and 1.00D cylinder or less. The children were fitted bilaterally with +2.50D add Biofinity (CooperVision) multifocal lenses. The initial multifocal power was the spherical equivalent of a standardized subjective refraction, rounded to the nearest 0.25D step.
“This study found that children who have between -0.75D and -5.00D with less than 1.00D of astigmatism can achieve high contrast best-corrected visual acuity (BCVA) that is equivalent to spectacle correction,” Dr. Press says, “but expect to incorporate an additional -0.50 to -0.75 spherical power in the final lens.”
In addition, neither pupil size nor degree of myopia or astigmatism influenced that amount of over-refraction needed for BCVA, he said.
With a careful over-refraction, these +2.50D add multifocal contact lenses provide good distance acuity, making them viable candidates for myopia control in children, the investigators concluded.
“It is important to note that this study’s purpose is not to evaluate effectiveness of myopia control in bifocal contact lenses, and we will have to wait until completion of the Bifocal Lenses in Nearsighted Kids (BLINK) group for that critical information,” Dr. Press said. BLINK is evaluating the same set of subjects as those in the current report. “What we can take away is confidence in achieving acceptable BCVA in children fit in Biofinity Multifocal +2.50D contact lenses.”
| Schulle K, Berntsen D, Sinnott L, et al. Visual acuity and over-refraction in myopic children fitted with soft multifocal contact lenses. Optom Vis Sci. 2018;95(4):292-8. |
| In Brief Chen X, Sullivan DA, Sullivan AG, et al. Toxicity of cosmetic preservatives on human ocular surface and adnexal cells. Exp Eye Res. 2018;170:188-97. A new study published in Cornea reveals results of long-term follow up post-corneal collagen crosslinking (CXL)—and the data is promising. Researchers looked at 62 eyes of 47 pediatric keratoconic patients who underwent epithelium-off CXL and evaluated uncorrected distance visual acuity, corrected distance visual acuity, Scheimpflug corneal tomography and optical coherence tomography demarcation line measurement at baseline and up to 10 years after treatment. They found CXL was effective at slowing keratoconus progression in nearly 80% of study participants, while also improving functional performance. Mazzotta C, Traversi C, Baiocchi S, et al. Corneal collagen cross-linking with riboflavin and ultraviolet a light for pediatric keratoconus: ten-year results. Cornea. 2018;37(5):560-6. Results from a recent study suggest iontophoretic administration of dexamethasone phosphate 40mg/mL solution is safe and well tolerated for patients with anterior scleritis. Researchers used this treatment on 18 non-infectious scleritis patients at three different doses on day zero and day seven of the study. The primary and secondary endpoints at day 56 were dose-limiting toxicity and improvement on scleritis scale score, respectively. They found a suggestion of efficacy even in the lowest dose group, and five of seven eyes met the primary efficacy outcome within 28 days. O’Neil EC, Huang J, Suhler EB, et al. Iontophoretic delivery of dexamethasone phosphate for non-infectious, non-necrotizing anterior scleritis, dose-finding clinical trial. Br J Ophthalmol. April 17, 2018. [Epub ahead of print]. |


