 |
Many contact lens wearers experience perennial symptoms of ocular allergy that can eventually lead to dropout if not addressed, but some patients are only affected during certain times of the year and thus may not be symptomatic when they come in for their exam. These patients often neglect to mention their symptoms or use of over-the-counter treatments when reviewing their eye history with you. In cases like these, it is important to ask the right questions—you may be surprised what you hear.
Case #1
A 31-year-old male patient presented for a comprehensive eye exam and update of his contact lens prescription. He did not have any comfort complaints, but was having some trouble focusing while using the computer throughout the day. He was wearing monthly disposable contact lenses and replacing them as prescribed. He also reported using the same multipurpose solution he had been using for several years and denied any other ocular or medical changes since his last eye exam.
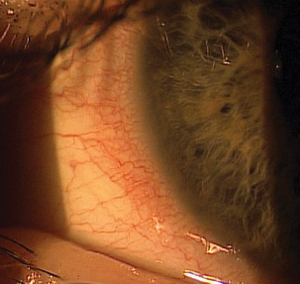 | |
| Fig. 1. Mild limbal injection was observed in a contact lens patient who complained of difficulty focusing while using a computer. | |
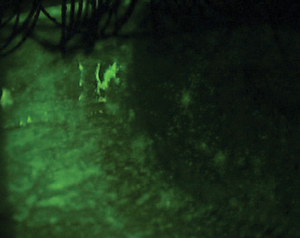 | |
| Fig. 2. Significant staining was observed following use of fluorescein. |
I (Dr. Miller) performed a refraction on this patient to see if we had over-minused him during his last appointment, but found no such issues. With slit lamp evaluation, I observed some mild limbal injection in both eyes (Figure 1). I instilled fluorescein and, upon observation of significant staining (Figure 2), asked him the following questions:
• Do you have seasonal allergies?
• Do you ever use OTC eye drops?
• How often do your eyes itch, water or turn red?
• Do your contact lenses ever become more difficult to wear or less comfortable during certain times of the year or in your work environment?
The patient admitted to using self-prescribed OTC Visine eye drops every few hours per day for approximately the last six months with his contact lenses in. He did not think anything was wrong with his regimen; in fact, he believed it was helping to clear up the redness in his eyes. We gradually tapered the Visine, and he was able to safely return to contact lens wear with no further issues after a couple weeks. I did refit him into daily disposable contact lenses, which eased daily irritation due to long hours on the computer.
Case #2
An 18-year-old female patient presented with ocular discomfort and itching, which she reported increased in severity after taking her contact lenses out each night. To alleviate this discomfort, she had taken to wearing her daily lenses overnight. Her symptoms started approximately one month ago and she stated that she had not been using any eye drops.
Her slit lamp exam demonstrated a moderate amount of conjunctival injection and edema (Figure 3), and her inferior palpebral conjunctiva revealed diffuse G3 papillae throughout (Figure 4), suggesting the presence of allergic conjunctivitis. I discontinued her contact lens wear so that I could get her allergic conjunctivitis under control, first using an ophthalmic steroid and later an antihistamine/mast-cell stabilizer for maintenance. She was able to return to using her daily disposable contact lenses and is no longer sleeping in them overnight.
Asking the right questions and treating patients appropriately can often help you to more easily manage common cases like these. By identifying those contact lens wearers who experience intermittent—rather than constant—visual or symptomatic discomfort, you can proactively help improve all of your patients’ experiences with contact lenses, thus reducing the potential for dropouts and improving the profitability of your practice.
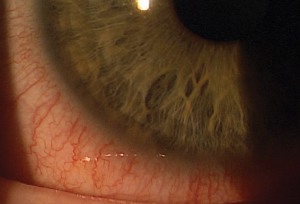 | 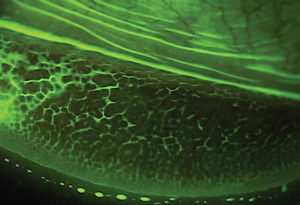 | |||
| Fig. 3. A slit lamp exam revealed moderate conjunctival injection and edema. | Fig. 4. Observation of diffuse G3 papillae, suggesting allergic conjunctivitis. |
| TREATMENT OPTIONS Types of antihistamine/mast-cell stabilizer combination drops include: Astelin (azelastine hydrochloride ophthalmic solution 0.05%, Optivar); Elestat (epinastine hydrochloride ophthalmic solution 0.05%, Allergan); Zaditor (ketotifen fumarate ophthalmic solution 0.025%, Novartis); ketotifen fumarate (Alaway, Bausch + Lomb); Patanol (olopatadine hydrochloride ophthalmic solution 0.1%, Alcon); and Bepreve (bepotastine besilate ophthalmic solution 1.5%, Bausch + Lomb). All should be used twice daily. Pataday (olopatadine hydrochloride ophthalmic solution 0.2%, Alcon), Lastacaft (alcaftadine, Allergan) and the new Pazeo (olopatadine hydrochloride ophthalmic solution 0.7%, Alcon) are all used once daily. Topical steroids may also be an option for patients requiring topical medical treatment for their ocular allergy symptoms in more severe cases or those who are not responding to treatment with the antihistamine/mast-cell stabilizer. Alrex (loteprednol etabonate ophthalmic suspension 0.2%, Bausch + Lomb) and Lotemax (loteprednol etabonate ophthalmic suspension 0.5%, Bausch + Lomb) are two commonly prescribed steroid drops for allergic conjunctivitis. Topical steroids are often used for a pulse during a short period of time (one to two weeks), followed by use of an antihistamine/mast-cell stabilizer for sustained maintenance over a longer period of time. |


