 In fitting a patient who presents with both keratoconus and astigmatism, the need for adding some type of toricity is not always clear. In general, though, we tend to ignore the corneal astigmatism because, in the big picture, the keratoconus is often more significant.
In fitting a patient who presents with both keratoconus and astigmatism, the need for adding some type of toricity is not always clear. In general, though, we tend to ignore the corneal astigmatism because, in the big picture, the keratoconus is often more significant.
Then again, what about the individual who has severe astigmatism but less severe keratoconus? In this instance, the best approach is usually to address the astigmatism primarily and the keratoconus secondarily. Consider the following case.
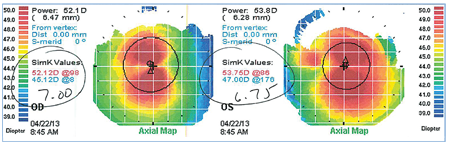 |
| Figure 1. Corneal topography demonstrates steep, highly astigmatic corneas. |
A 27-year-old white male presented for a contact lens fitting upon referral from a LASIK center. He was told he was not a candidate for LASIK due to keratoconus, and was sent to us for new contact lenses.
He reported that he already had GP lenses but, due to the discomfort and instability, he used them only when he played golf. The rest of the time he could function without correction.
His visual acuity without correction was 20/40+1 OD and 20/30-2 OS. Autorefraction yielded OD -1.25-5.75 x 180 and OD -1.75-5.50 x 175. Autokeratometry measured OD 45.75 x 53.50 x 90 and OS 46.25 x 53.25 x 85. We performed corneal topography (figure 1), which correlated well with the autokeratometry results.
Pachymetry measured central corneal thicknesses of 455μm OD and 459μm OS. The combination of steep curvature and thin corneal tissue, as well as the irregular reflex on retinoscopy, indicated that this patient did indeed have mild keratoconus.
Performing manifest refraction was difficult, with poor endpoints and no real improvement in vision no matter what lens was used. This may have been due partially to his adaptation to never having worn correction for the astigmatism, or more likely to the keratoconus creating a muddled endpoint. Whatever the reason for his lack of ability to distinguish clarity between any of the lenses, he preferred a final refraction of OD -0.50 sph to 20/30-1 and -1.00 sph to 20/30 to anything with cylinder in it.
I asked him to insert his current lenses for evaluation. Both lenses—spherical corneal GPs with a diameter of 9.5—fit with significant inferior edge lift and were unstable with eye movement, with his vision correcting to 20/25+1 in each eye with the lenses in. An over-refraction revealed residual astigmatism, likely from lens flexure.
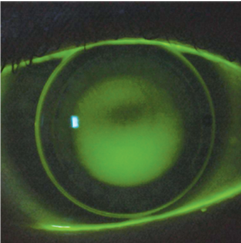 |
| Figure 2. Right eye of patient after being refit
with a bi-toric. Note the apical clearance fit and marking at 3 o’clock, demonstrating rotational stability. |
After discussing his options—including the possibility of trying to adjust his current lens fit, or attempting hybrid or scleral lenses—he decided that he wanted to stay with corneal lenses first. Based upon his corneal topography, I decided to fit him in a bi-toric base curve lens with spherical peripheral curves (figure 2).
The patient returned the following week for a dispensing visit. Upon insertion, he instantly noted that the new lenses felt much less noticeable compared to the old ones. His visual acuity was 20/25 in each eye while wearing the lenses, but a spherocylindrical over-refraction of +2.25-1.00 x 95 OD +1.25-1.25 x 85 OS improved each eye to 20/20 easily.
Because the over-refraction indicated a change in the sphere and cylinder numbers that aligned to the major meridians of the patient’s corneal astigmatism, we were able to incorporate this change in his lenses. In addition, the lenses were marked for rotation, and evaluation revealed a stable fit with no rotation.
The lenses were ordered with the over-refraction incorporated, which provided an excellent fit and clear stable vision OU.
When assessing the need for a toric lens in cases of irregular astigmatism, it’s helpful to place a spherical lens on the eye to assess the fit. If the lens appears to fit as if the eye is highly astigmatic, a toric GP design should work. In this case, the patient’s current lens fit indicated that the astigmatism—more than the keratoconus—was the bigger problem.
Of course, a scleral lens or perhaps even a hybrid would have been just as satisfactory. But the toric back surface corneal lens was at least as effective, and much simpler for all involved.


