The use of custom rigid lenses to reshape the cornea is increasingly prevalent throughout the world, albeit more so in Asia than in Europe and the United States.1-3 Therapeutic orthokeratology lenses are typically fit in Europe to eliminate the need for glasses or contact lenses, while in Asia they are primarily used to control the progression of myopia.1 Europe’s orthokeratology fitting process employs corneal topography with a software-based approach that is supplemented with trial lenses. This is achieved via the manufacturing of contact lenses by a third party, so the practitioner’s knowledge of back surface parameters remains limited. In Asia, however, the fitting process for orthokeratology incorporates topography, trial lenses and fluorescein pattern evaluation, meaning practitioners typically achieve a greater amount of confidence and success with the fitting process, though this is not always the case. This article will discuss the orthokeratology lens fitting process in the context of calculating back lens parameters individually for unusual cases.
 | |
 | |
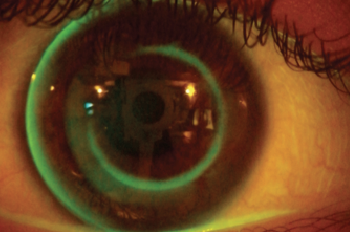
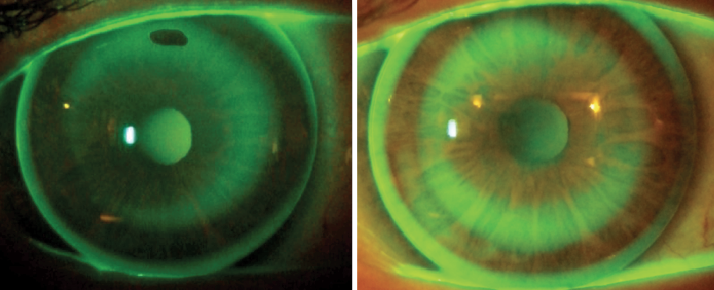
| Fig. 1. Fluorescein patterns of the first pair of lenses, three nights after initiation of treatment. Note, the steep pattern of the lenses is clear. | |
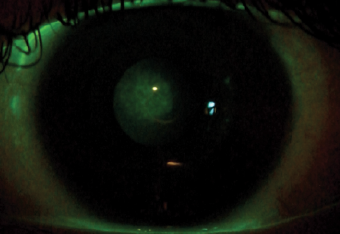 | |
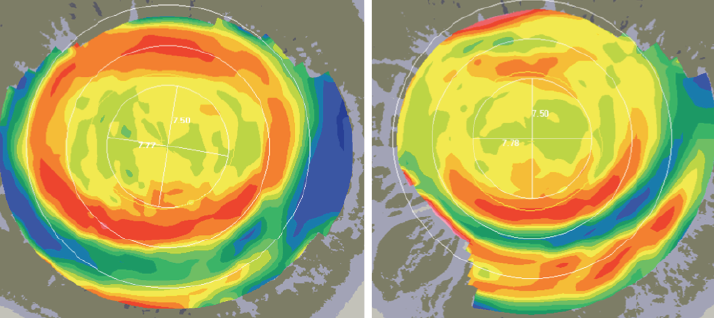
| Fig. 2. Note the corneal staining in the central area. |
1. Teenage Patient
Presentation. A 17-year-old patient underwent an orthokeratology fitting to control her myopic progression, as her mother had myopia in both eyes corrected with eyeglasses (sph -18D). She presented with moderate myopia (-5.50D), a steep and small cornea and a medium-to-low eccentricity value. Her refractive and corneal data were as follows: Rx sph -5.50 cyl -0.50x175° BCVA 20/20, Ks 7.26/7.09mm, average corneal eccentricity E = 0.24, horizontal visible iris diameter 10.60mm and pupil size 3.60mm in the right eye; and Rx sph -5.00 cyl -0.50x10° BCVA 20/20, K 7.24/7.03mm, average corneal eccentricity E = 0.30, horizontal visible iris diameter 10.70mm and pupil size 3.70mm in the left eye.
For this patient, the prescribed lens back surface exhibited a tetracurve design with a back optic zone (BOZ); a first peripheral zone or reverse curve steeper than the BOZ (BPZ1); a second peripheral zone or landing zone flatter than the previous one (BPZ2); and a third peripheral zone steeper than the second one (BPZ3). This approach uses one of several different modern reverse orthokeratology lens designs available on the market. In theory, more curves could occur to smooth the junction’s angle between one curve and another to produce conformal periphery and to increase the lens centration.
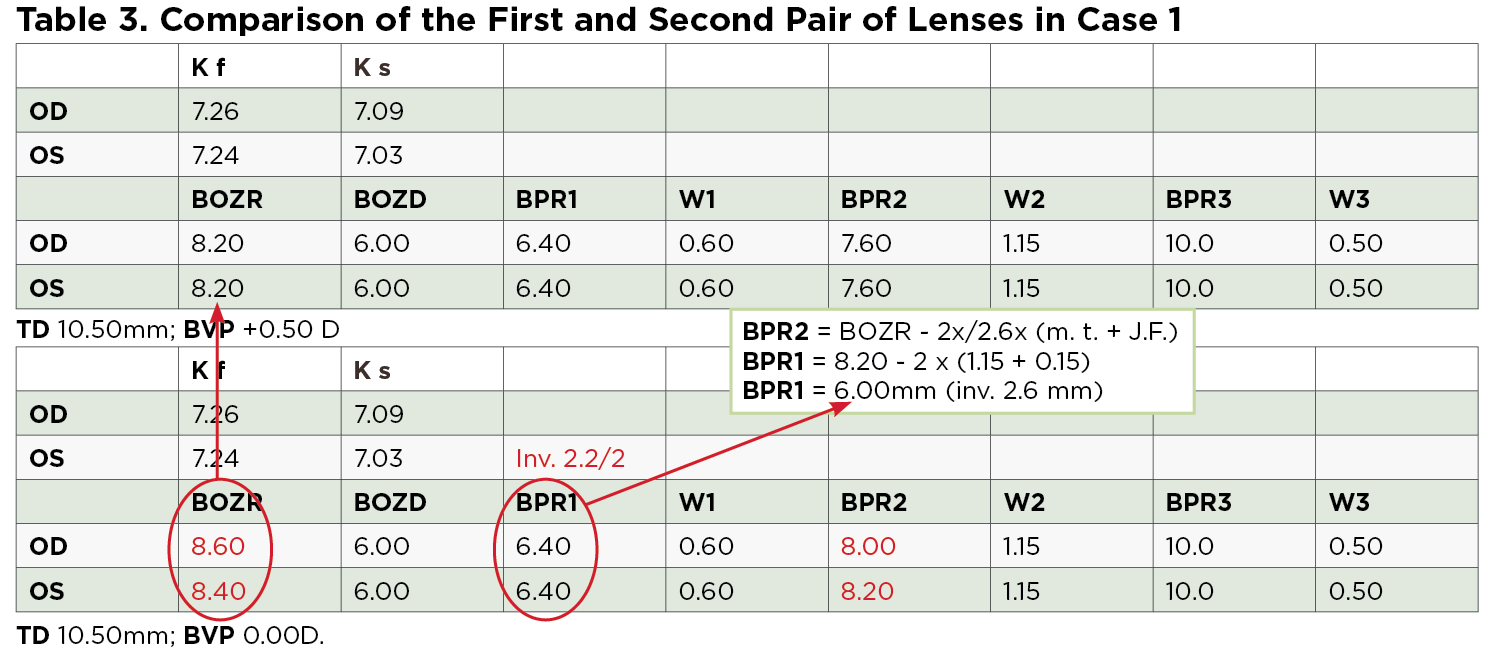
Methods. When choosing the back optical zone radius (BOZR) for the first trial lens, it’s possible to use different formulas.4-7 Additionally, instead of selecting the BOZR, it’s possible to use sag fitting methods.7,8 The indications to calculate these orthokeratology lens parameters (using the Jessen Factor formula) are demonstrated in Table 1, while the parameters of the first pair of lenses fit on the patient in question are shown in Table 2. For the purpose of this discussion, however, it is not relevant which formula is used to calculate the first lens back surface parameters, because the final parameters were revised after evaluating the lens fit on the eye as well as its position, its movement and its fluorescein pattern.
In comparing these parameters with those indicated in the literature, note that the chosen BOZR is 0.36mm shorter; from this, a residual refractive error of 1.75D in the right eye (OD) and 1.25D in the left eye (OS) was then expected. Additionally, the BPR1 was longer with a lower inversion than normal, while the BPR2 was longer than 0.40mm; this could mean a possible lifting of the optical zone with modest result in the treatment. Additionally, note that the lens is fit steeply with central corneal staining most visible after lens removal (Figures 1 and 2). Corneal topography demonstrated the typical central islands that can be induced from a steep lens.
Following this evaluation, new lenses were calculated based on the parameter analysis of the first trial lenses and the fluorescein pattern. The BOZ was flattened according to calculations made previously, which automatically increased the reverse curve, leaving the same BPR1 (Table 3). The BPZ2 was also flattened to allow a lifting of the optical zone to prevent corneal abrasions and allow for a better distribution of epithelial tissue.
Results. Five days after the patient was fit with an orthokeratology lens, her UDVA was 20/25+2 OD with residual refractive errors present in the spectacle plane sph -1.00D and 20/20 OS with residual refractive errors sph -0.50D. Twenty days after the fitting, the patient’s UNVA was 20/16-1 OD with residual refractive errors: sph -0.25D; 20/16 OS with no residual refractive errors; and 20/12.5 in both eyes (OU). The patient reported having good vision with the lenses for up to 15 hours per day, but complained that she sometimes observed visual halos around lights. At her three-and-a-half month follow-up appointment, the UDVA was 20/16 OD with residual refractive errors sph -0.25D and 20/16 OS with no residual refractive errors. The low contrast UNVA was 20/25 OD, 20/25 OS and 20/12.5 OU.
| Potential Orthokeratology Contraindications A better understanding of lens parameters and fitting techniques may allow practitioners to beat some of these typical orthokeratology contraindications: 1. Myopia correction up to -6.00D, due to a lack of predictability of the treatment.8,12 2. Correction of with-the-rule corneal astigmatism higher than 1.50D.22-25 The most common problem in patients with high corneal astigmatism is spherical lens decentration, which can lead to further induced astigmatism and poor vision.24,26 3. Correction of against-the-rule and oblique corneal astigmatism higher than 0.75D.18,19,25,26 This is due to lens decentration, which can induce more astigmatism.24,26 4. Correction of corneal astigmatism. Residual astigmatism can affect refractive outcomes post-treatment.27 5. The need for spectacle lens cylinder to always be less than the spherical power (i.e., less than one-third of the sphere).8 6. Astigmatism spanning limbus-to-limbus because of lens decentration.8 7. Irregular corneal astigmatism, given the difficulty to stabilize the lens on the cornea.8 8. Pupil size of about 5mm to 6mm or larger under dim light conditions.12 Orthokeratology can induce higher-order aberrations, especially spherical aberrations. In patients who have a pupil size greater than 5mm, the amount of high order aberrations increases dramatically. 9. Low corneal eccentricity, in that the correlation between eccentricity and the predictability of the treatment is not well defined, so orthokeratology is only considered safe for correction of myopia less than -4.00D.8,12 | ||
 | ||
 | ||
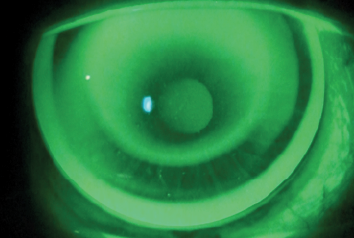
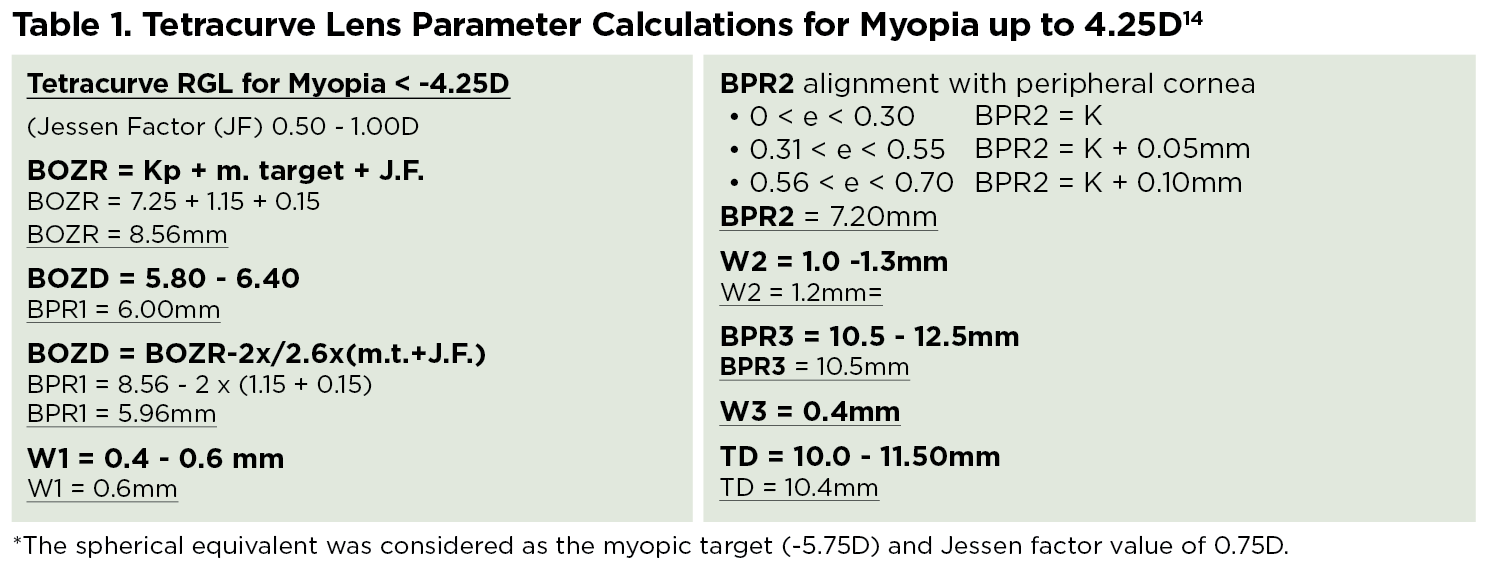
| Fig. 3. Fluorescein patterns of the second pair of lenses, 20 days post-orthokeratology. Both lenses are decentered, compromising the refractive outcome. |
Discussion. Previous research has suggested that low corneal eccentricity is predictive of a lower refractive error change. As such, these results are in agreement with other studies demonstrating that low eccentricity may not be an absolute contraindication to orthokeratology, despite the fact that the patient’s cornea was small and steep with a medium-to-high degree of myopia.8-12 In these cases, the corneal shape becomes oblate due to the negative eccentricity (i.e., E = -1.62 OD and E = -1.50 OS). In the case of this patient, her issue was resolved using a four-curve reverse lens with a mean back optic zone diameter and relatively small total diameter.
2. Contact Lens Dropout
Presentation. A 48-year-old patient presented to the clinic wishing to try wearing orthokeratology lenses to eliminate the need for eyeglasses. She had previously worn soft contact lenses, but had stopped due to resulting dry eye symptoms. Her refractive and corneal data at the time of presentation was Rx sph -0.75 cyl -2.50x170° BCVA 20/16 Add 1.50D, K 7.81/7.49mm, E = 0.10, horizontal visible iris diameter 11.60mm and pupil size 3.40mm OD; and Rx sph -1.50 cyl -1.50x20° BCVA 20/16 add 1.50D, K 7.51/7.29mm E = 0.20, horizontal visible iris diameter 11mm and pupil size 3.50mm OS.
It was noted the patient’s cylindrical component was three times larger than the spherical one in the right eye, while in the left eye they were equal. Also, there was refractive astigmatism (cyl -2.50 OD and cyl -1.50 OS higher than corneal astigmatism (i.e., -1.82D OD and -1.39D OS) and low eccentricity present. Additionally, though the patient’s marginal dry eye was not an absolute contraindication to orthokeratology lens wear, it could challenge the practitioner’s ability to create a reliable topography map, since corneal topographers are typically more effective at generating a clear image when evaluating a wetter corneal surface.12
Few published studies currently exist on the subject of toric orthokeratology for astigmatism, though conference abstracts and case reports on the subject are numerous.13-21 One study was conducted on patients who have astigmatism greater than 1.25D at any orientation.13 The lenses used in this project contained five toric zones with double reverse curves, with the second and the fourth zones being the reverse ones. This design is known as a full toric double reservoir. The researchers suggested that to achieve an adequate effect with a toric orthokeratology lens, mechanical and hydrodynamic forces must occur in different ways in each corneal meridian, with greater flattening in the meridian where the myopia is greater.20 Results demonstrated an 85% change in initial astigmatism.
Another study on patients ranging from six to 12 years old with myopia of 0.50D to 5.00D and with-the-rule astigmatism of 1.25D to 3.50D incorporated a lens characterized by an alignment toric zone with spherical back optics and a reverse zone design.14,15 According to the authors of this study, the advantage of placing a spherical optic zone on a toric cornea is that the flattest lens meridian creates a normal orthokeratology effect, while the steepest meridian results in a greater orthokeratology effect, leading to the correction of the corneal astigmatism. The study results demonstrated a fit success rate of 95% with a significant reduction in myopia and astigmatism.
Some of the case reports in existence in which authors fit different toric orthokeratology lens designs include:
• A case of a 22-year-old patient, sph -4.25 cyl -3.75x8° OD. The corneal astigmatism (CA) was -3.10x7°, and the lens used had two toric zones: the reverse and the landing zone.19 The reduction of a high CA can be achieved if the reverse zone design allows for a close tangential or alignment in each meridian to properly modulate the hydrodynamic forces, which enables for the flattening of each meridian to establish the orthokeratology effect. In the presented case, at two months post-treatment the CA was largely reduced, and the subjective correction was cyl -0.50Dx8° with UNVA 20/20.
• A case of a 44-year-old patient with a mixed astigmatism in which the cylindrical component was greater than spherical one. The patient presented with sph + 1.00 cyl -2.00x180° OD and sph +1.25 cyl -2.25x180° OS.20 The lens fit on this patient was a hexacurve (i.e., six back curves) design with two back toric zones, dual toric zones and optical and landing zones. Also, the vertical meridian was steeper than the horizontal meridian in the landing zone and vice versa in the optical zone. Three months post-orthokeratology fitting, the subjective correction was sph + 0.50 cyl -0.50x10° (UNVA 20/16) OD and sph+0.25 cyl -1.00x5° (UNVA 20/16) OS.
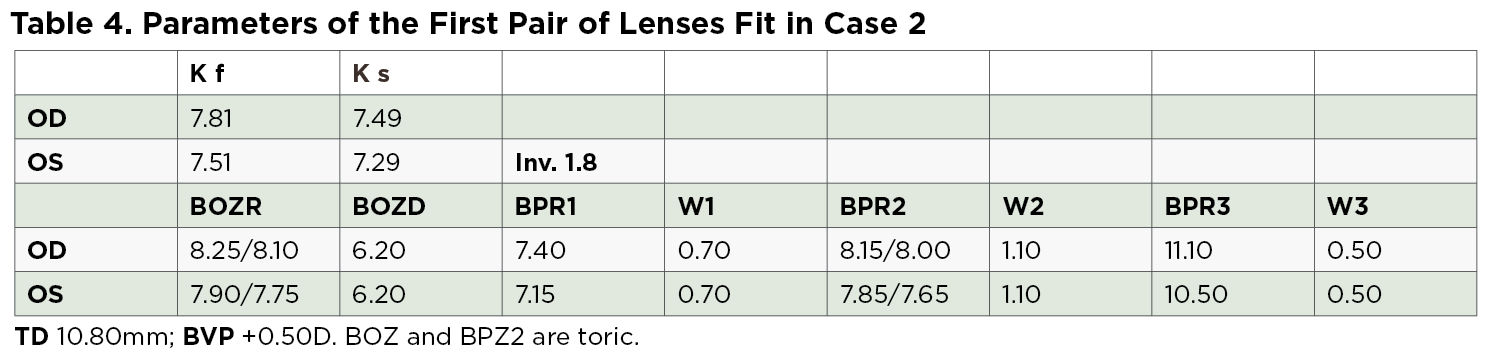
Methods. Because there do not appear to be any set guidelines for toric orthokeratology lens parameter calculation in the literature, indications for spherical orthokeratology lenses were followed instead. The first pair of lenses used demonstrated a tetracurve design with two toric zones—one in the optical zone to correct the astigmatism and another in the landing zone to help achieve a centered lens. Parameters are listed in Table 4.
Fluorescein patterns for this lens fit demonstrated the presence of an upward decentration in the right eye, while in the left eye the pattern was suitable as the BPZ2 was aligned over the corneal peripheral meridians. The spectacle correction was OD sph +1.00 cyl -1.25 x 145°(UNVA 20/32) and OS cyl 1.00 x 40° (UNVA 20/25). Once the treatment effect was underway in the left eye, the design was maintained via flattening of the BOZ by 0.2mm in the horizontal meridian.
 | |
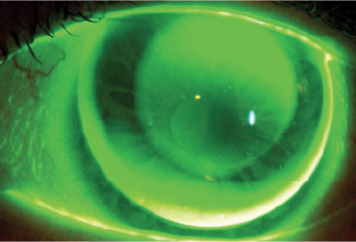
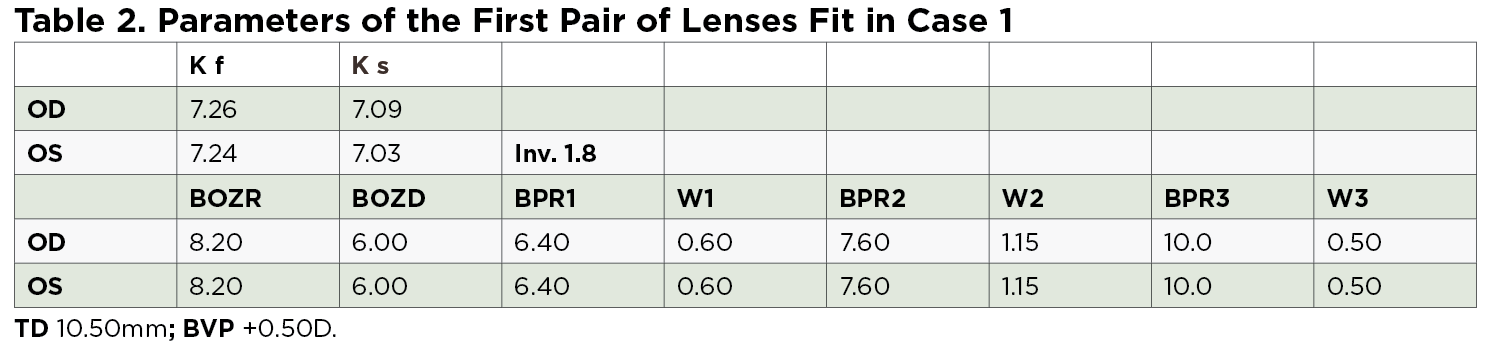
| Fig. 4. Fluorescein patterns of the third pair of lenses, 20 days post-orthokeratology. In this instance, the lenses were centered. | |
 | |
| Fig. 5. Corneal topographies after removing the third pair of lenses. |
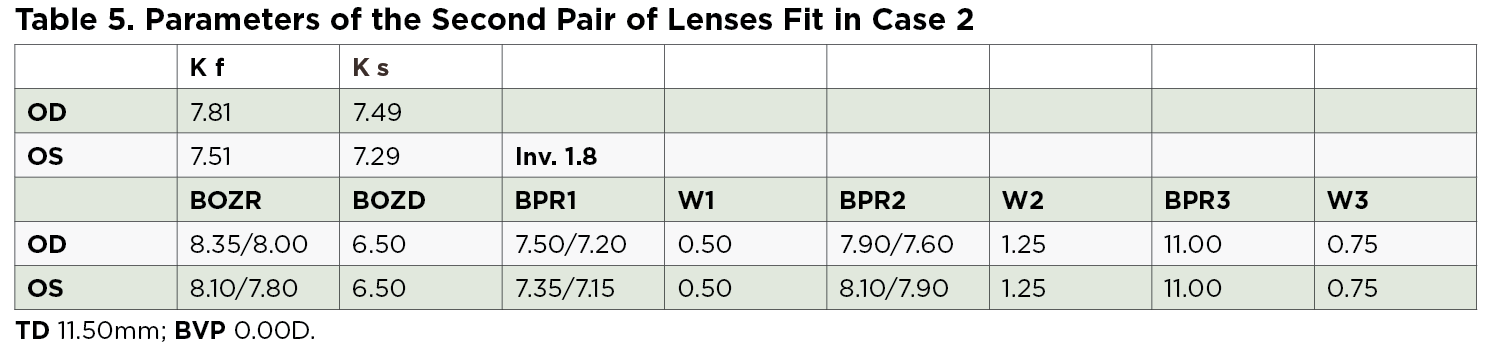
The second pair of lenses was calculated and a tetracurve lens with three toric areas—the optical zone, the reverse zone and the landing zone—was selected based on the residual refraction with the first lenses (Table 5). Fluorescein patterns and corneal maps post-fit demonstrated lens decentration in both eyes, leading to poor refractive results and visual acuity (Figure 3). Parameters were sph +1.00 cyl -1.25x145°(UNVA 20/32) OD and cyl -1.00x40° (UNVA 20/25) OS.
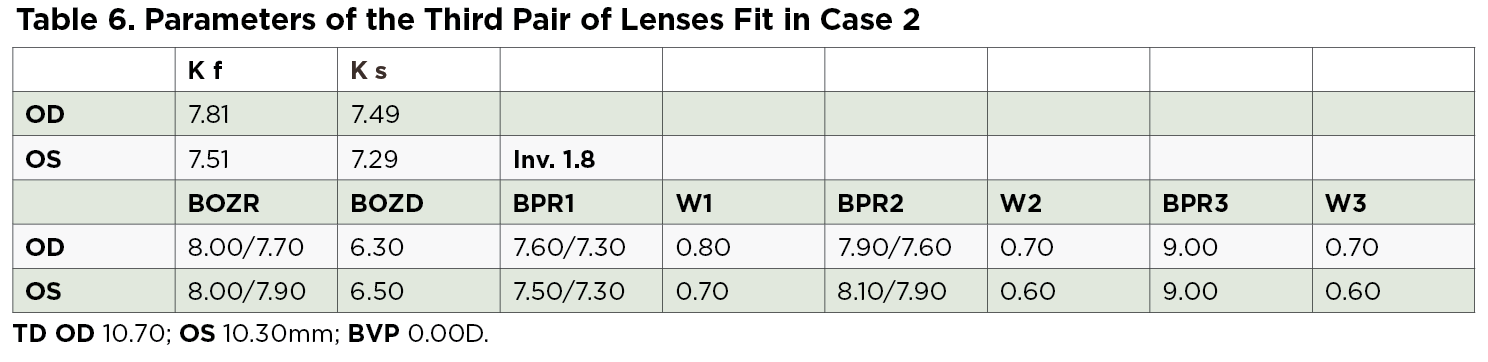
Next, a third pair of lenses was ordered; the parameters are shown in Table 6. It should be noted that the majority of new lens parameters do not necessarily respect the indication reported in literature for spherical orthokeratology lenses. For example, the width of the reverse zone (W1) was larger than the landing one (W2) to achieve a greater hydrodynamic force action, allowing a higher closing lens in each meridian to increase the effect of orthokeratology. For the lens stability, it was decided that the BPZ2 should be flatter than K. In this case, the BPZ3 was steeper than most literature indications to allow for a tear exchange, and the width of the third peripheral zone (W3) was the same as W2 to help balance corneal touch around all meridians.
Results. Twenty days post-treatment, the fluorescein patterns looked good, with regular and constant (real or apparent) touch in all the corneal meridians (Figure 4). The corneal profile post-orthokeratology is shown in the corneal maps (Figure 5). The subjective correction was cyl -0.75x150° (UNVA 20/16) OD, cyl -0.50x30° (UNVA 20/16-1) OS and UNOU 20/16. The patient demonstrated good UNVA for more than 13 hours a day. Additionally, topoaberrometry showed that corneal higher-order aberrations were not relevant except the spherical ones, which allowed the patient to have a good VA at different distances and hence setting up close.
The slit lamp examination showed instability of the tear film in both eyes but the patient reported no presence of symptoms throughout the day.
Discussion. As seen before, in the published studies, conference abstracts and case reports, there are a number of designs of toric contact lenses to treat astigmatism that work equally well.13-21 This second case was solved using a four-toric zone reverse lens, even if it was an apparently contraindicated scenario for this type of lens. In fact, the cylindrical component in the OD was three times larger than the spherical one, while in the OS they were equal. Also there was a refractive astigmatism (OD -2.50D, OS -1.50D) higher than CA (OD -1.82D and OS -1.39D) and a low eccentricity. The parameters of the back curve were then calculated manually.
Though FDA approval criteria states that orthokeratology is appropriate for myopia correction up to -6.00D, there is enough evidence to suggest that orthokeratology also has function for higher myopia and astigmatism. As such, the orthokeratology fitting process in these instances could be made easier with the knowledge of all the lens’ back surface parameters. It enables the contact lens practitioner to become more familiar with the functionality of each parameter so that it can easily be changed to further improve the lens fit. These cases also suggest that a “simple” tetracurve lens could be considered as an option to resolve complex cases as well.
 |
 |
 |
 |
 |
 |
Dr. Fadel specializes in fitting contact lenses for the irregular cornea as well as in scleral lens fittings and orthokeratology. She has a contact lens private practice in Italy where she designs special customized contact lenses. She lectures and publishes especially on the aforementioned subjects. She can be reached at [email protected].
1. Chetty E, Jackson S, Mitton C, Phillips TK. A look at important issues regarding safe orthokeratology. The South African Optometrist, December 2007.
2. Morgan PB, Woods CA, Tranoudis IG, Helland M. International contact lens prescribing in 2014. Contact Lens Spectrum 2015 January; 30: 28-33.
3. Morgan PB, Woods CA, Jones D, et al. International contact lens prescribing in 2012. Contact Lens Spectrum 2013 January; 28: 31-44.
4. Luk BMW, Bennett ES, Barr JT. Fitting orthokeratology contact lenses. Contact lens Spectrum 2001 October, 16(10):22-32.
5. Jessen GN. Orthofocus techniques. Contacto 1962; 6(7):200-204.
6. Chan B, Cho P, Mountford J. The validity of the jessen formula in overnight orthokeratology: a retrospective study. Ophtalmic Physiol Opt 2008 May;28(3):265-268.
7. Swarbrick HA. Orthokeratology review and update. Clin Exp Optom 2006; 89; 124-143.
8. Mountford J, Ruston D, Dave T. Orthokeratology. Principles and Practice. London, Butterworth-Heinemann, 2004.
9. Mountford J. Orthokeratology. In Phillips AJ & Speedwell L. Contact lenses. Edinburgh, Butterworth-Heinemann. 2007:423-450.
10. Joe JJ, Marsden HJ, Edrington TB. The relationship between corneal eccentricity and improvement in visual acuity with orthokeratology. J Am Optom Assoc 1996; 67:87-97.
11. Lui WO, Edwards MH. Orthokeratology in low myopia. Part I: efficacy and predictability. Contact Lens Anterior Eye 2000;23:90-99.
12. Van der Worp E, Ruston D. Orthokeratology: an update. Optom in Practice 2006;7:47-60.
13. Paunè J, Gardona G, Quevedo L. Toric double reservoir contact Lens in orthokeratology for astigmatism. Eye Contact Lens 2012;38:245-251.
14. Chen C, Cheung SW, Cho P. Myopia control using toric orthokeratology. Invest Ophthalmol Vis Sci 2013; 54: 6510-6517.
15. Chen C, Cho P. Toric orthokeratology for high myopic and astigmatic subjects for myopic control. Clin Exp Optom 2012;95:103–108.
16. Beerten R, Christie C, Sprater N, Ludwig F. Improving orthokeratology results in astigmatism. Poster presented at the Global Orthokeratology Symposium, Chicago, IL, July 29–31, 2005.
17. Baertschi M. Short and long term success with correction of high astigmatism in OK. Poster presented at the Global Orthokeratology Symposium, Chicago, IL, July 29–31, 2005.
18. Chan B, Cho P, de Vecht A. Toric orthokeratology: a case report. Clin Exp Optom 2009;92:387–391.
19. Baertschi M, Wyss M. Correction of high amounts of astigmatism through orthokeratology. A case report. J Optom 2010;3:182-184.
20. Calossi A. Mixed astigmatism treated with a Dual-Toric ortho-k design. Contact Lens Spectrum 2013, February;28:49.
21. Jackson JM. Advanced corneal reshaping for astigmatism. Contact Lens Spectrum 2013, February;28:42.
22. Ruston D, Van Der Worp E. Is ortho-K ok? Optometry Today 2004; Dec 17:25-32.
23. Chen CC, Cheung SW, Cho P. Toric orthokeratology for highly astigmatic children. Optom Vis Sci 2012; 89:849-855.
24. Mountford J, Pesudovs K. An analysis of the astigmatic changes induced by accelerated orthokeratology. Clin Exp Optom 2002; 85:284–293.
25. Cheung SW, Cho P, Chan B. Astigmatic changes in orthokeratology. Optom Vis Sci 2009;86:1352–1358.
26. Chan B, Cho P, Cheung SW. Orthokeratology practice in children in a university clinic in Hong Kong. Clin Exp Optom 2008;91:453–460.
27. Van der Worp E. Correcting astigmatism with orthokeratology. Contact Lens Spectrum 2006 July, 21(7):21.


