Although the eye care community has well over 100 years of experience in studying, fitting and observing contact lenses, our understanding continues to evolve in the face of new findings and theories. Lid wiper epitheliopathy (LWE), first described in 2002, has since attracted considerable attention among researchers and clinicians in the dry eye world—especially as it challenges conventional notions of diagnosis and management.1 And it may underlie some of the factors that degrade the on-eye performance of contact lenses and threaten to reduce patient satisfaction.
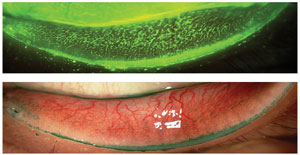
The lid wiper (LW) region is the portion of the marginal conjunctiva of the upper and lower eyelid that acts as a wiping mechanism to spread the tear film over the ocular surface or, if present, a contact lens (CL). LWE describes a disturbance to the epithelium of the lid wiper region and is observed through vital staining of the upper and lower lid margin regions that are in contact with the ocular surface or CL (Figures 1 and 2).
Lid Margin Up Close
The eyelid margin is divided into three regions: (1) the skin epidermis that extends over the meibomian gland orifices, (2) the mucocutaneous junction, which represents the line of Marx, and (3) the lid wiper region.2 The wiper region in the upper lid is the palpebral marginal conjunctiva in contact with the ocular surface. This area, about 1mm in height, ranges from the crest of the sharp posterior lid border to the sub-tarsal fold superiorly and from the upper punctum to the lateral canthus horizontally (Figure 3).1,3 It is wider in the nasal and temporal regions compared with the center of the eyelid.2
 |
| Fig. 1. Lid wiper staining extending from the nasal to the canthal area of the upper lid margin (Top: sodium fluorescein. Bottom: lissamine green.) Photos: Jalaiah Varikooty, Centre for Contact Lens Research. |
 |
| Fig. 2. Lid wiper staining extending from the nasal to the canthal area of the lower lid margin (Top: sodium fluorescein. Bottom: lissamine green.) Photos: Jalaiah Varikooty, Centre for Contact Lens Research. |
The conjunctiva of this region contains goblet cells that secrete soluble mucins onto the surface of the LW. These mucins and other components of the tear film form a hydrated gel between the LW and the ocular surface, providing lubrication and keeping the lid and the ocular surface separated. Impression cytology of the LW region shows the presence of goblet cells, mucins, cell nuclei and various degrees of pre- and parakeratinization.4 Researchers also found metabolic activity, compromised cell membranes, nucleic acids and apoptosis in cells stained with calcein AM, ethidium and annexin V dyes.4
Upper vs. Lower LWE
The primary hypothesis for the cause of LWE is increased friction between the LW and ocular or CL surface due to inadequate lubrication, leading to inflammation and epithelial compromise.
Researchers proposed that the lower lid wiper makes blink-related movements on a much smaller scale than the upper lid wiper and, as a result, has less opportunity to suffer friction-related damage; any epitheliopathy observed may more likely be due to hyperosmotic changes.5 Although the upper eyelid wiper has captured the most attention of researchers—likely due to the large, sweeping movements it makes—the upper lid typically glides over a vast expanse of generally well-lubricated ocular surface. In fact, the frictional effects that cause LWE may be expressed more explicitly in the lower eyelid than the upper.
Investigators evaluated the prevalence and type of lid margin staining and found that LWE is seen in 25% of a population presenting to an eye clinic.14 Others examined LWE in non-CL wearers, soft CL wearers and rigid CL wearers and found that the prevalence and mean grade of lower LWE was significantly higher than that of upper LWE in non-lens wearers. LWE (both upper and lower) was detected in a higher percentage of CL wearers than in non-lens wearers.15
Researchers examined images of upper eyelid wiper staining of non-CL wearers, including the area of the line of Marx in the measurement of lid wiper staining area.16 They also measured the tarsal length, height and area of the tarsal plate in these subjects, but found none of these measures correlated with the area of lid wiper staining. Another study found no difference in the severity of LWE between current CL wearers, previous CL wearers and non-lens wearers.17
Testing
Researchers use a variety of staining methods to examine the lid wiper region, including sodium fluorescein (NaFl), lissamine green (LG), fluorescein and rose bengal (RB), fluorescein and LG and a combination of fluorescein, LG and RB.1,6 However, lissamine green has been the dye of choice for visualizing LWE over the past three years, likely due to the ease of visualization without any barrier filter. Researchers have moved away from RB because of its relatively greater toxicity profile.
When NaFl is used to visualize LWE, a Kodak Wratten 12-barrier yellow filter (transmitting above 495nm) is employed to enhance the view. The slit lamp beam is set to maximum width and 10mm height, and the potentiometer is set to provide maximum illumination through the Wratten 47 or 47A cobalt blue exciter filter.
Clinicians can use both subjective and objective/automated techniques to grade the severity of LWE. Subjective grading—the first and most frequently used system—is based on the appearance of the lid wiper following instillation of vital dyes. Severity of LWE is graded for each eye on a scale of 0 to 3 or 0 to 4 on the basis of the horizontal and vertical extent of lid margin staining with NaFl, LG or RB vital stains.7,8
Investigators graded on a 0 to 3 subjective scale (0=none, 1=mild, 2=moderate, and 3=severe, using 0.5 steps).9 Others used LG to grade the severity of LWE in 0.5 steps using a 4-point simplified pictorial severity grading scale (0=none and 3=severe).10
Research reports the length of the band of staining while grading LWE (Figure 1), and some report more complex patterns of staining including fimbriated or feathery extensions from the superior margin of the subtarsal fold onto the upper tarsal plate.1,7,11 A recent study of silicone hydrogel CL wearers shows six patterns of upper lid margin staining (in addition to no staining): vertical streaks, short horizontal band, broad horizontal band, speckled appearance, comb-shaped and atypical appearance.11
Due to growing interest in understanding LWE, researchers have developed automated grading methods to assess LWE, but they are mainly used for research purposes. Two recently developed methods of automating grading of LW staining involve digital image capture of the stained lid wiper followed by image analysis.12,13 While these techniques are novel and useful in determining the severity and extent of LWE, they are neither quick nor clinician-friendly.
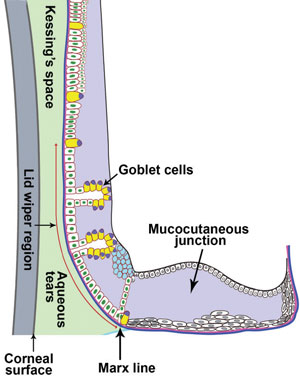 |
| Fig. 3. Representation of histology of the lid wiper region. Vertical width of the lid wiper region is indicated by the red line. |
Friction, CL Wear and LWE
Measuring friction under the human eyelid during blinking is complicated. Tear film components, including proteins and lipids, are attracted within the first few minutes of CL insertion.18 This deposition alters surface properties of the lens material, significantly impacting lid/CL interaction. Studies suggest CL frictional properties may also be associated with LWE and lid parallel conjunctival folds (LIPCOF).19, 20 Thus, measuring the coefficient of friction (COF) over CLs has attracted interest among researchers. COF can be measured by different techniques such as microtribometry, inclined plane method or atomic force microscopy.21-23 The recent TFOS report on contact lens discomfort indicates that COF is the only CL material property that correlates with discomfort.24
COF values can vary depending on technique and testing conditions, and there is no standardized method to assess COF. It is therefore vital to be cautious when interpreting results presented in the literature. Researchers have made significant advances in trying to develop models that mimic on-eye conditions, and further research is warranted in understanding the role of friction, LWE and CL wear.
What we do know for sure is that a lubricious ocular surface is essential to minimize friction. Switching to a lens with high surface lubricity may decrease LWE associated with CL wear. Research shows that contact lenses have a wide range of surface lubricity values.21 One study demonstrates that lenses with higher lubricity values are likely to be more comfortable.25 However, no studies to date have demonstrated a link between CL surface lubricity and LWE. Other management strategies under investigation include altering lens wear modalities, using lubricant drops and improving blinking behavior.
Correlation or Causation?
Although the relationship between LWE and symptoms of dryness or discomfort in CL wearers has been widely studied, the literature is inconsistent in demonstrating a link between LWE and CL-associated dryness and discomfort. For every publication that has found LWE to be greater in CL wearers, another one has found no differences. These inconsistencies could be due to low sample size, recording inconsistencies (time of day, length of lens wear), or insensitive techniques for assessing LWE, comfort or dryness. Any of these factors may have confounded the capacity to detect differences or associations.
Lid wiper epitheliopathy is a condition seen in both contact lens wearers and non-wearers, as well as asymptomatic and symptomatic individuals. Future studies are warranted to understand its cause, nature (i.e., acute or chronic), time of development, diurnal variation and long-term effects.
Dr. Srinivasan is a research assistant professor and a clinical research manager at the Centre for Contact Lens Research (CCLR), School of Optometry and Vision Science, University of Waterloo, Canada. She is actively involved in various clinical trials conducted at the CCLR. Dr. Srinivasan graduated from the Elite School of Optometry, India, obtained her PhD in vision science from the University of Waterloo in 2008 and did her postdoctoral fellowship at the Ohio State University College of Optometry. Dr. Srinivasan is a fellow of the American Academy of Optometry as well as a Scientific Program Committee member. She is also a member of the Association for Research in Vision & Ophthalmology and the International Society for Contact Lens Research.
1. Korb DR, Greiner JV, Herman JP, et al. Lid-wiper epitheliopathy and dry-eye symptoms in contact lens wearers. CLAO J. 2002;28:211-16.2. Knop E, Knop N, Zhivov A, et al. The lid wiper and muco-cutaneous junction anatomy of the human eyelid margins: an in vivo confocal and histological study. Journal of Anatomy. 2011;218:449-61.
3. Knop N, Korb DR, Blackie CA, Knop E. The lid wiper contains goblet cells and goblet cell crypts for ocular surface lubrication during the blink. Cornea. 2012;31:668-79.
4. Muntz A, van Doorn K, Subbaraman LN, Jones LW. Impression cytology of the lid wiper area. Investig Ophthalmol Vis Sci. 2015;56:ARVO E-Abstract 4432.
5. McMonnies CW. An examination of the relationship between ocular surface tear osmolarity compartments and epitheliopathy. The Ocular Surface. 2015;13:110-7.
6. Korb DR, Herman JP, Finnemore VM, et al. An evaluation of the efficacy of fluorescein, rose bengal, lissamine green, and a new dye mixture for ocular surface staining. Eye & Contact Lens. 2008;34:61-4.
7. Korb DR, Herman JP, Greiner JV, et al. Lid wiper epitheliopathy and dry eye symptoms. Eye & Contact Lens. 2005;31:2-8.
8. Willis T, Blackie CA, Korb D. Meibomian gland function, lid wiper epitheliopathy, and dry eye symptoms. Ophthalmol Vis Sci. 2011;52:ARVO EAbstract 3740.
9. Stahl UG, Delaveris A, Madigan M, Jalbert I. Lid wiper epitheliopathy: exploring the links to comfort and osmolality in contact lens wear. Contact Lens Ant Eye. 2011:(Suppl. 1):34.
10. Jalbert I, Rejab S. Increased numbers of Demodex in contact lens wearers. Optom Vis Sci. 2015;92:671-8.
11. Varikooty J, Srinivasan S, Subbaraman L, et al. Variations in observable lid wiper epitheliopathy (LWE) staining patterns in wearers of silicone hydrogel lenses. Contact Lens & Anterior Eye: The Journal of the British Contact Lens Association. 2015;38:471-6.
12. Varikooty J, Lay B, Kier N, et al. The relationship between clinical grading and objective image analysis of lid wiper epitheliopathy. Invest Ophthalmol Vis Sci. 2013;54:ARVO E-Abstract 5460.
13. Kunnen CK, Lazon De La Jara P, Holden BA, Papas EB. Automated assessment of lid margin lissamine green staining. Invest Ophthalmol Vis Sci. 2014;55:ARVO E-Abstract 1976.
14. Guillon M, Maissa C. Assessment of upper and lower lid margin with lissamine green. Optom Vis Sci. 2008;84:E-abstract 80088.
15. Shiraishi A, Yamaguchi M, Ohashi Y. Prevalence of upper- and lower-lid-wiper epitheliopathy in contact lens wearers and non-wearers. Eye & Contact Lens. 2014;40:220-4.
16. Navascues-Cornago M, Maldonado-Codina C, Gupta R, Morgan PB. Characterization of upper eyelid tarsus and lid wiper dimensions. Eye & Contact Lens. 2016 Sep;42(5):289-94.
17. Alghamdi WM, Markoulli M, Holden BA, Papas EB. Impact of duration of contact lens wear on the structure and function of the meibomian glands. Ophthalmic & Physiological Optics. 2016;36:120-31.
18. Bontempo AR, Rapp J. Protein and lipid deposition onto hydrophilic contact lenses in vivo. CLAO J. 2001;27:75-80.
19. Berry M, Pult H, Purslow C, Murphy PJ. Mucins and ocular signs in symptomatic and asymptomatic contact lens wear. Optom Vis Sci. 2008;85:E930-938.
20. Pult H, Purslow C, Berry M, Murphy PJ. Clinical tests for successful contact lens wear: relationship and predictive potential. Optom Vis Sci. 2008;85:E924-929.
21. Roba M, Duncan EG, Hill GA, et al. Friction measurements on contact lenses in their operating environment. Tribol. 2011;Lett. 44:387-97.
22. Tucker RC, Quinter B, Patel D, et al. Qualitative and quantitative lubricity of experimental contact lenses. Invest Ophthalmol Vis Sci. 2012;53:ARVO E-Abstract 6093.
23. Kim SH, Marmo C, Somorjai GA. Friction studies of hydrogel contact lenses using AFM: non-crosslinked polymers of low friction at the surface. Biomaterials. 2001;22:3285-94.
24. Jones L, Brennan NA, Gonzalez-Meijome J, et al. The TFOS International Workshop on Contact Lens Discomfort: report of the contact lens materials, design, and care subcommittee. Invest Ophthalmol Vis Sci. 2013;54:TFOS37-70.
25. Coles CML, Brennan NA. Coefficient of friction and soft contact lens comfort. Optom Vis Sci. 2012;88:E-abstract 125603.


