Soft contact lenses come with myriad benefits and have served our patients well for over four decades. With a wide range of new designs and materials, expanded prescription ranges and customization options, we can achieve great comfort and vision in many more patients than in the past. Toric soft lenses have improved greatly in recent years, expanding the pool of soft contact lens wearers. But where do you turn for astigmatic patients who have not been successful with any soft lens options you have tried? Scleral lenses may provide the solution for practitioners who feel they’ve run the gamut with soft lens options.
Candidates for Scleral Lenses
Ideal candidates include any patient with an irregular corneal surface. This includes patients with keratoconus, pellucid marginal degeneration, post-penetrating keratoplasty (post-PKP), corneal scarring, irregularities following refractive surgery and ocular surface disorders. My experience has shown that patients with these conditions are most appreciative of the benefits that accompany scleral lenses. For some patients, fitting sclerals may eliminate or delay the need for corneal transplant surgery.1,2
In addition, patients with ocular surface disease report less dryness when wearing scleral lenses.3,4 In cases of ocular surface disease or persistent epithelial defects, scleral lens wear can facilitate healing and long-term corneal health, as they help maintain a smooth, wet and protected corneal surface.
 |
| Fitting scleral lenses isn’t a high-tech endeavor; all you need is a diagnostic lens fitting set, slit lamp and phoropter. Photo: Christine Sindt, OD. |
Finally, sclerals are a great option for patients with otherwise healthy corneas who have very high prescriptions (high myopia, high hyperopia and high astigmatism). The gas permeable (GP) optics of scleral lenses provide excellent vision because they center well, have minimal movement and are not dependent on rotational orientation to correct astigmatism.
Benefits for Astigmats
More often than not, my patients with irregular corneas love scleral lenses. Irregular cornea patients who have switched from corneal GP lenses to sclerals report improved comfort, longer wearing time and better visual acuity.5 Here are five benefits scleral lenses can provide to your irregular cornea patients:
Visual acuity. Scleral lenses provide excellent visual acuity due to the inherent stability and customization possible with GP lens optics.6 Rigid materials create a new front surface for the eye by positioning the tear lens between the scleral lens and the cornea, which corrects astigmatism and irregularities of the corneal surface. One study found keratoconus patients who were fit with scleral lenses had better acuity than when previously measured with corneal GP lenses.7 In patients who have residual astigmatism, scleral lenses can be customized with front toric optics. This astigmatic correction is placed on the front surface of the lens and requires a rotationally stable lens attained via double thin zones or toric peripheral curves. Scleral lenses can also incorporate multifocal designs to provide both distance and near vision for presbyopes. The lenses center well and can be made rotationally stable as described above.
Comfort. With proper fitting, scleral lenses prove to be extremely comfortable. Most people describe the feeling of a properly fit scleral lens as being more comfortable than soft lenses.8 Not only are they often more comfortable, in patients with irregular corneal curvature, scleral lenses also allow patients to wear lenses for longer periods each day compared with soft lenses.9
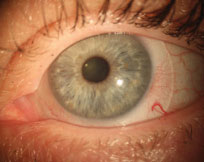
 |
| A decentered corneal GP lens secondary to corneal irregularity. Such a patient may experience a better fit with a scleral lens. |
As practitioners are well aware, lens comfort is a major factor contributing to improvement in our patients’ vision-related quality of life (QOL).8 Studies show higher QOL scores for patients wearing sclerals compared with their previous mode of correction.8,10 In one study of patients who had ocular surface disease, 45 of 49 (92%) reported improved quality of life due to the reduction of photophobia and discomfort.11 During the fitting process, if patients have adverse effects such as lens awareness or discomfort, various changes in lens parameters such as diameter, edge lift, limbal clearance, toric peripheral curves and overall sagittal depth can be modified to make scleral lenses more comfortable. These design changes improve lens comfort by minimizing edge standoff and ensuring the lens has no corneal or limbal bearing. Because of this adaptability, scleral lenses present a good alternative for a wide range of patients.
Performance. Due to their size, scleral lenses do not dislodge with quick eye movements. In addition, airborne particles and dust rarely get under the lens. My clinic sees significantly fewer patients reporting foreign objects beneath their scleral lenses compared with soft lens options. Further, I’ve yet to see a case of lenses dislodging. Both of these factors make sclerals a good option for patients who play sports or lead active lifestyles.
Corneal health. Scleral lenses help maintain a healthy ocular surface.11 Because properly fit sclerals vault the cornea, they maintain a layer of tears that continually bathes the cornea in moisture. In patients suffering from severe dry eye or any ocular surface disorder, scleral lenses provide an ongoing therapeutic effect by keeping the corneal surface protected from trauma, irritation, dehydration and desiccation.12
Delayed surgical intervention. The use of scleral lenses may delay or eliminate the need for corneal transplant surgery.1 If a patient has been unsuccessful with previous modes of contact lens correction, scleral lenses often provide a comfortable, less costly and more convenient solution than surgery, which comes with numerous follow-up visits, long-term eye drop use and a long recovery period.
Learning to Fit Sclerals
Most eye care practitioners already have the skills required to fit scleral lenses. But, at the slit lamp, scleral lens fitters need specific training to know what to look for. Three critical observations are necessary to establish proper fit of a scleral lens:
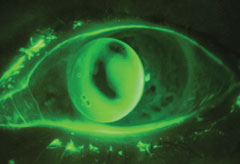
 |
| This well-centered scleral lens shows no edge impingement or scleral compression. Note the continuity of blood vessels under the lens. |
First is central clearance. During diagnostic fitting and evaluation, clinicians must evaluate the thickness of the tear film with an optic section to ensure full corneal clearance, record for future use or give very specific information to a fitting consultant as needed.
Second is evaluation of limbal clearance. Long-term bearing on the limbus will create irritation and redness.
Third is evaluation of the landing profile. The goal is to achieve a uniform, gentle landing 360°. Excessive bearing will show impingement of conjunctival vessels and increasing redness over time, while excessive lift will create increased lens awareness.
Numerous resources can help you learn the necessary skills to gain confidence in fitting scleral lenses. The Scleral Lens Education Society (www.sclerallens.org) and the GP Lens Institute (www.gpli.info) are both excellent resources. Additionally, wet labs and fitting workshops at national and regional specialty contact lens meetings are a great opportunity to learn general scleral skills in a hands-on setting. It is also worth noting that scleral manufacturers hold dedicated webinars and workshops to help clinicians gain experience with a specific design.
Not for Every Patient
While part of the appeal of scleral lenses is the wide range of patients for whom they prove successful, there are some exceptions. A few patient characteristics may be contraindications for scleral lenses:
• If, for example, you have a patient with a very small palpebral fissure with deep-set orbit, sclerals may not be the best option. These anatomical factors can make application of the lens difficult for patients.
• Most patients, even those with small eyes, can be taught to competently apply and remove scleral lenses. We do, however, occasionally come across a patient who just can’t do it and finds repeated attempts too frustrating to tolerate.
• Patients with low endothelial cell counts (<800 cells/mm2) represent another contraindication for scleral lenses. This can occur with various corneal conditions but must be carefully evaluated in post-PKP patients. Patients with low endothelial cell counts who wear scleral lenses are more prone to significant corneal edema and the potential for graft rejection reactions.13
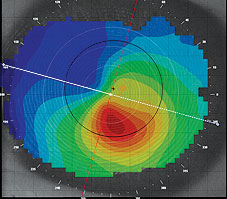
| Case 1 | ||
| A 56-year-old male was referred to me complaining of poor vision in the right eye, although his left eye is fine. He had a history of radial keratotomy in both eyes in 1992 and LASIK in the right eye in 2003. He stated he needed better vision for all activities, but especially for golf. He inquired about additional surgery, glasses or contact lenses. Other practitioners had tried a variety of CL fitting modalities over the past six years. The latest correction was a hybrid lens that provided good vision, but his comfort was not acceptable.
Findings Solution First lens ordered: At one-week follow-up he reported comfortable wearing time of eight hours, but he continued to wear them for a total of about 10 hours a day. He reported his visual acuity as quite good, and he read 20/25 with no distortions. Slit lamp evaluation showed moderate temporal hyperemia, 200 microns of central clearance and slight temporal conjunctival prolapse. I ordered a new lens with a toric landing zone (90 microns flatter in the horizontal meridian with no change vertically). With the new lens, one month later, he reported excellent vision (20/25+), comfortable wearing time of 12 hours a day and only slight and occasional redness. He also reported much better vision on the golf course! |
Although not a contraindication, the presence of pre-existing central corneal scarring will limit the vision-correcting potential of any contact lens—including sclerals. But appearances of scarring can be deceiving, and clinicians should still provide a diagnostic fitting for these patients; scleral lenses may still provide the best potential visual acuity.
Complications
As with any contact lens fitting, complications can occur with scleral lenses.13 Some include corneal neovascularization, limbal injection, corneal/conjunctival infection, corneal staining and corneal edema.
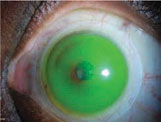
| Case 2 | ||||||
A 29-year-old male was referred to me with a history of keratoconus in both eyes. When he was first diagnosed at 19, he was prescribed corneal GP lenses. He wore those for about five years with varying degrees of comfort. After hearing about new contact lens options for keratoconus, he pursued other modalities over the next five years, including: piggyback, hybrid and special soft lenses. He came in wearing the special soft lenses that provided good comfort, but he complained that vision was not acceptable and that he had to replace them every two months due to deposits. Findings
Solution Diagnostic evaluation for fitting his left eye went well. He was happy with both the vision and comfort with the scleral lenses. I used a prolate back surface design in a 17.0mm lens. Initial diagnostic lens for the left eye: The initial diagnostic lens showed slight central bearing but good limbal clearance and good edge alignment.
The first lens I ordered had 150 microns greater sagittal depth than the diagnostic lens. First lens ordered for the left eye: At one-week follow-up he reported comfortable wearing time of 14 hours and reported not needing to use any lubricating drops. He reported his visual acuity in his left eye as very good, and he read 20/20- with no distortions. Slit lamp evaluation showed minimal hyperemia that did not change with increased wearing time. |
To minimize complications, clinicians should provide a thorough initial fitting evaluation, patient education on proper disinfection and handling techniques, and careful follow-up procedures. In addition, the use of highly permeable materials and special solutions during application can minimize the chance of patients experiencing these complications. These instances, however, are rare and will occur less frequently with increased practitioner experience and confidence.
Fitting your patients with irregular corneas with scleral lenses can be gratifying and is a worthwhile skill set to incorporate into your practice. Scleral lenses can provide comfortable lens wear, clear vision and longer wear time.9 As a practitioner, it is rewarding to hear patients who were unsuccessful in other contact lens modalities report clear vision and an improved quality of life with properly fit scleral lenses. Further, as sclerals are specialty lenses, they can generate greater revenue per patient for your practice from higher fitting fees and enthusiastic word-of-mouth referrals for other specialty patients.
Dr. Lipson is an assistant professor at University of Michigan’s Kellogg Eye Center, Department of Ophthalmology and Visual Science, at the Northville location. His clinical practice involves contact lenses with an emphasis on specialty lenses for overnight corneal reshaping, keratoconus, post-corneal transplant, post-refractive surgery and severe dry eye. He conducts clinical research as the principal investigator for studies on corneal reshaping, vision-related quality of life, myopia control and new lens designs. He lectures nationally and internationally on specialty contact lens and research topics. He is a consultant for Bausch + Lomb’s Specialty Vision Product (SVP) division, specializing in education and training on specialty contact lenses with emphasis on orthokeratology. Dr. Lipson is the vice president of the Scleral Lens Education Society and a fellow of the American Academy of Optometry.
1. Deloss KS, Fatteh NH, And Hood CT. Prosthetic replacement of the ocular surface ecosystem (PROSE) scleral device compared to keratoplasty for the treatment of corneal ectasia. Am J Ophthal. 2014;158:974-82.
2. Severinsky B, Behrman S, Frucht-Pery J, Solomon A. Scleral contact lenses for visual rehabilitation after penetratingkeratoplasty: Long term outcomes. Cont Lens Ant Eye. 2014;37:196-202.
3. Schornack MM, Baratz KH, Patel SV, Maguire LJ. Jupiter scleral lenses in the management of chronic graft versus host disease. Eye Cont Lens. 2008;34(6):302-5.
4. Rosenthal P, Cotter J. The Boston scleral lens in the management of severe ocular surface disease. Ophthalmol Clin N Am. 2003;16:89-93.
5. Segal O, Barkana Y, Hourovitz D, et al. Scleral lenses may help where other modalities fail. Cornea. 2003;22:308-10.
6. Stason WB, Razavi M, Jacobs DS, et al. Clinical benefits of the boston ocular surface prosthesis. Am J Ophthalmol 2010;149:54–61.
7. Schornack MM, Patel SV. Scleral lenses in the management of keratoconus. Eye Contact Lens 2010;36:39-44.
8. Bergmanson JP, Walker MK and Johnson LA. Assessing scleral contact lens satisfaction in a keratoconus population. Optom Vis Sci 2016;93. Epub ahead of print.
9. Ortenberg I, Behrman S, Geraisy W and Barequet I. Wearing time as a measure of success of scleral lenses for patients with irregular astigmatism. Eye Contact Lens. 2013;39:381-4.
10. Visser E-S, Visser R, van Lier H, Otten H. Modern scleral lenses part II: patient satisfaction. Eye Contact Lens. 2007;33:21-5.
11. Romero-Rangel T, Stavrou P, Cotter J, et al. Gas permeable scleral contact lens therapy in ocular surface disease. Am J Ophthal. 2000;130:25-32.
12. Van der Worp E, Bornman D, Ferreira DL, et al. Modern scleral lenses: a review. Cont Lens Ant Eye. 2014;37:240-50.
13. Walker MK, Bergmanson JP, Miller WL, et al. Complications and fitting challenges associated with scleral contact lenses: A Review. Cont Lens and Ant Eye. 2015;39:88-96.