Benefits to Fitting Pediatric Patients
For the adult population, improved cosmesis is one of the most common reasons patients choose contact lenses over spectacles—and the same could be said about pediatric patients. The ACHIEVE study found children wearing contact lenses felt significantly better about themselves in the areas of athletic competence, social acceptance and physical appearance compared with study participants wearing spectacles.1 In children who are not compliant with spectacle wear because of cosmetic concerns, contact lenses can lead to an overall improvement in compliance with refractive correction. This is particularly important for children with significant refractive errors, as contact lenses will increase the field of view particularly well in patients with a high refractive error. Patients with corneal irregularities or high refractive errors may experience improved visual acuity and comfort with contact lenses. Children with significant anisometropia benefit from the decrease in aniseikonia with contact lens wear compared with spectacle wear, which not only decreases asthenopia, but also can improve binocularity.2
Concerns for Clinicians
One of the first concerns that many practitioners have when fitting children in contact lenses is the potential increase in chair time. Contrary to popular belief, fitting a young child does not necessarily take more time than fitting an older child or an adult. The Contact Lens In Pediatrics study found that it takes, on average, only 15 more minutes to fit children age eight to 12 compared with children older than 12.3 Most of this extra time was spent on insertion and removal training, a task that can generally be delegated to staff members. Another notable concern clinicians have in fitting children—particularly younger ones—in contact lenses is the risk of an adverse event. However, younger children are actually less likely to have an adverse event during contact lens wear than teenagers and young adults, and microbial keratitis is uncommon in this population.4
 |
 |
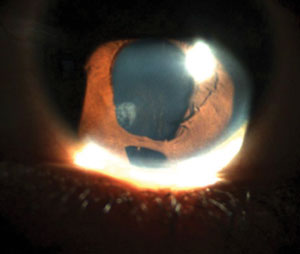
| On top, a custom prosthetic lens decreases the amount of light entering the pupil and the cosmetic appearance of the iris irregularity. Below, an inferior iris coloboma causes increased light sensitivity and haloes around objects. |
Ready or Not (to Wear Contacts)
Determining if a child is ready for contact lens wear is one of the most challenging parts of the fitting process. Although most parents ask at what age we begin fitting contact lenses, the patient’s age is generally not the limiting factor. The pediatric population is not homogeneous, and each patient must be treated individually. While some children as young as seven may prove ready for contact lens wear, some adolescents are not good candidates.
Often to the caregiver’s surprise, the best resource for answering the question of a child’s readiness is the parents or guardians themselves. Questioning parents about the overall responsibility level of the child will help to determine if the child is ready for the responsibility of contact lens wear. Are they able to take responsibility for homework or chores at home? Does the child make their bed every morning and keep a clean room? Will they remember to remove the lenses before bed every night and clean them properly? The parent can also give insight into the child’s personal hygiene, which can impact their ability to properly care for contact lenses.
Both patient and parent motivation is essential to successful lens wear in pediatric patients. If a child is reluctant to wear lenses, it can be challenging to successfully fit them in contact lenses. Similarly, if a parent is reluctant to allow a child to wear lenses, it may be an indication the parent realizes the child is not ready for contact lens wear.
Special Indications
Some pediatric patients who may not be ideal candidates for contact lens wear may, nevertheless, need to be fit in contact lenses to improve vision, comfort or binocularity. The overwhelming benefits of contact lenses over spectacles in these patients may make contact lens wear the best option for the pediatric patient, regardless of the patient’s age. In these cases, parental motivation and support is the key to successful contact lens wear. Children who are aphakic—either from congenital aphakia or from cataract removal at an early age—are often fit in contact lenses as infants or toddlers. Infants and toddlers with extremely high refractive error or high amounts of anisometropia may benefit from contact lens wear to improve acuity and binocularity.
Contact lenses can also be used for penalization therapy in amblyopia, either by overplussing the non-amblyopic eye to cause blur significant enough to switch fixation to the amblyopic eye or using a lens with an opaque pupil to occlude the non-amblyopic eye. When using the plus therapy, the lens-induced blur must be greater than the blur experienced by the amblyopic eye.6
Additionally, tinted lenses can be fit for patients with achromatopsia or other cone dystrophies to decrease photophobia and enhance color perception. Patients with achromatopsia often prefer red, magenta or brown lenses in lieu of wearing tinted spectacles. Although the contact lens tint can be seen under the slit lamp, it is not detectable under normal viewing conditions, providing a more cosmetically appealing option. Colored lenses can decrease photophobia, improve vision and provide better cosmesis for patients with iris abnormalities such as iris coloboma and aniridia.
Pediatric patients with corneal irregularities may experience better vision as well as increased comfort with contact lenses.
 |
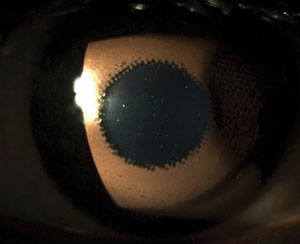
| During a prostehtic lens fitting, contact lenses can be layered to show the patient how the final product may look. Here is an occluded pupil contact lens with a brown underprint layered on top. |
Choosing the Right Lens
Options for fitting children in contact lenses are similar to those with any other age group. Soft lenses are the most commonly used modality for general refractive cases such as myopia, hyperopia and regular astigmatism. Many manufacturers offer extended range parameters for patients with high amounts of myopia and hyperopia, keeping the overall cost to a minimum for the patient and avoiding the need to switch to custom soft lenses.
Daily lenses decrease the likelihood of contact lens-related adverse events. Daily disposables can also be easier for children to handle, eliminating the need for cases and solution bottles.5
Children with aphakia, significant corneal cylinder, irregular corneas or ocular surface disease can be fit with rigid gas permeable lenses, including scleral lenses. When fitting rigid lenses in children, it may be beneficial to use a Burton lamp or a Bluminator for lens evaluation outside of the slit lamp. This allows the child to sit comfortably in a stroller or parent’s lap during the lens evaluation. Prosthetic contact lenses are an option for children with iris or corneal irregularities. These lenses can help decrease photophobia, diplopia or improve cosmesis.
Insertion and Removal
Training in the pediatric population can be slightly more challenging than in adult patients. Parents or guardians should be present to listen to the instructions given to the pediatric patient so the parent also learns about proper contact lens care in case they need to assist the child. This is crucial for children too young to insert and remove the lenses themselves, as the parent will be handling this process for the child.
With every new pediatric patient, there is always an insertion and removal training in-office. For parents of infants and toddlers, clinicians should stress the importance of having a secure hold of the infant’s head and body. Many times, this becomes a two-person effort, as one person holds the infant while the other inserts or removes the contact lens.
 |
 |
| Even with a lighter iris, it’s hard to tell a patient is wearing a tinted contact lens, which help avoid the use of red glasses. |
For children able to insert and remove lenses on their own, clinicians should begin by emphasizing the need to wash your hands before insertion and removal. Generally, the practitioner places the lenses first, so the child will have the lenses in during the fitting process. Therefore, training will entail teaching removal skills first, followed by lens storage and ending with insertion techniques. It is important to guide the child the first time to help increase confidence and then let them do it on their own. This will show them they can do it and indicate they may be ready to take the lens home.
Clinicians should watch the child insert and remove the lenses at least twice before dispensing. This ensures patient and parent have the proper technique and are comfortable with the lenses. If the first training is unsuccessful, stop before the patient and parent become frustrated and have them return to attempt training on a different day.
Laying a towel over the sink drain can help young patients avoid losing lenses, and labeling solution bottles and contact lens boxes and cases carefully can avoid misusing the solution or wearing incorrect lenses.
Compliance
Children are more likely to share their lenses with friends, so it is important to educate them that they cannot do so with anyone else or allow anyone try their lenses on. As with any medical device, compliance is always an issue. A handout that details how lenses are to be worn and the proper care method can help with this. Written instructions that includes the solution names, replacement schedules, wearing time and signs and symptoms of common complications can be extremely helpful. Regardless of age, clinicians should also warn against swimming in lenses, and stress the need to always rub the lenses with solutions, store them with new solution each night and replace the case every three months.
Many pediatric patients can easily and safely use contact lenses, even young children, with proper oversight. Contact lenses can provide improved confidence, better visual acuity, higher levels of comfort and better potential for binocular vision in pediatric patients. Although fitting young children can be intimidating at first, it can be equally rewarding for both the patient and practitioner.
Dr. Jenewein completed a residency in pediatrics and binocular vision at Nova Southeastern University. She is an assistant professor at Salus University Pennsylvania College of Optometry.
Dr. Bhagat is a faculty member at the Pennsylvania College of Optometry at Salus University. She specializes in managing ocular surface disease and fitting specialty contact lenses.
1. Walline J, Jones L, Sinnott L, et al. Randomized trial of the effect of contact lens wear on self-perception in children. Optometry and Vision Science. 2009;86(3):222-32.
2. Winn B, Acherley RG, Brown CA, et al. Reduced aniseikonia in axial anisometropia with contact lens correction. Ophthalmic Physiological Optics. 1988;8(3): 341-4.
3. Walline, J, Jones L, Rah M, et al. Contact lenses in pediatrics (CLIP) Study: chair time and ocular health. Optometry and Vision Science. 2007;84(9):896-902.
4. Wagner H, Richdale K, Mitchell G, et al. Age, behavior, environment, and health factors in the soft contact lens risk survey. Optometry and Vision Science. 2014;91(3):252-61.
5. Chalmers RL, Hickson-Curren SB, Keay L, et al. Rates of adverse events with hydrogel and silicone hydrogel daily disposable lenses in a large postmarket surveillance registry: the TEMPO Registry. Invest Ophthalmol Vis Sci. 2015;56(1):654-63.
6. Walline J, Rah M. Contact lenses for amblyopia Treatment. Contact Lens Spectrum. 2008. Available at www.clspectrum.com/issues/2008/november-2008/treatment-plan. Accessed January 17, 2017.


