The ocular surface is part of a complex network of mucous membranes spread throughout the body. While membranes exhibit similar essential characteristics, each has its own unique attributes as well. For example, the mucous membrane of the nose and throat produces significant quantities of mucus to help enable the capture of airborne pathogens. Cilia then move the contaminated mucus upward, where it is expelled through the nose and mouth.
The eye is no exception to this, possessing a specialized epithelium that maintains and protects the ocular surface. However, because of the tremendous sensory advantage the eye’s external structures gives an individual, the conjunctival and corneal epithelium is also exposed to an almost constant environmental assault—more so than any other mucous membrane. Environmental toxins, ambient humidity and allergens in the environment are some of the assailants that must be defended against. This article discusses their effects and methods of patient management.1,2
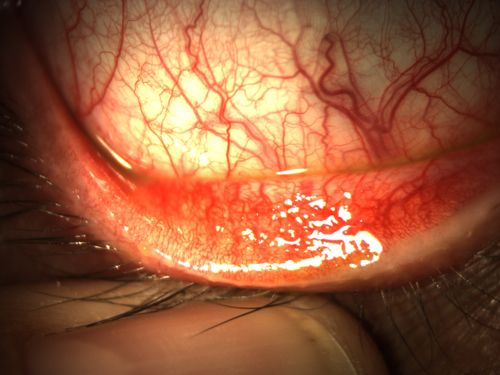 | |
| Fig. 1. Hyperemia and papillary response of the conjunctiva in seasonal allergic conjunctivitis. |
Humidity
Low ambient humidity can have a significant effect on the tear film evaporation and evaporative dry eye.3 Geographic considerations for humidity vary not only with local weather patterns and with altitude. Humidity levels vary both with local weather patterns and altitude: as such, patients located in different areas of the vast and varied geographic makeup that comprises the United States may be affected differently. For example, as altitude increases, air pressure decreases, reducing the amount of water vapor the air can hold. Temperature has the inverse relationship, with air of a higher temperature able to contain more water than that of a colder temperature.
The importance of ambient humidity is often overlooked in patients with dry eye symptoms for one reason: it’s a local environmental factor that remains relatively consistent from day to day. Thus, it often fails to even register as an external influence. However, a factor that is easily augmented in both the home and work environments with commercially available humidifiers, which come in two basic varieties: heated and cool-mist. Heated humidifiers produce warm steam and are highly effective at quickly modulating indoor humidity. Cool-mist humidifiers, in contrast, use ultrasonic pulses to create water vapor. While not as effective as heated humidifiers, they are less likely to raise the temperature of the room or cause water to condensate on the walls.
Environmental Toxins
Chemical or irritative conjunctivitis may develop in response to significant irritation brought on by environmental toxins. These include smoke, chlorine in swimming pools, air pollution and volatile organic compounds.4,5 Effective treatments include limiting exposure to the offending chemical, if possible, increasing local ventilation and washing remaining toxins away from the ocular surface. In extreme cases this may require lavage, but generally frequent use of nonpreserved artificial tears is sufficient and will not only help clear the toxin, but also help soothe the ocular surface.
Allergens
Most common environmental irritants are not toxic in and of themselves; rather, the human body’s inappropriate inflammatory response to them, known as allergy, is what results in discomfort. The word antigen is derived from the word antibody and the Greek suffix -gen, meaning “that which induces production” of something (in this case, antibodies).
Antigens are not limited to triggering allergic reactions; rather, they encompass anything the immune system reacts to. This can be virtually anything in the environment that is not essential for life.
The subcategory of infectious antigens is comprised of proteins and molecules produced by various microorganisms, while allergic antigens are innocuous substances that pose no threat to the health of the individual, yet elicit an inappropriate immune response. For example, pollens responsible for the mating and fertilization of different plants are not harmful if inhaled, but can be responsible for triggering an allergic response. Other common environmental allergens include mold, pet dander and dust mite feces.6
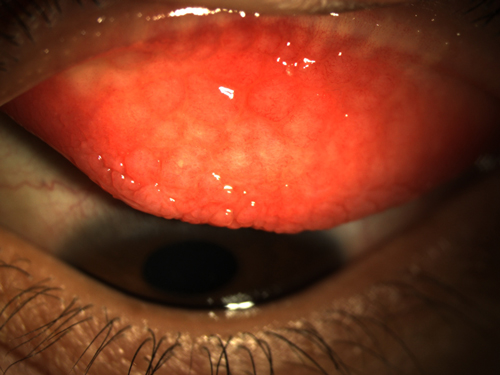 | |
| Fig. 2. Giant papillae in atopic keratoconjunctivitis. |
When considering the pathophysiology of allergy and allergic eye disease, it is crucial to understand some fundamental key concepts. First and foremost is the recognition that, at the cellular level, allergic responses are essentially initiated the same way no matter where they occur in the body. From an immunology standpoint, key players in the allergic response to environmental allergens include T-cells and the action of mast-cell degranulation that produces the symptomatology we are familiar with.
To adequately counteract any potential threats and protect the body, the human immune system must be prepared to halt anything it perceives as threatening, even though it may not know what it might encounter. A newborn infant’s immune system is considered the most naïve in that it has not encountered much prior to exiting the womb. After birth, however, it is immediately subjected to an onslaught of antigens. Each initial encounter may trigger the development of an immune response, known as T-cell priming and sensitization. If the response is to an antigen that poses no threat to the individual, it is then, by definition, allergic. It can take 10 to 14 days to set the stage for an initial allergic response.7
During subsequent encounters, when the T-cell encounters the allergen, it communicates with B-cells to mass-produce IgE subtype antibodies—Y-shaped proteins that tightly bind to the antigens they are indicated for upon an encounter. Once created, these antibodies are released from the B-cells into the bloodstream, where they locate mast cells that reside in superficial layers in the skin and mucosa. These mast cells include a receptor on their surface that binds to the antibodies and are packed with granules that contain many factors. When an allergen encounters the tethered IgE antibodies, it triggers degranulation, spilling inflammatory factors like histamines into the surrounding tissue.
The release of histamine is responsible for much of the signs and symptoms we observe in allergic eye disease. Upon binding to receptors on nearby blood vessels, they elicit vasodilation and increased the permeability of the nearby vasculature. Vasodilation is responsible for the hyperemic appearance of the conjunctiva characteristic of ocular allergies; this increase in permeability of blood vessels also allows leakage of serum components into the surrounding tissues, causing chemosis. Histamine release also induces significant pruritis, or the moderate to intense itching most commonly associated with allergic conjunctivitis.
Mild to Moderate Ocular Allergy
Simple allergic conjunctivitis can be divided into two primary subtypes: seasonal allergic conjunctivitis (SAC) and perennial allergic conjunctivitis (PAC). Together, SAC and PAC account for 95% of allergic conjunctivitis presentations in the United States.8 While this distinction may suggest they are two different clinical entities, the terms are in fact more descriptive of the timing of onset and types of allergens involved.
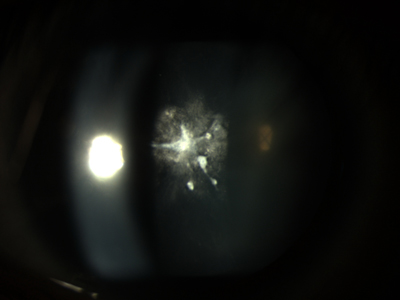 | |
| Fig. 3. Anterior subcapsular cataract in a patient with atopic keratoconjunctivitis. |
Though spring is predominantly thought of as allergy season, different pollens are produced at different times of the year depending upon the plant variety and geographic weather patterns such as average temperature and prevailing winds. As such, certain offending allergens may in fact peak in the summer, fall, winter or even during multiple seasons throughout the year.
Perennial allergic conjunctivitis, in contrast, does not follow seasonal patterns because it involves allergens that do not fluctuate throughout the year; these include mold spores, pet dander and dust mite feces.
Common clinical findings associated with these conditions include chemosis of the bulbar conjunctiva, hyperemia of the bulbar and palpebral conjunctivae and the formation of small papillae on the upper and lower tarsal conjunctiva (Figure 1).9,10 Many patients also report moderate to intense itch and watery or mucoid discharge.
To differentiate between the mucoid discharge in allergic conjunctivitis and the mucopurulent discharge of bacterial conjunctivitis, ask the patient to describe the color and intensity of discharge upon wakening. Discharge from bacterial conjunctivitis tends to be yellowish or greenish in color, and lids are often matted shut upon wakening, while in the case of allergic conjunctivitis, discharge is typically grey or white in color. Discharge from allergic conjunctivitis can also matte the eyelids shut, though this is not as common as in bacterial conjunctivitis. To differentiate between allergic conjunctivitis and viral conjunctivitis—which presents similarly—note the presence of pruritis.
Laterality in allergic eye disease is approached by many clinicians as absolute. There is a misconception that symptoms must be bilateral and symmetric because the response is to a factor that is ubiquitous in the environment, and therefore would cause similar reactions in both eyes. While true overall, there are two scenarios that may lead to a unilateral or asymmetric presentation. The first is that the patient is allergic to something that is not airborne, but rather is transferred to the ocular surface via a vector like the patient’s hand. The second is individuals with an allergy to dust mite feces who regularly sleep on their side.11
Treatment for SAC and PAC is often confined to palliative measures like cold compresses and nonpreserved artificial tears. For patients who require pharmaceutical intervention, however, a non-drowsy oral antihistamine should be used. Allergy sufferers can often achieve relief from multiple allergic conditions. In the case of a patient with significant ocular symptoms who also presents with severe dry eye, try treating with a multimodal antiallergy drop such as ketotifen, olopatadine or alcaftadine.
Moderate to Severe Allergies
The two more severe ocular allergic conditions are atopic keratoconjunctivitis (AKC) and vernal keratoconjunctivitis (VKC). These are chronic allergic inflammatory conditions with acute exacerbations that have severe visual consequences because of the potential for corneal involvement. In addition to findings of simple allergic conjunctivitis, AKC and VKC sufferers often report more discomfort and photophobia. These symptoms can have a profound impact on quality of life.12
Many of the clinical findings associated with AKC and VKC are characteristic of both conditions. Patients typically develop large papillae on the tarsal conjunctiva of the upper lid (Figure 2). Additionally, gelatinous lesions referred to as Horner points or Trantas dots form on the limbus, and a filamentary keratitis is sometimes present. Pseudomembranes can materialize in the lower and upper fornix and should be removed to prevent eventual formation of symblepharon. If left untreated, the corneal epithelium will begin to decompensate, with the potential for shield ulcers that leave the patient open to a higher risk of infection and eventual corneal scarring. Scarring of the upper palpebral conjunctiva from chronic inflammation can lead to shortening of the fornix and corneal scarring secondary to trichiasis.13
Distinguishing AKC from VKC relies on a few key clinical features. VKC typically affects preadolescent to early-adolescent males and may become exacerbated in certain seasons over others. Papillae on the upper tarsal conjunctiva are large, giving the appearance of cobblestones on exam.
AKC, by contrast, has a late adolescence to early adulthood onset and generally does not show a gender predilection. Additionally, though the conjunctival papillary response can be pronounced, it is generally less so than with VKC. Most AKC patients have an associated atopic dermatitis (eczema) on or around the lids, though this is not always the case. One unique feature of AKC is the development of a “polar bear rug” cataract, or an anterior subcapsular cataract with a characteristic appearance that earns its nickname (Figure 3).
Acute episodes of VKC and AKC are typically treated with topical steroids such as loteprednol or prednisolone drops. Due to the multitude of negative side effects, however, long-term steroid use should be avoided. New research suggests that immune modulators like cyclosporin A and tacrolimus may actually be better options for long-term management; however, these treatment options are still experimental and considered off-label.14-16
The environment poses a constant threat to the ocular surface. The key to minimizing its effects is avoidance of the causative environmental agents and using supportive and therapeutic measures when avoidance is not practical or, as is often the case, not possible.
1. Sundbom F, Malinovschi A, Lindberg E, et al. Effects of poor asthma control, insomnia anxiety and depression on quality of life in young asthmatics. J Asthma. 2015 Dec 15:1-17.
2. Bielory L, Skoner DP, Blaiss MS, et al. Ocular and nasal allergy symptom burden in America: the allergies, immunotherapy, and rhinoconjunctivitis (AIRS) surveys. Allergy Asthma Proc. 2014 May-Jun;35(3):211-8.
3. Abusharha AA, Pearce EI. The effect of low humidity on the human tear film. Cornea. 2013 Apr;32(4):429-34.
4. Granet D. Allergic rhinoconjunctivitis and differential diagnosis of the red eye. Allergy Asthma Proc. 2008 Nov-Dec;29(6):565-74.
5. Wieslander G, Norbäck D. Ocular symptoms, tear film stability, nasal patency and biomarkers in nasal lavage in indoor painters in relation to emissions from water-based paint. Int Arch Occup Environ Health. 2010 Oct;83(7):733-41.
6. Lambrecht BN, Hammad H. Allergens and the airway epithelium response: gateway to allergic sensitization. J Allergy Clin Immunol. 2014 Sep;134(3):499-507.
7. Weston WL, Bruckner A. Allergic contact dermatitis. Pediatr Clin North Am. 2000;47(4):897-907, vii.
8. Butrus S, Portela R. Ocular allergy: diagnosis and treatment. Ophthalmol Clin North Am 2005; 18:485–492; v.
9. Bielory L, Friedlaender MH. Allergic conjunctivitis. Immunol Allergy Clin North Am. 2008; 28:43–58; vi.
10. Castillo M, Scott NW, Mustafa MZ, et al. Topical antihistamines and mast cell stabilizers for treating seasonal and perennial allergic conjunctivitis. Cochrane Database Syst Rev. 2015 Jun 1;6:CD009566.
11. Blochmichel E, Helleboid L, Corvec MP. Chronic allergic conjunctivitis. Ocul Immunol Inflamm. 1993;1(1-2):9-12.
12. Zicari AM, Nebbioso M, Lollobrigida V, et al. Vernal keratoconjunctivitis: atopy and autoimmunity. Eur Rev Med Pharmacol Sci. 2013 May;17(10):1419-23.
13. Chen JJ, Applebaum DS, Sun GS, Pflugfelder SC. Atopic keratoconjunctivitis: A review. J Am Acad Dermatol. 2014 Mar;70(3):569-75.
14. Vichyanond P, Kosrirukvongs P. Use of cyclosporine A and tacrolimus in treatment of vernal keratoconjunctivitis. Curr Allergy Asthma Rep. 2013 Jun;13(3):308-14.
15. Tzu JH, Utine CA, Stern ME, Akpek EK. Topical calcineurin inhibitors in the treatment of steroid-dependent atopic keratoconjunctivitis. Cornea. 2012 Jun;31(6):649-54.
16. Al-Amri AM. Long-term follow-up of tacrolimus ointment for treatment of atopic keratoconjunctivitis. Am J Ophthalmol. 2014 Feb;157(2):280-6.


