 |
Congratulations, you have ocular allergies.
Most eye care professionals have never uttered this statement offhand to their patients, but for those with ocular allergy sufferers who may be interested in wearing contact lenses, it’s an important point to consider. Proactively identifying contact lens candidates who may experience allergy-related discomfort gives us the opportunity to turn a possible negative into a positive before it becomes a larger issue.
Treating current lens wearers’ ocular allergies will also allow those who are experiencing limited wearing success to more comfortably enjoy the benefits of contact lens wear. Some of these patients may have been told by other eye care professionals that nothing can be done to ease their symptoms and may have resorted to dropping out of contact lens wear during allergy season to avoid discomfort. So, if you are able to offer the possibility of comfortable contact lens wear during allergy season, you may very easily earn yourself a lifelong patient. But, how do you achieve this? Here are some tips to help you manage this unique group of patients.
1. Ask the right questions at the right time. Many practitioners employ technical staff to discuss symptoms with the patient at the beginning of the exam and help administer medication as needed. While patients who present with an ocular infection typically report continual symptoms during the period of infection, patients with ocular allergies may only experience symptoms during certain times of the year—which may not be during the time of their exam. These patients often neglect to mention their allergies when discussing their eye history for the simple reason that it slips their mind, so tailor your symptom questionnaire to catch them even during the offseason. By asking the right questions, you may be surprised how many allergy sufferers go undiagnosed and untreated in your practice.
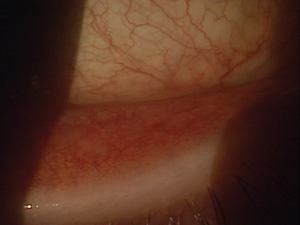 | |
| Fig. 1. Inferior palpebral conjunctival papillae and redness due to ocular allergies. |
Even if the patient indicates no allergy-related discomfort (i.e., their contact lenses become more difficult to wear during certain times of the year, or while in their work environment), make sure to ask follow-up questions during the anterior ocular exam. Peek around the slit lamp and ask, “Do your eyes ever burn, itch or water, or do your eyelids ever swell or turn red?” Look closely for mild eyelid and conjunctival edema and/or redness (Figure 1).
Evert the upper and lower eyelids to reveal the presence of papillae or other complicating factors. These can often be seen more easily when visualized with the use of fluorescein. You can also follow up with, “Do you ever experience intermittent blur with your contact lenses during certain times of the year?” These factors, while not directly related to contact lens comfort, can also be indicative of possible allergies that may eventually lead to lens issues.
2. Address the issue and treat the underlying condition. Patients are often surprised to hear that their allergies are responsible for their issues with contact lens wear, especially if the reaction is mild. Once informed of their diagnosis, however, they are now aware and looking for solutions. Take the appointment a step further by informing them that there are still possible contact lens options.
Daily disposables are one suitable option for patients who suffer from ocular allergies. Because surface allergens do not build up on these daily replacement lenses, patients’ clinical reactions are limited.1 Additionally, there are no compliance issues that could further aggravate a patient’s allergic reaction because a clean lens is placed on the eye each day. If your patients have not heard about these lenses already, this is an ideal time to educate them.
3. Individualize the approach. In some cases, the patient’s contact lens fitting and allergic treatment regimen may collide. This is because the presence of ocular allergies may decrease lens awareness or reduce vision during the fitting, complicating the process. Also, if the patient is using topical steroids throughout the day, lens wear would be contraindicated.
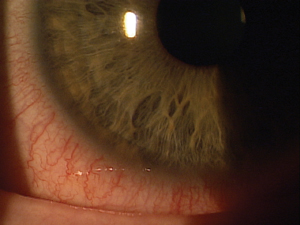 | |
| Fig. 2. Conjunctival injection and chemises from an ocular allergic reaction.
|
This is the time to customize a treatment plan according to the patient’s particular needs. Take a step back and explain to them how their allergic condition may need specific medical attention (and not just an OTC product) and what steps would be required to clear it. For example, they may need to remove their lenses for a period of time, treat the allergic state and then consider other lens options. Be sure to stress that the treatment will help them with symptoms.
Case in Point
A 26-year-old female patient presented complaining of frequent itching and burning. She reported using OTC Visine-A Allergy Relief Drops (Johnson & Johnson) to no relief. She is an IT consultant who has never worn contact lenses because she was informed in the past she could not wear them. During her examination, it was evident ocular allergies were the cause of her issues. Her inferior palpebral conjunctiva was red, inflamed and chemotic in both eyes (Figure 2).
The patient was treated with a topical ocular steroid for two weeks, then moved to a daily antihistamine/mast-cell stabilizer for maintenance. After finishing the steroid eye drops, she was successfully fit into hydrogel daily disposable lenses. This made a huge difference in her ocular irritation, even compared to no contact lenses. She had less allergic symptoms throughout the day, and she enjoyed the convenience her new daily contact lenses provided.
Above all, the challenge with current contact lens wearers and allergy sufferers is identifying allergies as the underlying cause of symptoms. Many eye care professionals look to place the “blame” on their patient’s current contact lenses. Instead, consider identifying and treating any underlying conditions prior to a successful contact lens fit.
1. Stiegemeier M, Thomas S. Seasonal allergy relief with daily disposable lenses. Contact Lens Spect. 2001:April;16(4):24-8.


