 |
If, after examining the patient, you can’t think of a reason it’s not HSV—if there isn’t another, more likely culprit—then call it herpes simplex and treat it as indicated and observe for a response.
A Virus Worth Knowing
This is an unspoken rule in cornea clinics because of how widespread the virus is and its wide range of clinical manifestations. First, in the United States alone, there are 500,000 cases of ocular HSV per year.1 Just about every adult carries HSV serotype 1, and a smaller percentage carries serotype 2, so most adults have some risk. Next, the virus has significant predilection for the eye. HSV keratitis is the most common cause of infectious blindness in industrialized countries.1 Finally, HSV keratitis can present as essentially any form of keratitis, including vesicular pre-dendrites, dendritic epithelial disease, sub-dendritic stromal keratitis, neurotrophic epithelial disease, marginal keratitis, nummular stromal keratitis, diffuse stromal keratitis, necrotizing stromal keratitis, interstitial keratitis (with this, instead of thinking syphilis, think HSV), corneal rings, disciform endotheliitis and linear endotheliitis.
All corneal tissue is at risk for developing HSV involvement, and it can look like just about anything. Unless the exam and history are suggestive of an alternate pathology, you’ll rarely be wrong in treating a unilateral keratitis as HSV and assessing for a response.
Because it is such an important diagnosis, my next few columns will discuss some of the finer elements of identifying and working with patients you suspect might have HSV. As dendritic keratitis theoretically sets the stage for all other forms of HSV keratitis, let’s discuss the dendrite—its clinical behavior, role in the natural history of other HSV keratitides and treatment, which is unique compared with all other forms of HSV keratitis.
 |
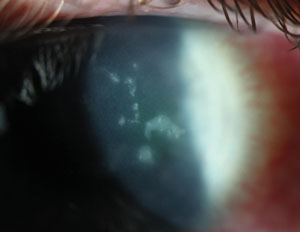
| Fig. 1. If it looks like a dendrite and is ulcerated like a dendrite, it’s probably a dendrite—and this photo is no exception. |
Obviously, having successfully completed optometry school (sorry, student readers), you are aware of dendrites and would never, ever misdiagnose them (Figure 1). Despite the consistency with which infectious epithelial HSV forms dendriform lesions, other conditions may occasionally produce branching epithelial lesions as well, which can lead to some clinical head scratching. Thygeson’s superficial punctate keratitis, for example, generally produces small, round lesions, but may occasionally take on a dendritic appearance. In these cases, the greater number of lesions the smaller size and the (typical) involvement of both eyes suggests Thygeson’s. Zoster-related pseudodendrites or zoster mucous plaque keratitis can each mimic HSV dendrites on gross examination, but on closer evaluation neither of these lesions is ulcerated. HSV keratitis is the most frequent initial misdiagnosis of Acanthameoba keratitis (AK), which in its early stages takes on a pattern epitheliopathy that may have a dendritic distribution; once again, however, these lesions will be non-ulcerated and may have perineuritis. Other rarer causes of dendriform lesions also exist, but given the unique elements of each, the diagnosis of HSV dendritic keratitis should generally be straightforward.
The Dendrite’s Role in HSV Keratitis
The natural history of HSV corneal infection leads to potential for both infectious and inflammatory sequella, which can limit vision. Of the wide range of HSV corneal manifestations, only two have actual viral proliferation and infection as the accepted source of morbidity: dendritic keratitis and the very uncommon necrotizing stromal keratitis.2 Researchers speculate the other forms are inflammatory sequela or a mix of inflammatory and infectious mechanisms.2 This is important for two reasons:
(1) Because dendrites are true infectious ulcerations, we treat them with a topical or oral antiviral and leave out the steroid. Perhaps less known, however, is how unique this treatment is in the spectrum of HSV keratitis. For nearly all other forms of HSV keratitis, the appropriate treatment is pairing a steroid and antiviral, even in cases when a preceding dendrite has not fully resolved (Figure 2). If it’s HSV and not ulcerated, you add a steroid.
(2) HSV is an epithelial-based pathogen, meaning initial attacks have to occur within epithelial cell populations, which open the door for alternate, deeper pathologies. In theory, this means every patient with a deeper form of corneal HSV must have experienced an epithelial episode at one point. In practice, however, this rule is not preserved.
I would estimate that around 50% of the stromal and endothelial keratitides we treat as HSV at our clinic have no compelling historic or objective clinical evidence of previous dendritic keratitis. To reconcile the science with the clinical manifestation, you may look for any telltale irregular anterior scar, which could be an indication of a past episode of dendritic keratitis. When scarring is also absent, however, it does not rule out the possibility of stromal HSV as the underlying etiology. It’s widely speculated that a high percentage of HSV patients will have bouts of subclinical infectious keratitis as their initial corneal exposure rather than a dendritic keratitis.
 |
| Fig. 2. Sub-dendritic stromal keratitis immediately following a dendritic episode. In this case, it’s appropriate to add a steroid and continue the antiviral. |
Without the need for a preceding dendrite, you are free to keep HSV on the differential list for just about any type of keratitis. However, this does require supporting the diagnosis in other ways. In most cases, the clinical picture itself will tell you what you need to know. When further evidence is warranted, clinicians can use ancillary testing.
As HSV tracks along sensory nerves, patients will frequently develop varying degrees of corneal neuropathy and the involved eye will become relatively less sensitive than the non-involved eye. With no esthesiometer at our clinic, we use dental floss to touch the cornea across quadrants to assess sensitivity and compare the involved eye to the non-involved eye. Although an indirect way to assess HSV risk, in a patient with unusual unilateral keratitis and ipsilateral reduced or absent sensitivity, it’s a strong indicator of a viral source or history.
Another ancillary test is a viral swab and culture. This also is only an indicator of active virus, so it will only be positive with a dendrite (which you probably shouldn’t need a culture to identify) or necrotizing stromal keratitis, which diagnostically could benefit from a culture.
When the diagnosis of HSV is more difficult to confirm, a blood test for IgG or IgM viral antigens, while not diagnostic of corneal disease, can support exposure to the underlying etiology. If you are treating for viral keratitis and the antibodies are both negative, you likely need to reconsider your diagnosis. Again, most of our diagnoses of HSV keratitis are based on clinical features, and it is relatively uncommon that we send out for labs.
Infectious epithelial HSV keratitis, which we see clinically as a dendrite, is a fairly simple clinical diagnosis, and its treatment is the most straightforward of any of the manifestations of HSV keratitis. More interesting is the science behind how these episodes set the stage for myriad other, deeper forms of HSV even though, in many cases, the initial infectious bouts are asymptomatic. This, when paired with the extremely varied manifestations of HSV keratitis, frees us to keep it on the differential for virtually any form of corneal inflammation, which is why for any unilateral keratitis without a compelling history, HSV keratitis will always be near the top of your differential until examination and patient history prove otherwise.
1. Farooq A, Shukla D. Herpes simplex epithelial and stromal keratitis: an epidemiologic update. Surv Ophthalmol. 2012;57:448-62.
2. Holland EJ, Brilakis HS, Schwartz GS. Herpes simplex keratitis. In: Krachmer JH, Mannis MJ, Holland EJ, eds. Cornea. 2nd ed. St. Louis: Mosby; 2004:1043-74.


