Eye care providers should have three goals in mind when fitting a patient with keratoconus. Each prescribed contact lens should provide: (1) adequate visual function for a patient’s daily activities, (2) acceptable comfort across the entire wearing period, and (3) proper fitting characteristics, such as sufficient dynamic tear exchange and oxygen transmission, to promote long-term ocular surface health. The patient doesn’t have to see 20/20 or have a lens that “fits perfectly” to have success, provided that these three goals are met.
Specialty lens fitters now have a range of lens designs to choose from, including specialty soft, corneal gas permeable (GP), piggyback, hybrid and scleral lenses. Although new options can increase a practitioner’s fitting success, it can be challenging to know when to use a particular lens design. Here, we discuss new specialty lens designs—and how clinicians can make the right choice for patients with keratoconus.
 |
| Fig. 1. Soft keratoconus lens designs have center thickness typically three to six times that of a traditional custom soft hydrogel lens. |
One fitting strategy is to choose the initial lens type based upon the patient’s graded severity of keratoconus. Many clinicians start with specialty soft lenses if a patient’s presentation is considered mild based on clinical examination. If it’s more severe, fitting a scleral lens might prove more effective. Other variables to consider when choosing an initial design include topography findings, ocular comorbidities, previous lens experience, aperture size, manual dexterity and physical disabilities.
Adding to the fitting challenge is the presence of significant interocular asymmetry that often manifests with keratoconus. As a result, patients may ultimately have the best success with a different lens type in each eye, or may have to wear spectacles over their contact lenses to manage residual astigmatism, presbyopia or both.
Specialty Soft Contact Lenses
Patients who have mild keratoconus can sometimes successfully wear molded disposable soft contact lenses. Here, the primary benefit is patient convenience. These are prefabricated with multi-lens packaging to help reduce the anxiety of losing lenses and are available with various replacement schedules, including daily disposables. However, standard soft lenses are generally unable to provide the required visual improvements for patients with moderate keratoconus. In these cases, patients will need to be fit with a specialty soft keratoconus lens if they desire to stay with soft lenses.
Specialty soft contact lenses—custom designed and lathe cut for each individual eye—allow practitioners to adjust individual lens parameters to improve fit and vision. Soft keratoconus lens designs are manufactured by specialty lens laboratories with extended base curve and power ranges, which can accommodate many of the extreme fitting requirements of keratoconic eyes. This lens type’s center thickness is typically three to six times that of a traditional custom soft hydrogel lens (Figure 1). Enhanced center thickness helps to mask anterior corneal irregularities and decrease HOAs.
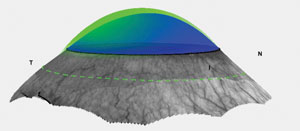
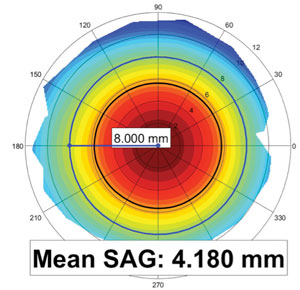 |
| Fig. 2. Corneoscleral topography allows for measurement of mean sagittal height at a selected chord diameter. |
Outside of the optical zone, a soft keratoconus lens is usually lenticularized to reduce lens profile thickness, improving the overall comfort of the lens and increasing oxygen transmissibility over the corneal limbus.
Given the high amount of astigmatic power often prescribed, most specialty soft keratoconus lenses will be ballasted with a double slab-off design to stabilize front surface toricity. They can now be manufactured in hydrogel or silicone hydrogel material. Silicone hydrogel, in particular, can increase oxygen permeability and avoid hypoxia associated with traditional hydrogel.2
The increased expense of lathe cut lenses largely determines lens replacement schedules as recommended by lens manufacturers, which are typically set at two- to three-month intervals.
Most designs are fit using diagnostic lenses by matching the sagittal height of the anterior eye with the sagittal depth of the soft keratoconus lens. High molecular weight sodium fluorescein can help clinicians assess flat or steep fits during the diagnostic fitting process. However, newer instruments capable of providing objective sagittal height data, such as a corneoscleral topographer, have dramatically improved fitting efficiency. Corneoscleral topography allows practitioners to measure mean sagittal height at a selected chord diameter, and a specific soft keratoconus design can then be matched to the sagittal height of the anterior ocular surface (Figure 2).
Corneal GP Lenses
The conventional standard for managing keratoconus has been corneal GP lenses. In fact, they are still the most commonly prescribed rehabilitation device for irregular cornea patients.3 In addition to significantly reducing HOAs, corneal GP lenses are usually least disruptive to corneal oxygenation due to their movement and smaller dimensions when compared with other lens types.1 However, the posterior GP surface bears weight on the cornea, causing longer adaptation time and greater lid-lens interaction.
Corneal GP lenses tend to center at or near the corneal apex and, therefore, can be an excellent choice for fitting keractoconus patients who have more centrally located apices such as central nipple cones and mild paracentral oval cones. Corneal GPs are often the only contact lens option for patients with deep sockets, small apertures or disabilities that prevent successful application of larger lens designs. Corneal GP lenses can be categorized into small (8mm to 9mm), medium (9mm to 10mm) and large (10mm to 11.5mm) diameters. Today, practitioners gravitate toward using corneal GP designs with large diameters, which tend to provide better centration, less unwanted lens movement and improved wearing comfort. Modern corneal GP designs can also offer benefits of aspheric optics, including back surface asphericity, which can improve the fitting relationship against an irregular corneal surface when compared with spherical posterior lens design fitting.
Alignment fitting is often only achieved in those with mild keratoconus, although some corneal touch may become unavoidable as the pathology progresses. Research shows flat-fitting lenses are associated with a higher rate of incidences of scarring.4 Although investigators have not shown a direct causal relationship between GP lens bearing and corneal scarring, it would be clinically prudent to minimize excessive apical bearing, since it can further lead to traumatic epithelial disruptions and associated lens discomfort (Figure 3).
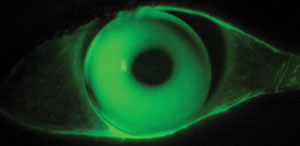 |
| Fig. 3. Apical bearing can lead to traumatic epithelial disruptions and associated lens discomfort. |
To avoid apical bearing with corneal GP lenses in moderate to severe keratoconic cases, clinicians can piggyback a corneal GP lens on a soft contact lens. Due to the epithelial protection provided by the soft lens that is in immediate contact with the cornea, this modality also enables clinicians to troubleshoot short-term sequelae, such as contact lens discomfort from unnecessary mechanical trauma, thus ensuring long-term corneal health.
One of the most common patient objections to being fit for the piggyback lens system is the perceived inconvenience of maintaining two different lenses. Daily disposable lenses can frequently overcome this perception, provided the lens can center reasonably well. Daily replacement lenses can also provide better lens performance, as they are much less likely to develop chronic deposits or other issues with solution sensitivity and allergy-related wearing discomfort. Moreover, using silicone hydrogel materials will ensure enhanced oxygen transmissibility, which is an important consideration with tandem lens wear.
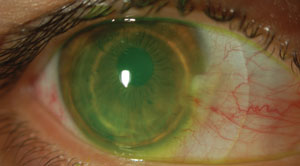 |
| Fig. 4. A built-in soft skirt helps to reduce complexity when fitting keratoconus patients with anatomical scleral obstacles. |
Many patients may not overcome their own perceived objections for piggyback lenses, and some may not adapt to piggyback lenses due to advanced staging of keratoconus. In these cases, newer hybrid lens designs may offer new hope. Hybrid lenses have a central GP disc surrounded by a soft material in the periphery. The GP center can offer good visual quality, while the soft skirt adds comfort by lifting the GP center from sensitive corneal tissue.
Many hybrid keratoconus lenses also have reverse geometry designs. This offers increased mid-peripheral sagittal height to better accommodate a decentered corneal apex and provide enhanced lens comfort. The added feature of reverse geometry also improves overall optics by approximating the optical zone closer to the corneal plane. In addition to reduced adaptation time from the incorporation of a soft lens periphery along with increased sagittal height in recent generations of hybrid lenses, this recombinant lens design reduces lens handling complexity and care compared with a piggyback lens system.5
Not only does a built-in soft skirt assist with the centration of the hybrid lens on the eye, but it also helps to reduce complexity when fitting keratoconus patients with anatomical scleral obstacles (Figure 4). Research suggests the expanded range of fitting parameters in hybrid lenses can improve clinical outcomes in keratoconus patients, with a reported fitting success rate of 86.9%.6
Investigators reported hypoxia and difficulty with lens removal with early iterations of hybrid lenses; however, increased Dk value in GP centers and the incorporation of silicone hydrogel soft skirts (Dk of 84) in the newest hybrid lenses have largely alleviated clinical concerns of poor corneal oxygenation.7,8 Still, some patients have reported initial difficulty with proper lens removal techniques. Thus, it is wise to educate new patients regarding the early adaptation challenge prior to fitting and again at dispensing.
Scleral Contact Lenses
Keratoconus management is the most cited reason for using scleral contact lenses.9 Because the influence of corneal geometry is eliminated or significantly reduced, sclerals can achieve stable fitting patterns with improved comfort even in patients with advanced keratoconus. Most specialty lens manufacturers offer their own scleral lens designs that include fitting features such as bitoricity, notching, microvaults and multifocal optics. Bitoricity in posterior haptical surface can be used when scleral toricity is present, whereas notching or microvault can help to clear anatomical obstacles such as pinguecula or pterygium.
 |
| Fig. 5. Software algorithms can now help practitioners create scleral lenses. |
Some scleral profiles are spherical, so not all patients require a back toric haptic surface. When a patient with a spherical sclera needs front surface toricity, a double slab-off prism can rotationally stabilize a scleral lens. With that said, the ability to measure scleral topography to determine individualized back surface customizations in the haptic zone is an important step forward in improving the fitting efficiency and accuracy.
Commercially available instruments now map corneoscleral topography, and software will allow for simulated fitting of a scleral lens. Software algorithms can determine customized optic zone, limbal zone and haptic shapes to create a scleral lens that clears the cornea by a predetermined vault value set by the practitioner (Figure 5). Fitting software can also help dictate the geometry of a lens design. Although keratoconic corneas are prolate in geometry, some fits will result in more uniform vaulting with a reverse geometry scleral design. For example, keratoglobus, a special subcategory of keratectasia, can challenge even the most experienced practitioner. Typically, these patients require large-diameter scleral lenses (between 20mm and 22mm) to create enough effective sagittal depth to vault over the extreme sagittal height manifested by this condition. Large optic zones and reverse geometry designs are needed to create extra mid-peripheral steepness to avoid peripheral corneal touch.
With recent manufacturing advancements in scleral lens technologies, multifocal optics have become reliable in correcting for presbyopia, even when fitting keratoconus patients. Most scleral multifocals are center-near designs that use simultaneous vision and are effective when two minimum conditions are met: (1) the central cornea is relatively clear of significant scar tissue, and (2) when the scleral lens is well centered.
Whether using a multifocal or single vision design, residual optical aberrations and lens decentration can be detrimental to the success of a scleral lens fitting. Clinicians can add wavefront correction to the front lens surface to correct for residual aberrations, including coma. To provide the best visual outcome, clinicians must ensure the anterior optical zone is decentered so that the center of the front optical zone best matches the presumed location of a patient’s line of sight.
While scleral lenses can certainly be the first choice for patients who have severe keratoconus or keratoglobus, some experts debate whether they should be the first choice for patients presenting with mild to moderate irregularity. Since scleral lens fitting involves more ocular surface area than any other lens type and may lower oxygen bioavailability due to thicker tear lenses, clinicians must objectively monitor for long-term corneal health, as a patient’s subjective comfort may not indicate a healthy ocular surface.10,12
Expanded lens choices and improved designs have helped contact lens specialists better manage irregular cornea patients.
The clinical adoption of corneal collagen crosslinking as a first-line keratoconus treatment can serve to stabilize a majority of patients and reduce the need for constant lens refits.13 It’s essential to remember that even stable keratoconus patients can manifest different visual demands that may require clinical use of different contact lens technologies across various stages of life. Therefore, clinicians must keep an open mind about offering lens fitting options to achieve best possible outcomes.
It may be tempting to offer a universal solution to all problems by fitting everyone in a single lens modality. However, while scleral lenses may be successful for many patients, some eyes will do better with specialty soft lens designs, corneal GP lenses or hybrid lens designs. Clinicians must carefully assess the unique needs of each person and adhere to the three basic fitting goals. Furthermore, keeping up-to-date with advancements in lens design technologies and diagnostic instrumentation is also of paramount importance for the continual delivery of the best keratoconus care we can offer to our patients.
Dr. Chang is director of cornea specialty lenses at Wills Eye Hospital – Cornea Service and director of clinical services at TLC Vision. Also, he is an advisory board member for SynergEyes, International Keratoconus Academy, Gas Permeable Lens Institute and Optometric Cornea Cataract and Refractive Society. You can reach him at [email protected].
Dr. DeNaeyer practices at Arena Eye Surgeons in Columbus, OH. He is a shareholder of Precision Ocular Metrology, has proprietary interest in Visionary Optics’ Europa and Elara Scleral Lenses and is a consultant to Visionary Optics and Alcon. You can contact him at [email protected].
1. Marsack JD, Parker KE, Niu Y, et al. On-eye performance of custom wavefront-guided soft contact lenses in a habitual soft lens-wearing keratoconic patient. J Refract Surg. 2007 Nov;23(9):960-4.
2. Situ P, Simpson TL, Jones LW, Fonn D. Effects of silicone hydrogel contact lens wear on ocular surface sensitivity to tactile, pneumatic mechanical, and chemical stimulation. Invest Ophthalmol Vis Sci. 2010 Dec;51(12):6111-7.
3. Shorter E, Harthan J, Nau C, et al. The role of scleral lenses in the treatment of corneal irregularity and ocular surface disease. 1475 – A0155 ARVO 2016.
4. Barr JT, Wilson BS, Gordon MO, et al. Estimation of the incidence and factors predictive of corneal scarring in the collaborative longitudinal evaluation of keratoconus (CLEK) Study. Cornea. 2006;25:16-25.
5. Hashemi H, Shaygan N, Asgari S, et al. ClearKone-Synergeyes or rigid gas-permeable contact lens in keratoconic patients: a clinical decision. Eye Contact Lens. 2014 Mar;40(2):95-8.
6. Abdalla YF, Elsahn AF, Hammersmith KM, Cohen EJ. SynergEyes lenses for keratoconus. Cornea. 2010 Jan;29(1):5-8.
7. Carracedo G, González-Méijome JM, Lopes-Ferreira D, et al. Clinical performance of a new hybrid contact lens for keratoconus. Eye Contact Lens. 2014 Jan;40(1):2-6.
8. Potter R. The history of hybrid contact lenses. Contact Lens Spectrum. 2015 Nov;30:30, 32-5.
9. Nau A, Nau C, Shorter E, et al. SCOPE study: indications for scleral lens wear. Available at www.pentavisionevents.com/ckfinder/userfiles/files/Nau,%20Amy%20-%20SCOPE%20Study,%20Indications.pdf. Accessed January 31, 2017.
10. Michaud L, van der Worp E, Brazeau D, et al. Predicting estimates of oxygen transmissibility for scleral lenses. Cont Lens Anterior Eye. 2012 Dec;35(6):266-71
11. Visser ES, Visser R, Van Lier HJ. Advantages of toric scleral lenses. Optom Vis Sci. 2006;83(4):233-6.
12. Jaynes JM, Edrington TB, Weissman BA. Predicting scleral GP lens entrapped tear layer oxygen tensions. Cont Lens Anterior Eye. 2015 Feb;38(1):44-7.
13. Chang CY, Hersh PS. Corneal collagen cross-linking: a review of 1-year outcomes. Eye Contact Lens. 2014 Nov;40(6):345-52.


