Whether you’re working with a first-time contact lens patient or an existing wearer who is having difficulties, you need to play every card you hold if you want to win them over to long-term lens wear. During the contact lens fitting process, the influence of case systems on comfort is often sidelined for a proper fit and correction, and with a 24% contact lens dropout rate directly due to discomfort, it can feel like a no-win scenario.1 However, choosing the right lens care system can help minimize discomfort. Here are some of the most important things to keep in mind when recommending an effective and comfortable lens care system for your patients.
1. Consider the Lenses
Choosing the right contact lens solution to keep your patient comfortable starts with choosing a contact lens that meets their needs best; that decision will then dictate much of the care system selection process. Clinicians must consider how the lens dehydrates throughout the day, how stable the lens is on the patient’s eye and much more. “If you had somebody with dry eye, you would want to choose a lens that has a very hydrophilic surface,” says Christine Sindt, OD, director of contact lens service and clinical professor at the University of Iowa. “Something that has a lot of surfactant or polymer or phospholipids to prevent dehydration of the lens material itself.”
While GP lenses take some getting used to for soft lens wearers, they have several valuable benefits.2 GP lenses are more resistant to deposits and bacteria, which could prove beneficial in minimizing long-term comfort decline for patients with eye hygiene issues.3 “Unquestionably, GP lenses are initially less comfortable than soft,” says Daniel G. Fuller, OD, of Southern College of Optometry. “This difference dissipates with adaptation over approximately a two-week period to where it is often clinically insignificant.” One study shows using a topical anesthetic prior to lens insertion during diagnostic fitting and dispensing visits is effective at easing the adaptation process for patients.2
“GP wearers are, by far, more faithful to their solution than the soft lens wearers,” says Dr. Sindt. “They feel like that’s how their contact lenses are supposed to feel vs. other products that say they wet better but don’t have the same gooey feeling to them.”
After deciding on the best lens option, clinicians should turn their attention to the best lens care solution, and its interaction with the lens will be a significant factor in the decision. For example, a lens with high silicone content requires extra attention, as the hydrophobic nature of silicone may create a bond between solution properties and the surface of the lens.4 “You can have the uptake and release of biocides back to the surface of the lens, and that can cause some end-of-the-day drying,” says Dr. Sindt. “If you have a high-silicone lens, you may want to choose to use a peroxide-based solution so that you won’t have the silicone reacting to the solution.”
Sometimes, the lens type necessitates more than a simple multipurpose solution. Patients prone to heavy deposits on their lenses or who wear lenses approved for three months or more may need to use a daily enzymatic cleaner, says Susan Gromacki, OD, MS, director of contact lens service at Washington Eye Physicians & Surgeons.
2. Know Your Patients
Patient lifestyle often weighs heavily on contact lens comfort. Here are some important factors to consider when finding a lens care system to maximize comfort:
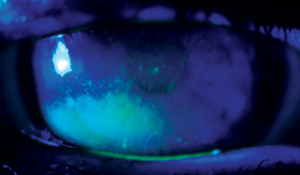 |
| A telltale sign of nocturnal lagophthalmos is inferior cornea staining corresponding to exposure. Photo: Diana L. Shechtman, OD |
Sleep. If a patient is not getting enough sleep at night, their lens comfort can suffer. “Just like our bodies in general, we need time to repair and we’re going to need time with our eyes shut for our eyes to repair,” says Dr. Sindt. Ask your patients about their sleep habits—if they are not getting enough sleep or experience nocturnal lagophthalmos (look for the telltale signs of exposure keratopathy), you may have found the cause of their discomfort.5,6 In these cases, using preservative-free artificial tear at least four times a day may provide relief.7 Ointments and moisture goggles may also be necessary.7
Screen time. The daily amount of hours a patient spends with their eyes focused on a computer, TV, tablet or phone is an increasingly prevalent cause of discomfort.8 It reduces the blink rate, which impairs proper tear film replenishment from lipid release, causing symptoms of dryness.9 Again, preservative-free tears should be among the first lines of defense here to provide relief, but reducing screen time can minimize risk of further irritation.10 For more severe cases, methods that may provide aid include conserving tears through punctal occlusion or cautery, increasing tear production with prescription eye drops and omega-3 fatty acids, or directly treating the inflammation with ointments, warm compresses and lid massage, or daily cleaners.11
Compliance. Noncompliance causes problems with every facet of eye care, so it’s no surprise that it promotes discomfort as well.11,12 Knowing a patient’s noncompliance tendencies can steer you toward specific care systems. “If a patient is going to wear their lenses overnight and remove them one time a week, I want to provide them the solution that will kill the most bacteria during that one night of cleaning,” says Jason Miller, OD, of EyeCare Professionals of Powell, Ohio. For many, a daily disposable option often helps reduce the risk of compliance-related microbial issues and improve comfort.12
Age. The older we get, the greater our propensity for inflammation, and that includes in our eyes.13 Our circulating hormones decrease as we age, and as a result, our ability to control inflammation decreases.13 In cases where age-related inflammation is a problem, practitioners first need to decide whether the inflammation warrants a new form of control in the absence of hormones. Some options for this include topical inflammatory mediators such as cyclosporine, lifitegrast or even steroids.14
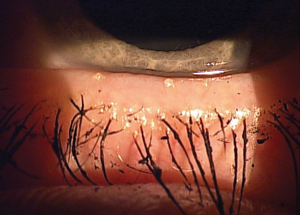 |
| Dry eye disease is a major contributor to contact lens dropout. Photo: Paul M. Karpecki, OD |
Dry eye disease (DED) is also prevalent in patients older than 65, most of whom experience at least some dry eye symptoms.15,9 “A contact lens splits the tear film, so if it is thin or unhealthy, a patient will experience discomfort over time,” says Dr. Gromacki. Research shows DED is a major contributor to the contact dropout rate.1 “Those who continue to wear contact lenses successfully beyond this point require special attention to visual acuity needs and dryness,” says Dr. Fuller. For dry eye sufferers, “lenses with lower wetting angles created by surface treatments or the incorporation of hydrophilic and amphiphilic agents into the lens matrix may help. They attract moisture and mimic the natural tear film.”
In younger patients, hygiene and compliance are potentially problem areas, too. Teens and college students in particular can have an invincibility complex that encourages outright disdain for lens care. As such, these patients may require extra attention and coaching.16
Knowing your patients and all the factors that could affect their contact lens wear will allow you to bring up potential issues before they occur. This is a good way to gain their trust and ensure issues are addressed right from the start. “If the patient does end up having problems, they’re going to think, ‘Wow, you knew that! How did you know that?’” says Dr. Sindt. “And then, because you alerted them to it ahead of time, they’ll go back to you to make sure that it gets managed.”
3. Match Lens Cases With Solution
The importance of compatibility between lenses and solutions is well known; what gets less attention, however, is the need to match cases and care systems. Contact lens cases are specifically designed to go with their solution counterparts, and as such, mixing them up could be problematic, Dr. Sindt says. Some plastics used for lens cases bind preservatives tightly to their surface. If a foreign solution is used and binding occurs, that preservative will no longer be present in the solution.
“The worst cases out there that patients have the most problems with are actually those flat packs that doctors buy with their names imprinted on them,” says Dr. Sindt. “Those are going to have the most uptake and release of solutions, as well as binding of the preservative out of the solution.” The key here is to have patients replace the solution in the case each night and the case itself with each new bottle purchase.
4. Be Careful With Disinfectants
Disinfectants are designed to destroy cell membranes.17 That works to an OD’s advantage to reduce microbial populations, but against them on the ocular surface itself, as exposure to disinfectants can cause irritation. Disinfectants can bind to the lens and break down tears when the lens is on the eye, leading to discomfort.18 For sensitive patients, the presence of disinfectant on the surface or within the matrix of a lens may cause toxic reactions. “It’s always this very fine balance between having a disinfectant that is efficacious enough to kill the bacteria that’s in the well, but isn’t so strong that it’s going to kill the surface of your eye,” says Dr. Sindt.
As with disinfectants, preservatives can bind to the lens, and they are also prone to uptake into the lens material and subsequent release into the tear film, which sometimes causes corneal staining.18
Hydrogen peroxide-based disinfection systems and preservative-free tears can be helpful alternatives.19 For example, Dr. Gromacki recommends hydrogen peroxide for patients with allergies. “But, if the patient wears their lenses less than once per week, then they’ll have to re-disinfect the lenses prior to wearing them,” she says. Hydrogen peroxide solutions also must be neutralized, which can take anywhere from four to six hours, so patient lifestyle will need to allow time for this.20 As a result, practitioners and patients will have to make a decision based on the magnitude of allergies and level of compliance.
5. Avoid Generics
While your patients may be attracted to the lower price tags of generic solutions, the notion that you get what you pay for may apply here. A major issue with generics is the consistency of their contents—or lack thereof, specifically.
About once a year, retailers take bids from solution companies to produce and package their private-label solution.21 The contracts won in the bids generally expire in 18 to 36 months, so the formulation of that generic brand solution may change.21 As a result, there could potentially be two of the same bottle but each could have different chemical formulations.21 Also, “since the contract goes to the lowest bidder, manufacturers are highly unlikely to place their premium lens solutions into privately labeled bottles,” says Dr. Gromacki. “Many of the generic brands, for example, were developed prior to the advent of silicone hydrogels (1999) and as such cause significant solution-induced corneal staining in combination with some of these materials.”
To combat generics, practitioners should address the risks with patients and strongly recommend avoiding them. “Doctors generally delegate training to technicians, but we need to use the ‘power of the white coat’ to prescribe an appropriate care system,” says Dr. Fuller. “If we don’t take the time to explain our decision-making, the patient assumes there is no difference.”
Many factors affect the lens care system you ultimately recommend for your patients, and comfort is just one of them. Despite significant advances in contact lens materials and lens care systems, contact lens dropout rates have not changed significantly in decades.22-25 No one should hold their breath for a technological breakthrough that will solve the many problems that can arise with contact lens wear.22-25 However, if you take the time to balance all your lens care options, ultimate comfort will no longer need to sit on the sidelines.
1. Dumbleton K, Woods CA, Jones LW, Fonn D. The impact of contemporary contact lenses on contact lens discontinuation. Eye Contact Lens. 2013;39(1):92-98.
2. Bennett ES, Smythe J, Henry VA, et al. Effect of topical anesthetic use on initial patient satisfaction and overall success with rigid gas permeable contact lenses. Optom Vis Sci. 1998;75(11):800-5.
3. Morris J. RGP lenses part 1- materials, manufacturing and design. Optician. 2004;228(5971):28-33.
4. Jones L, Powell CH. Uptake and release phenomena in contact lens care by silicone hydrogel lenses. Eye Contact Lens. 2013;39(1):29-36.
5. Latkany RL, Lock B, Speaker M. Nocturnal lagophthalmos: an overview and classification. Ocul Surf. 2006;4(1):44-53.
6. Blackie CA, Korb DR. A novel lid seal evaluation: the Korb-Blackie light test. Eye Contact Lens. 2015 Mar;41(2):98-100.
7. Lawrence SD, Morris CL. Lagophthalmos Evaluation and Treatment. EyeNet. April 2008. www.aao.org/eyenet/article/lagophthalmos-evaluation-treatment. Accessed April 19, 2017.
8. ‘Rideout V. The common sense census: media use by tweens and teens. Common Sense Media. https://roem.ru/wp-content/uploads/2016/12/census.researchreport.pdf. Accessed April 7, 2017.
9. Hauser W. Dry eye: a young person’s disease? Rev Optom. 2017. 154(2):60-4.
10. American Optometric Association. Dry Eye. AOA Glossary of Common Eye & Vision Conditions. www.aoa.org/patients-and-public/eye-and-vision-problems/glossary-of-eye-and-vision-conditions/dry-eye?sso=y. Accessed April 7, 2017.
11. Dumbleton K, Richter D, Bergenske P, Jones L. Compliance with lens replacement and the interval between eye examinations. Optom Vis Sci. 2013;90(4):351-8.
12. Dumbleton K, Woods C, Jones L, et al. Patient and practitioner compliance with silicone hydrogel and daily disposable lens replacement in the United States. Eye & Contact Lens. 2009;35(4):164-171.
13. Sullivan DA, Wickham LA, Rocha EM, et al. Androgens and dry eye in Sjögren’s syndrome. Ann N Y Acad Sci. 1999;876:312-24.
14. Genvert GI, Cohen EJ, Donnenfeld ED, Blecher MH. Erythema multiforme after use of topical sulfacetamide. Am J Ophthalmol. 1985;99(4):465-8.
15. Lonsberry B. Dry eye in the office. Rev Optom. February 2008. www.reviewofoptometry.com/article/9th-annual-dry-eye-report-dry-eye-in-the-office. Accessed April 7, 2017.
16. Wagner H, Richdale K, Mitchell GL, et al. Age, behavior, environment, and health factors in the soft contact lens risk survey. Optom Vis Sci. 2014;91(3):252-61.
17. Centers for Disease Control and Prevention. Division of Oral Health - Infection Control Glossary. www.cdc.gov/oralhealth/infectioncontrol/glossary.htm. Accessed April 7, 2017.
18. Gromacki SJ. Contact lens deposition and dry eye. Contact Lens Spectrum. 2012;28(7):23.
19. Riley MV, Wilson G. Topical hydrogen peroxide and the safety of ocular tissues. CLAO J. 1993;19(3):186-90.
20. Willcox M. Hydrogen peroxide versus multipurpose disinfecting solutions, what are the differences? July 2008. Available at: www.siliconehydrogels.org/editorials/jul_08.asp. Accessed April 18, 2017.
21. Gromacki SJ. The truth about generics. Contact Lens Spectrum. 2005;20(12):24.
22. Schlanger J. A study of contact lens failure. J Am Optom Assoc. 1993;64(3):220-4.
23. Weed K, Fonn D, Potvin R. Discontinuation of contact lens wear. Optom Vis Sci. 1993;70(12s):140.
24. Pritchard N, Fonn D, Brazeau D. Discontinuation of contact lens wear: A survey. Int Contact Lens Clin. 1999;26(6):157-62.
25. Young G, Veys J, Pritchard N, Coleman S. A multi-centre study of lapsed contact lens wearers. Ophthalmic Physiol Opt. 2002;22(6):516-27.


