|
The number of patients diagnosed with glaucoma is expected to exceed 70 million by 2020.1 When pharmacological or laser treatments fail to control intraocular pressure (IOP), surgical options such as trabeculectomy can be effective.2 But what happens when these patients need contact lenses? To prevent fibrosis, the conjunctiva above the bleb is usually treated with mitomycin C or 5-FU, both of which can make the conjunctiva thin and more susceptible to infection.3-4 Additionally, if soft or rigid lenses induce mechanical trauma to the bleb, they can lead to blebitis or endophthalmitis.
To respect the integrity of the bleb, contact lens practitioners have three options: a soft low modulus lens that vaults the entire bleb, a notched scleral lens or a small, well centered rigid gas permeable (RGP) lens fit with minimal excursion.5
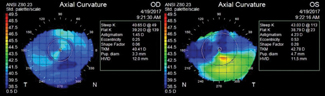 |
| Fig. 1. Topographical map of this patient revealed a normal cornea OD and an elevated scar inferior temporal OS. |
Case
An 84-year-old female presented with long-standing blurred vision OS for a contact lens evaluation after referral by her glaucoma specialist. Her vision did not correct well with glasses and she felt it was worsening. Her history included glaucoma OU, herpes simplex virus infection OS in 2012 with residual scarring, s/p trabeculectomy OS in 2014 and bleb revision OS in 2016. Her medical history was positive for hypertension, hyperlipidemia and osteoporosis.
Her presenting visual acuity (VA) was 20/20 OD and 20/200 OS, pinhole: 20/40, with a spectacle prescription of -1.25 +1.50x 27 OD and plano +0.75x156 OS. Her manifest refraction was -1.25+1.50 x027 VA 20/20 OD and -0.25+2.50 x 120 VA 20/150 OS, pinhole to 20/40. A slit lamp exam revealed 1+blepharitis OU, a clear cornea OD and inferior corneal scar OS and an elevated avascular bleb adjacent to the superior limbus OS (Figure 1). The anterior chamber was deep and quiet OU. Her irises were normal with posterior chamber intraocular lenses OU. IOP was soft and equal by digital palpation OU.
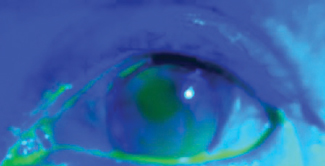 |
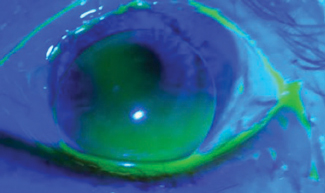
| Fig. 2. Here, the first lens is positioned under the patient’s bleb, but is still too close. |
Diagnostic Conact Lens Fitting
We performed a diagnostic RGP over-refraction in office to determine the best potential acuity of the left eye. An 8.33/-3.00/9.6 diagnostic lens with standard curvatures was placed on the patient’s eye. Over-refraction of +4.50 brought the vision to 20/25+. The lens was aligned, but it was riding high and hit the bleb with each blink. We ordered the lens smaller with the central base curve steepened to compensate for the flattening effect of the decrease in diameter. A half-diapotor of prism base down was added to weigh the lens down and away from the bleb.
The parameters of this first lens were 8.23 BC/+1.25 power/9.2 diameter/0.5 diopter base down.
Dispensing Visit #1
The patient presented for a dispensing visit one week later with no new complaints. Her VA was 20/20 with no over-refraction. The position of the lens was lower but was still too close to the bleb (Figure 2). Each blink caused the lens to hit the bottom of the bleb. As a result, we ordered another lens with an additional half-step of prism base and 0.2mm smaller than the previous.
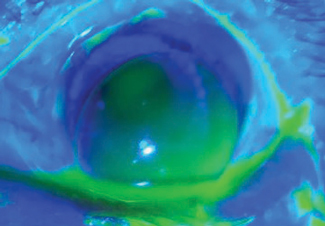 |
| Fig. 3. At the second dispensing visit, although the lens sat low and did not touch the bleb on blink, vision was less than ideal due to decentered optics. |
Parameters for this lens were 8.23 BC/+1.25 power/9.0 diameter/1D base down.
New lens parameters were 8.23 BC/+1.25 power/9.0 diameter/0.5D base down/1 step steep edge.
Dispensing Visit #3
When the patient presented for another dispensing visit a week later, her vision was measured at 20/20 with no over-refraction. The lens alignment was slightly steep but more centered over the pupil (Figure 4). There was less mobility on blink, but the amount was still adequate and the lens did not disturb the bleb. We trained the patient on lens insertion and removal and sent her home to try for a week.
 |
| Fig. 4. Here is the lens clearing the bleb during the third dispensing visit. Its alignment was slightly steep but more centered over the pupil than the previous lens. |
Follow-up
The patient presented one week later with no complaints. She was thrilled with the new vision in her left eye and was able to wear the lens comfortably. Her vision was 20/20. A slit lamp examination revealed a well-fit lens that cleared the bleb on each blink without punctate staining from the tighter than usual edge. The lens was finalized.
Patients who undergo glaucoma surgeries sometimes present with comorbidities that require RGP correction for better vision (i.e., corneal irregularities or aphakia). Fitting contact lenses on patients post trabeculectomy continues to be a bit controversial, and there are arguments to be made on both sides of the equation. Not fitting a lens will deprive the patient of better vision, while wearing a lens can compromise the integrity of the bleb and put the patient at risk for infection. However, the success rate of RGP lenses post trabeculectomy shows some promise.6-8
When a patient presents for a contact lens fit, practitioners should consider the status of the bleb and any history of prior infection or instability, as this can put the patient at greater risk for infection.6 Additionally, patients should be well educated on the signs and symptoms of an infection. These patients can be challenging to fit; as such, vigilant follow-up is an essential part of their success.
1. Tham YC, Li X, Wong TY, et al. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121(11):2081-90.
2. Guttman C, Singh K. Clinicians must weigh value of randomized clinical trial results. Ophthalmology Times. 2004;29(11):18.
3. Ticho U, Ophir A. Late complications after glaucoma filtering surgery with adjunctive 5-fluorouracil. Am J Ophthalmol. 1993;115(4):506-10.
4. Franks WA, Hitchings RA. Complications of 5-fluorouracil after trabeculectomy. Eye. 1991;5:385-9.
5. DeNaeyer GW. Contact lenses After Trabeculectomy. Contact Lens Spectrum. January 1, 2010. www.clspectrum.com/issues/2010/january-2010/contact-lenses-after-trabeculectomy. Accessed July 28, 2017.
6. Samples JR, Andre M, MacRae SM. Use of gas permeable contact lenses following trabeculectomy. CLAO J. 1990;16(4):282-4.
7. Lois N, Dias JL, Cohen EJ. Use of contact lenses in patients with filtering blebs. CLAO J. 1997;23(2):100-2.
8. Pederson K. Enhance postoperative filtering bleb-induced vision difficulties with well-fitted GP contact (oxygen-permeable) lenses. Optometry. 2005;76(2):115-22.