 |  |
When we started out in practice, gas permeable (GP) lenses were a mainstay. Practitioners readily fit everyday patients for them, and both practitioners and patients saw them as normal. However, over the last 10 years, opinions surrounding GP lenses have shifted. For example, many patients and practitioners began to overlook the benefits of GP lenses as a result of the increased availability of soft lenses.
One of the benefits of soft lenses, generally, is near immediate comfort for most patients. GP lenses, meanwhile, have historically been known for exceptional performance in vision. Recently, however, interest in GP lenses has picked back up in the marketplace.1 Here is an overview of three GP lenses and how they can help dramatically grow your practice in patient loyalty and satisfaction.
Orthokeratology
In the 1970s, practitioners started to see the benefits of fitting lenses flatter than the corneal shape. Although most of these lenses were worn during the day and provided variability in vision, the realization started the movement around orthokeratology (ortho-k). This resulted in dramatic growth of the understanding and knowledge of reverse geometry lenses. The rest is history.
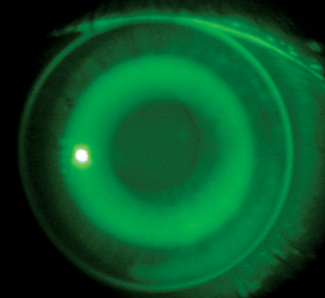 |
| Ortho-k lenses are a potentially beneficial option for myopes. |
Orthokeratologists began anecdotally reporting that some of their patients appeared to have slower myopia progression compared with their eyeglass-wearing counterparts. In 2004, one study showed that both the anterior chamber and vitreous chamber depths increased nearly twice as much in patients wearing spectacle lenses compared with those wearing ortho-k contact lenses.2 The body of evidence continues to grow around the benefits of ortho-k for children who are progressing or may progress in their myopia.3
Despite the evidence, many practitioners are reluctant to initiate ortho-k in their practice, whether stemming from a lack of understanding, a lack of knowledge about effects or concern about chair time. However, myopia stabilization through accelerated reshaping technique has revealed incredible success with ortho-k.4 In one study of myopia stabilization, about 80% of patients had success with their initial lens fitting, and nearly 95% of them had success with, at most, one lens change. This type of success is rarely achieved with soft toric lenses, let alone soft multifocal lenses. Seeing a lens perform so successfully is a helpful way to pull back hesitation barriers for both chair time and fitting complexity.
The investment required to start prescribing ortho-k is small, while the patient and financial benefits can be large. If you’re looking to dip your toe in, be sure to form a good relationship with one of the major orthokeratology manufacturers. Generally, clinical consultation will be your best ally. To get started, try calling an orthokeratology company to find out about the process.
If what they outline seems complicated and difficult, simply try another lab. Once you find a process that fits you and your practice, you will need to take a short course outlining the lens and its fitting system followed by a certification test. Although this may seem like a waste of time, rest assured that the small investment will be well worth it as you begin fitting.
Next, you will need to identify a patient to start with. Working with a low myope (-0.75D to -1.5D) is a good way to maximize your success and build your confidence. If you are fitting empirically, order the lens based on the parameters set forth by your chosen manufacturer (usually Ks, Rx and HVID). A follow-up visit will then allow you to determine whether the case is a success or another lens order is required.
Calling the laboratory and sharing your experience will be helpful in either case. A great company will have consultants to coach you on the next steps.
Typically, ortho-k is an out-of-pocket cost for patients. Its benefits are best known for myopia control, but it also allows the freedom from daytime contact lenses and glasses, something that often goes over well with adults and parents of school-aged children. Ortho-k is an excellent way to reshape your practice financially and, more importantly, for your patients’ benefit.
Multifocals
We see presbyopic patients in our offices every day, but sometimes forget to mention multifocal contact lenses as an available option for them. When we do mention them, however, it sparks great conversations. Some of these patients have dropped out because of comfort issues, in which case it is important to address their ocular surface disease more aggressively. Others may be unaware that they can still wear contact lenses. Despite this, you’ll likely find that a good number of patients want to wear lenses. For many, simultaneous vision soft multifocal contact lenses are suitable options to meet visual demands, but for those seeking full-time wear, soft mutifocals can fail to provide crisp clarity. For these patients, GP multifocal lenses are in order, of which there are two different types that need to be considered:
Aspheric. Both anterior and posterior aspheric powers can be incorporated into multifocal lenses. Due to the optics, amount of add that can be placed on the anterior surface is limited. However, it is easier to move a spherical single vision patient into a lens by simply adjusting the curvature of the anterior surface. As the demand for add goes up, many patients will require additional power adjustments to the posterior surface.
Segmented. Like a lined bifocal, some patients need a segmented or translating GP multifocal lens. These lenses require a unique fitting system to ensure the patient gets into the add zone upon downward gaze. Although these are somewhat complicated to fit, they can provide incredible value to patients who require their visual benefits.
Multifocals are an excellent way to grow your practice. They help keep patients in lens wear longer and provide an incredible amount of value for patients who want to be spectacle-free. They can provide financial benefits both in the short-term and long-term.
Sclerals
Since starting to fit scleral lenses in 2004, we have seen them dramatically grow in popularity. Our understanding of their effect on the eye, coupled with our ability to better fit patients, has helped bring them into the mainstream awareness. Because these lenses fit under the upper lid, they tend to provide much better initial comfort for patients. Also, since they are large and do not move or translate on the eye, they provide much better stability of vision for patients.
While there are always some cases that need advanced troubleshooting or a more advanced lens design, for most patients scleral lens fittings can be achieved by following three simple steps:
- Clear the central cornea by around 100 to 300μm.
- Clear the limbus.
- Land the scleral landing zone on the conjunctival surface as tangentially as possible.
There are many fitting guides, groups and training tools to help you get started in fitting scleral lenses. Our recommendation: Get started.
There are several practice management situations you will need to consider depending on the reason you are fitting a patient for scleral lenses. If you’re fitting for medical reasons (i.e., keratoconus), you will need to make sure your billing and coding team knows the proper codes to use. However, if you are fitting for astigmatism or presbyopia, you will likely be charging the patient out of pocket. With the increased cost of goods for scleral lenses, it is important to understand how to set your lens fees as well as your chair time costs.
Fitting patients for myopia management lenses, multifocals and scleral lenses can have a huge impact on your practice. Give all three a try as soon as you can.
1. Nichols JJ. Contact lenses 2016. Contact Lens Spectrum. 2017;32:22-25.
2. Cho P, Cheung SW, Edwards M. The longitudinal orthokeratology research in children (LORIC) in Hong Kong: a pilot study on refractive changes and myopic control. Curr Eye Res. 2005;30(1):71-80.
3. Walline JJ, Jones LA, Sinnott LT. Corneal reshaping and myopia progression. Br J Ophthalmol. 2009;93:1181-5.
4. Eiden BS, Davis RL, Bennett ES, et al. The SMART Study: background, rationale, and baseline results. Contact Lens Spectrum. October 1, 2009. www.clspectrum.com/issues/2009/october-2009/the-smart-study-background,-rationale,-and-baseli. Accessed August 5, 2017.


