 |
Refractive surgery can leave patients happy for many years. Unfortunately, in some cases, their refraction starts to degrade and they appear at your door, disappointed with their newfound blurry vision. What course of action would best suit these patients? Enhancement surgery? Glasses? Soft lenses? Custom lenses? Gas permeables?
A Lens for Every Eye
When patients undergo refractive surgery, their corneal shape is permanently altered. In some cases, patients can achieve post-op functional vision with standard glasses or soft contacts, and this option should be discussed. However, GP lens designs are often the only option to return their vision to 20/20.
• Glasses. Patients are sometimes able to see fairly well (20/40 or better) or even extremely well (20/20) with a spherocylindrical refraction. If this is the case, glasses should be presented as an option. However, 20/20 quantity with glasses does not always translate to 20/20 quality, so I always offer contact lenses first if the patient is a good candidate.
For example, I had a patient who had undergone previous RK surgery and who had worn progressive addition lenses for many years. With glasses, his vision was 20/20 in each eye. Although he had good vision, I asked him if he was interested in contact lenses. He was shocked; all these years, he thought contacts were not an option for him. “I would love to get back into contacts if I could!” he said.
• Soft contact lenses. A patient with a fairly normal prescription and minimal irregular astigmatism may be a good candidate for soft contact lenses. I find most have undergone LASIK or PRK, rather than RK surgery.
If you have trial lenses on hand, try applying a pair to the patient’s eyes to check vision clarity and lens fit. If the contacts fit well and the vision is acceptable, the patient could save a bit of money by using a basic lens. A standard soft toric lens may also work if the patient is able to achieve acceptable vision with refraction with some astigmatism. It’s best to start with the easiest and most cost-effective solution for the patient when possible.
• Soft custom toric lenses. Able to be made with virtually any base curve and power, custom soft lenses are perfect for patients with fairly regular astigmatism too high for standard soft toric lenses. Also, some soft custom lenses like Novacone, Kerasoft IC and Flexlens ARC have an increased center thickness to help mask small to moderate amounts of irregular astigmatism. Soft custom lenses are usually available in one-degree axis increments, which can really dial in a patient’s vision.
• Hybrid lenses. These combination lenses may be the answer for patients with a fairly normal corneal shape. Hybrid contact lenses combine a GP center with a soft lens skirt to give the patient the vision clarity of a GP lens and the comfort of a soft lens. The GP portion of the lens could help to correct any irregular astigmatism as well. However, I wouldn’t recommend a hybrid lens on a severely irregular cornea—the lens will likely decenter and corneal staining can often be seen. There is also a risk of corneal flattening over time.
Often, the GP portion will land at the “knee” of the treatment zone, causing seal-off or an abrasion. As an aside, RK patients have a more profound knee because, since tissue is not removed, as the center is flattened, the periphery is steepened.
• Corneal and intralimbal GP lenses. Certain corneal and intralimbal GP designs can be beneficial for patients who have undergone previous refractive surgery. These designs contain unique reverse curves with varied amounts of curvature to match the oblate shape of a previously myopic eye. It’s best to discuss design recommendations with a laboratory consultant, however, as all GP labs have surgery-specific designs.
• Scleral lenses. Sclerals are another option for many post-refractive surgical patients. These large lenses vault the cornea and rest on the sclera with a layer of liquid cushioned underneath, a design that can have many benefits.
 | |
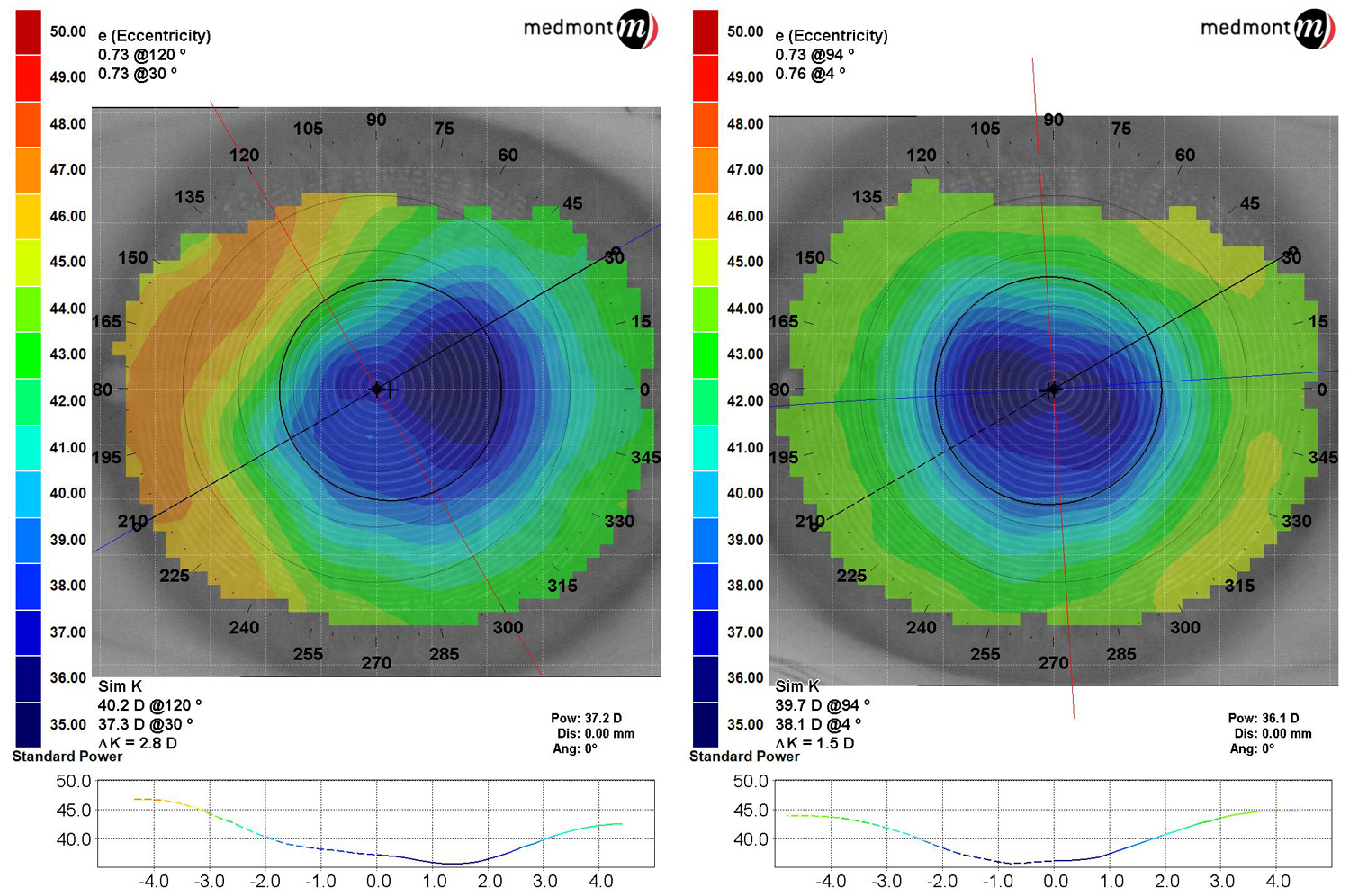
| Fig. 1. Post-LASIK ectasia shows steepening centrally similar to a keratoconus patient. |
First, since the lens does not touch the cornea, keratitis and scarring risks are greatly decreased. Second, the fluid layer helps to prevent fluctuating vision in post-RK patients, who are notorious for having varied refractions throughout the day. This is often thought to be due to the ever-changing corneal shape from hour-to-hour, and offering these patients a solution to their constantly fluctuating vision can be invaluable. Third, many patients who have undergone refractive surgery complain of dry eye. As scleral lenses are often used to treat dry eye symptoms, they can offer a solution to your patient’s vision inconsistencies and discomfort.
• EyePrint Lenses. If a patient has an extremely irregular cornea or sclera, consider the EyePrintPro system, which takes an impression of the patient’s unique ocular surface, generates a three-dimensional scan, then uses software to create a lens perfectly shaped to the entire ocular surface. The extreme stability of this design allows both toric and prism correction to be placed in any axis. Though any refractive surgery patient could be considered a candidate for this lens, RK patients in particular would greatly benefit from this device.
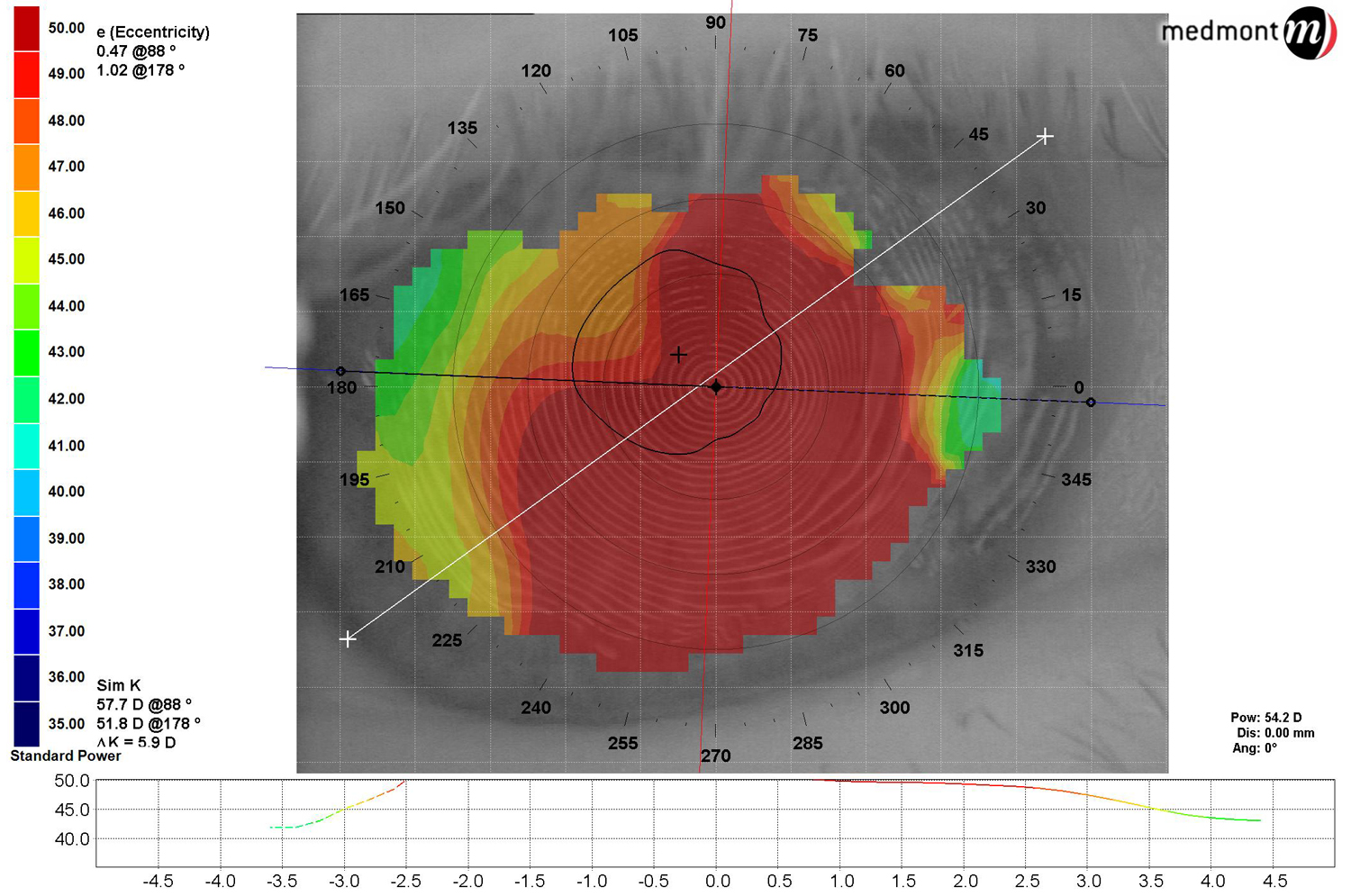
It’s important to note that both post-LASIK ectasia and hexagonal keratectomy patients exhibit topographies similar to a keratoconic patient (Figure 1). Fitting them is very similar to fitting a keratoconic or pellucid marginal degeneration patient, so fit these patients with your favorite keratoconic design!
Case Report
A 58-year-old Caucasian female presented to the clinic for a comprehensive eye exam. She reported undergoing RK in both eyes in 1992 and has worn lined bifocal glasses for the past 15 years. She complained of dry eyes and blurred and fluctuating vision.
Her BCVA in the OD was 20/70 and the OS was 20/50 with a large amount of irregular astigmatism in both eyes (Figure 2). Many RK scars were seen in both eyes under slit lamp examination.
|
|
| Fig. 2. Post-RK patient showing oblate corneas. |
At this time, scleral contact lenses were recommended. The patient was eager to try and solve some of her ocular complaints. After a diagnostic scleral contact lens fitting, the patient was dispensed:
OD: Atlantis scleral/ 7.85 BC/ 16.5 OAD/ standard limbal zone/ standard edge/ -3.50
OS: Atlantis scleral/ 7.78 BC/ 16.5 OAD/ increased limbal zone/ standard edge/ -4.00
Through these lenses, the patient saw 20/25 in both eyes.
During her follow-up visits, the patient reported less fluctuating vision while wearing her contacts and also decreased dry eye symptoms. She is extremely happy with the vision and comfort of the contacts, and I am happy with her corneal health. She has been successfully wearing these lenses for one year.
Generally, patients who have had refractive surgery are some of the best candidates for contact lenses because they likely underwent the surgery in the first place to eliminate the need for glasses. However, often they have been told by other doctors that they cannot wear contact lenses, so they may not even ask you about lens options.
So, the next time you have a post-surgical patient who normally wears glasses, offer them the option of contact lenses instead. You will be surprised at how many patients jump at the opportunity to enjoy contacts again!


