Once only available in specialized tertiary care centers, scleral lenses have become increasingly popular in general optometric practice during the past several years. Recent proliferation of scleral lens designs, the ready availability of diagnostic fitting sets and growth of educational programs and workshops designed to teach those interested in this lens modality how to fit them properly have vastly increased awareness and availability of these lenses among eye care providers.
Indications for scleral lens prescriptions are expanding as well. Originally, the lenses were reserved for eyes with severe irregularity or surface disease and were used only when all other therapeutic options had been exhausted. Now, not only are scleral lenses being prescribed for less severe disease, they are also being marketed as an option for correction of uncomplicated refractive error. Despite this overall progress, however, many optometrists remain wary of incorporating scleral lenses into their practice due to concerns regarding excessive cost, time or potential complications.
The Keys to the Kingdom
Fortunately, there are a number of considerations you can make to simplify the process of fitting scleral lenses. Don’t be afraid to pick and choose, or come up with your own ideas!
|
|
|
|
|
Fig. 1. Fitting scleral lenses isn't a high-tech endeavor; all you need is a diagnostic lens fitting set, slit lamp and phoropter. Photo: Christine Sindt, OD |
1. You don’t need to spend a fortune to fit scleral lenses. Depending on what images you have seen presented during scleral lens courses or lectures, you may have the impression that fitting these lenses requires a considerable capital investment. Not to worry—fitting sclerals is a surprisingly low-tech affair for most patients.
It’s true that anterior segment OCT can precisely define the fitting relationship between the lens and anterior ocular structures and confocal microscopy can provide much information on how scleral lens wear may affect corneal structure and function. However, this equipment is by no means necessary to fit scleral lenses. Additionally, more commonly available imaging technology such as corneal topography—while extremely useful in fitting corneal rigid gas permeable lenses—may be of only limited value in fitting scleral lenses because precise alignment between the anterior corneal and posterior lens surfaces is unnecessary in scleral lens fitting.1 Slit lamp photography can also be used to document lens fit as well as anterior segment structures, which may be helpful in following the condition of the eye over time, but is not essential in scleral lens fitting.
Realistically, an eye care provider who is interested in developing a scleral lens practice needs only the most basic equipment to get started. A diagnostic scleral lens fitting set, a slit lamp and a trial lens set or phoropter are all that is necessary. These rudimentary items, along with careful observation and evaluation, can provide all of the information necessary to successfully fit scleral lenses. Diagnostic lenses will allow you to assess the fit of the lenses, and over-refraction with either handheld trial lenses or a phoropter will provide the refractive information that you need to order the initial lens.
2. Learn how to use one or two lens designs well. There are dozens of scleral lens designs available today. While there are certainly differences between them, the fitting goals for all designs share some common characteristics. First, scleral lenses are designed to land on the conjunctival tissue overlying the sclera without causing excessive compression of tissue or blanching of conjunctival vasculature. Second, the lenses should completely and measurably vault the cornea and limbus. Finally, the lenses should exhibit minimal vertical or lateral movement on the blink.
Most major laboratories now offer scleral lens designs, so consult with your lab to get recommendations on their most successful designs. While it is not necessary to become familiar with all scleral designs, it may be helpful to procure fitting sets for one larger (approximately 17.0mm to 18.0mm) and one smaller (approximately 15.0mm to 16.0mm) design. This will allow for successful scleral lens fitting for a variety of indications.
Laboratory consultants are also typically well versed in scleral lens fitting, and can provide invaluable assistance to novice scleral lens fitters. Additionally, educational resources are available both at formal professional meetings and online through organizations such as the Scleral Lens Education Society and Gas Permeable Lens Institute.

|
|
| Fig. 2. Observation of the contour of the cornea and sclera from the side can help you choose an initial diagnostic lens. |
3. Make the most effective use of your time. Selecting an initial diagnostic lens can be challenging for the first-time scleral lens fitter. So, make use of all the tools at your disposal. Manufacturers’ guidelines can be useful, as can simple observation of the contour of the cornea and sclera as viewed from the patient’s side (Figure 2). Once you become familiar with your lens design, it’s likely you will be able to better predict which diagnostic lens will provide an appropriate fitting relationship on the basis of observation alone.
If you are uncertain of which lens to select, err on the side of greater sagittal depth. It is much easier to estimate the amount of excessive clearance in a lens that is too steep than it is to estimate the amount of additional sagittal depth required to clear the cornea in a lens that fits with considerable corneal touch.
Although we know that scleral lenses tend to settle with time, evaluating lens fit immediately after application will allow you to identify a lens that obviously provides too much or too little clearance.2 Bracket the fit in large intervals until you find a lens that demonstrates approximately 100µm to 150µm more clearance than would be considered ideal. Once you’ve identified an appropriate lens, allow the lens to settle for 20 to 30 minutes before final evaluation of fit.
It should be noted the “ideal” amount of clearance in scleral lens fitting has yet to be defined. Although recent studies have suggested that decreased oxygen transmissibility through an excessively deep fluid reservoir may be undesirable, successful scleral lens wear has been achieved with lenses providing between 100µm and 600µm of clearance.3,4
4. Get creative with initial lens application. Patients may be apprehensive during initial lens application, even if they have had previous experience with contact lenses. Distracting them from the application process, either by giving them something to do (such as holding their lower lid down while you apply the lens) or by encouraging them to look at something (such as a bottle cap or other object held on their lap) may make initial lens application easier.
While opening the lids widely enough to apply the lens directly to the ocular surface is ideal, it is not always possible. Sometimes, you may need to apply the lens by placing one edge beneath either the upper or lower lid and then “folding” or “tipping” the lens into place. If you find that you need to manipulate the angle of the lens during application, it may be helpful to use Celluvisc or another relatively viscous non-preserved product to prevent excessive fluid loss during application. Patients may also find it easier to avoid entrapped air bubbles if they use a more viscous product during initial lens application training. Using these products as “training wheels” can give patients confidence in their ability to successfully handle and wear lenses.
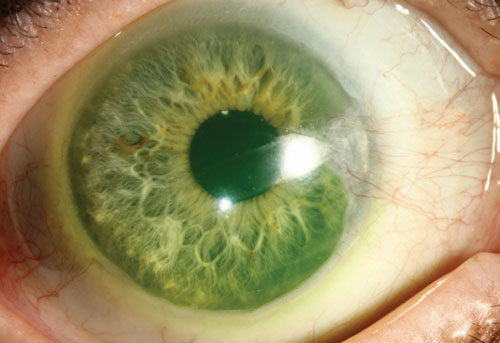
If you wish to use fluorescein to define the fluid reservoir during the fitting process, the dye can either be placed in the bowl of the lens prior to application or applied to the ocular surface directly. While the concentration of dye in the post-lens fluid reservoir may be somewhat diminished if fluorescein is applied to the ocular surface prior to lens application, the concentration will still be sufficient to allow for easy visualization of the fluid reservoir. Applying fluorescein to the ocular surface rather than placing the dye in the bowl of the lens also reduces the risk of staining clothing or fingers during lens application.
5. Perform a careful spherocylindrical over-refraction. The tear film beneath a corneal rigid gas permeable lens is of negligible thickness, and allows for reasonably accurate calculation of power for a lens of a given base curve on a given eye. Not only are most scleral lenses considerably thicker than corneal lenses, but the post-lens fluid reservoir is of considerably greater depth than the tear layer behind a corneal lens. Increased lens and fluid reservoir thickness could potentially alter effective lens power, so careful refraction over a diagnostic scleral lens is recommended to avoid power calculation errors.
Consider using handheld trial lenses to refine the prescription. Trials lenses can frequently be held very close to the anterior surface of the scleral lens, and can even touch the surface of the lens, if desired. This minimizes the need to calculate power adjusted for vertex distance.
Unlike spherical corneal GP lenses, scleral lenses tend to be very stable on the ocular surface. This rotational stability allows for incorporation of front surface toricity onto scleral lenses to correct residual astigmatic refractive error. Numerous lens designs now offer this option. Patients with as little as 0.75D to 1.00D of residual astigmatism with a spherical scleral lens may appreciate improved clarity with a toric lens. If your patient demonstrates improved visual acuity with a spherocylindrical over-refraction compared to a spherical over-refraction, consider ordering a front surface toric lens.
6. Follow your patients closely. Sclerals are still relatively new additions to the market. Although they are made of materials that have long been used, these lenses exhibit considerably different fitting characteristics than any other lens modality. We should not simply assume complications associated with scleral lens wear are identical to those we see with other lens modalities, nor should we assume risk factors for those complications are exactly the same as those that have been identified for other lenses. Though there have been case reports of microbial keratitis, we do not know for certain if risk factors are the same with sclerals as with corneal lenses; ideally, a national or international complications registry is needed. It should be noted, however, that application error might be a scleral-related complication—patients can give themselves corneal abrasions if the lens scrapes the cornea during insertion.
When scleral lenses are used in the treatment of severe ocular surface disease or corneal ectasia, the risk of complications that could be caused by scleral lens wear are outweighed by potential benefits, including the avoidance of more aggressive surgical intervention and maintenance of ocular surface integrity. However, as indications for scleral lenses have expanded to include correction of simple refractive error, we would do well to carefully evaluate relative risks and benefits of scleral lens wear compared to other options for refractive correction.
Ongoing management of ocular disease necessitates frequent follow-up for patients who use scleral lenses as therapeutic devices. Although patients who choose to wear scleral lenses for correction of uncomplicated refractive error may not have medical conditions that require frequent evaluation, regular examination of anterior ocular structures is prudent even in these patients. Frequent follow-up would allow for early identification of potential tissue changes, and would enable adjustments in lens design to minimize the potential for irreversible tissue damage.
7. Define your success. Characteristics of the “ideal” scleral lens fit have been described, but there may be more than one lens design that could provide an acceptable fit for a given patient. A scleral fit can be considered successful if the lens is stable on the eye, the patient achieves the best possible vision with the lens, there are no changes in ocular surface structures or tissue as a result of lens placement and long-term wear is comfortable. If the lens meets these criteria, you may declare success!
Dr. Schornack is a consultant in the department of ophthalmology at the Mayo Clinic in Rochester, MN. She is also a founding member of the Scleral Lens Education Society, and currently serves as the organization’s vice president.
1. Schornack MM, Patel SV. Relationship between corneal topographic indices and scleral lens base curve. Eye & contact lens 2010;36:330-333.
2. Kauffman MJ, Gilmartin CA, Bennett ES, Bassi CJ. A Comparison of the Short-Term Settling of Three Scleral Lens Designs. Optometry and vision science : official publication of the American Academy of Optometry 2014.
3. Michaud L, van der Worp E, Brazeau D, et al. Predicting estimates of oxygen transmissibility for scleral lenses. Contact lens & anterior eye : the journal of the British Contact Lens Association 2012.
4. Sonsino J, Mathe DS. Central Vault in Dry Eye Patients Successfully Wearing Scleral Lens. Optometry and vision science : official publication of the American Academy of Optometry 2013.


