Luckily, eye care practitioners have several treatment options available, including corneal reshaping with orthokeratology (ortho-k). Several studies show the effectiveness of ortho-k in slowing myopia progression in children.3-8 Researchers found axial elongation was 51% to 57.1% less compared with a control group wearing spectacles or soft contact lenses.6,8
But many patients with myopia have astigmatism, which can sometimes complicate ortho-k therapy. Nearly one quarter of patients wearing soft contact lenses require astigmatism correction, and 32% of patients with myopia present with astigmatism of 0.75D or greater in both eyes.9 These statistics suggest the number of patients with astigmatism is associated with the increasing of the number of patients with myopia. To effectively treat this patient population, clinicians must find creative alternatives to traditional ortho-k therapy. This article takes a closer look at the use of toric ortho-k lenses for myopia control in patients with astigmatism.
Efficacy of Toric Ortho-k
Researchers have suggested toric lenses can slow axial elongation in patients with myopia with astigmatism.10,11 A study investigating the effectiveness of toric ortho-k lenses for myopia control in children ages six to 12 with myopia from 0.50D to 5.00D and with-the-rule astigmatism from -1.25D to -3.50D found that, after one year of therapy, the axial elongation in subjects wearing toric ortho-k lenses increased by an average of 0.15mm.10 This was 58% slower than the control group, all of whom wore spectacles. After two years of therapy, the axial elongation in the toric ortho-k group increased by 0.31mm, 52% slower than the control group.10
In another study—comprised of 24 treated patients without a control group—researchers noted no myopia progression and no alteration in the axial length in myopic children ages nine to 16 after one year of toric ortho-k lens wear.11
 |
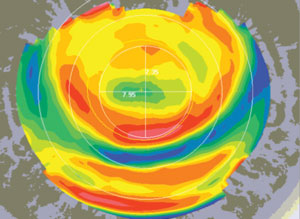 |
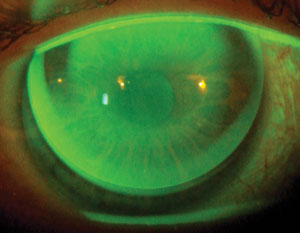
| Figs. 1a and 1b. Above, superior decentration of a spherical ortho-k lens on a toric cornea with no corneal touch in the steepest meridians. Below, the topography pattern of the same lens shows a decentrated treatment zone forming a ‘smiley face’ pattern. |
Clinical Need
Ortho-k treatment with spherical reverse geometry lenses presents two significant problems for patients with astigmatism, limiting their use to with-the-rule astigmatism up to 1.50D and against-the rule and oblique astigmatism up to 0.75D.12-15
First, a spherical accelerated ortho-k lens on a toric cornea will have poor centration because the lens’s sagittal depth is equal in each meridian and the cornea’s sagittal depth is different in each meridian. This leads to ‘smiley face’ (high ride) or ‘frowny face’ (low ride) topography patterns, induced astigmatism, glare and poor vision (Figures 1a and 1b).16-19 As a result, symmetric reverse ortho-k designs can only flatten the flattest meridian, which may actually cause the astigmatism to increase.16 A toric ortho-k design will extend the bearing area of the lens circumferentially to improve both lens fit and clinical outcome.
Second, spherical reverse geometry lenses cannot achieve the peripheral touch necessary to ensure stabilization, centration and properly modulated hydrodynamic forces. Ortho-k treatment is achieved by combining two pressures: the positive push force in the central cornea and the negative pull force in the mid-peripheral cornea.20 The negative fluid pressure necessitates a 360° total touch in the landing zone to prevent fluid outflow along the steepest meridian (Figures 2a and 2b).21 Therefore, the total peripheral touch is important not only for better lens stabilization and centration, but also to modulate the hydrodynamic forces that lead to corneal flattening in each meridian.16 In case of limbus-to-limbus astigmatism, the semi-closed, fluid-filled system in the reverse zone is achieved only with a toric ortho-k design.21
When to Fit Toric Ortho-k
Corneal astigmatism can be classified as apical, limbus-to-limbus or peripheral.22 In the apical form, astigmatism is greater centrally than peripherally. In limbus-to-limbus, central and peripheral astigmatisms are equal. Finally, in the third category, astigmatism is greater peripherally than centrally. The evaluation between corneal and refractive astigmatism can either be equal or different.22
Research suggests toric ortho-k lenses be used for apical astigmatism, measured with a corneal topographer, higher than 1.75D, limbus-to-limbus astigmatism higher than 1.25D and peripheral astigmatism higher than -1.00D.22 Using the toric back optic zone is recommended for corneal astigmatism that differs from refractive astigmatism. If the axes of corneal and refractive astigmatism do not coincide, the optical and the alignment zones require different axes.22
A recent study suggests toric ortho-k use may be beneficial when the sagittal height differential between the two principal meridians is greater than 25μm, or 1.00D of toricity.23 This might be better managed with a toric ortho-k design, especially for toric corneas. The majority of eyes looked at in the study had a peripheral astigmatism greater than central astigmatism.
Different Designs
Since their first introduction at the Global Orthokeratology Symposium in 2005 for the correction of astigmatism, toric ortho-k lens designs have varied across studies and case reports.10,13,16,18,21, 24-28
Clinical Studies
A study involving patients with astigmatism greater than 1.25D at any principal corneal meridian orientation used a lens design containing five toric zones, with reverse curves in the second and the fourth.21 This design is known as the “full toric double reservoir.” The researchers suggested that to achieve an adequate effect with a toric ortho-k lens, mechanical and hydrodynamic forces must occur differently in each corneal meridian, with greater flattening in the meridian where the myopia is greater. Results demonstrated an 85% change in initial astigmatism.21
An additional study, with subjects age nine to 16, used a design with reverse and alignment toric zones, which are more appropriate for toric corneas because they allow for better centration.11 The corneal astigmatism was gradually decreased, resulting in a success rate of 92.8%.11 This suggests that toric ortho-k designs are able to reduce moderate-to-high corneal astigmatism.
 |
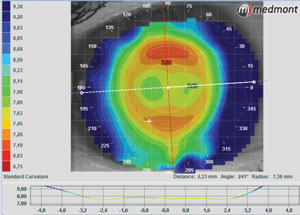 |
| Figs. 2a and 2b. On top, a toric ortho-k lens on a toric cornea showing 360° total touch in the landing zone. Below, the topography pattern of the same lens shows a centered flattening treatment zone. |
Case Reports
One case report used a toric alignment zone and spherical back optic and reverse zone for a 13-year-old patient with spectacle correction of -4.25 -1.50x165° OD and -4.25 -2.50x180° OS.18 According to the report’s authors, the advantage of placing a spherical optic zone on a toric cornea is that the flattest lens meridian creates a normal ortho-k effect while the steepest meridian results in a greater ortho-k effect—leading to the correction of the corneal astigmatism. Other case reports used the same design, as did the first studies on toric ortho-k lenses for astigmatism.10,13,26 These studies demonstrated a 95% toric ortho-k first lens fit success rate in correcting low-to-moderate myopia in children with moderate-to-high astigmatism, which was better than the trial lens rate of 73.5%, as well as a reduction in the axial elongation amount.10,13
In another case report, of a 22-year-old patient presenting with -4.25 -3.75x8° OD and corneal astigmatism of -3.10x7°, the authors fit a reverse ortho-k lens with two toric zones: the reverse and the landing.16 The correction of high corneal astigmatism needs a perfectly closed reverse zone in each meridian to properly modulate the hydrodynamic forces, allowing for separate corneal flattening in each meridian. At two months post-treatment, the patient’s corneal astigmatism was largely reduced, and the subjective correction was cyl -0.50Dx8° with uncorrected visual acuity (VA) of 20/20.16
One case report used a hexacurve (i.e., six back curves) design with two back toric zones, as well as optic and landing zones for a 44-year-old patient with mixed astigmatism in which the cylindrical component was greater than the spherical, the patient presented with + 1.00 -2.00x180° OD and +1.25 -2.25x180° OS.27 The vertical meridian was steeper than the horizontal meridian in the midperipheral landing zone and vice versa in the optical zone. Three months after ortho-k fitting, the subjective correction was +0.50 -0.50x10° (uncorrected VA of 20/16) OD and +0.25 -1.00x5° (uncorrected VA 20/16) OS.
In a more recent case report, a 48-year-old female presented with -0.75 -2.50x170° add 1.50D OD and -1.50 -1.50x20° add 1.50D OS.28 Her best-corrected VA was 20/16 in both eyes. The patient’s cylindrical component was three times larger than the spherical component in the right eye, while the two were equal in the left eye. Also, she had refractive astigmatism higher than corneal astigmatism (i.e., -1.82D OD and -1.39D OS) and low eccentricity. The lens fit was a tetracurve toric with optical, reverse and landing zones. According to the author, having the cylindrical component three times higher or equal to the spherical component and the refractive astigmatism greater than the corneal astigmatism was necessary for the toric optical zone. The toric reverse and alignment zones promoted the negative and hydrodynamic forces needed for treatment, better stability and centration of the lens.
While these reports are not conclusive, they do illustrate that various designs have proven useful for specific patients presenting with-the-rule, against-the-rule or oblique in any axis astigmatism up to -4.00D. Additionally, they show that possibilities exist for correction of different corneal and refractive toricity, as well as limbus-to-limbus astigmatism.
Having a wide range of toric ortho-k lens designs available expands the therapeutic options for the vast majority of patients. Practitioners can also design their own lenses, whether through contact lens fitting simulations in free style upon the corneal map with topography; empirical fitting software using keratometry and eccentricity through topography and refraction data; or downloadable topography software.
Evidence suggests children and adolescents with astigmatisms up to 4.00D in all directions, even limbus-to-limbus, can benefit from ortho-k and myopia control, as toric ortho-k lenses have proven to be efficient in reducing moderate-to-high astigmatism and slowing axial elongation.22
Dr. Fadel is an optometrist specializing in contact lenses for irregular cornea, scleral lenses and orthokeratology. She has a contact lens private practice in Italy, where she designs special customized contact lenses. She lectures and publishes, especially on contact lenses for the irregular cornea, scleral lenses and ortho-k. She is the founder and president of the Italian Academy of Scleral Lenses, a board member of the Italian Academy of Contact Lenses and a member of the Scleral Lens Society. Email: [email protected].
1. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-42.
2. Holden BA, Jong M, Davis S, et al. Nearly 1 billion myopes at risk of myopia-related sight-threatening conditions by 2050 - time to act now. Clin Exp Optom. 2015;98:491-3.
3. Walline JJ, Rah MJ, Jones LA. The children’s overnight orthokeratology investigation (COOKI) pilot study. Optom Vis Sci. 2004;81:407–13.
4. Cho P, Cheung SW, Edwards M. The longitudinal orthokeratology research in children (LORIC) in Hong Kong: a pilot study on refractive changes and myopic control. Curr Eye Res. 2005;30:71–80.
5. Kakita T, Hiraoka T, Oshika T. Influence of overnight orthokeratology on axial elongation in childhood myopia. Invest Ophthalmol Vis Sci. 2011;52:2170–4.
6. Zhu MJ, Feng HY, He XG, et al. The control effect of orthokeratology on axial length elongation in Chinese children with myopia. BMC Ophthalmol. 2014;14:141.
7. Li SM, Kang MT, Wu SS, et al. Efficacy, safety and acceptability of orthokeratology on slowing axial elongation in myopic children by meta-analysis. Curr Eye Res. 2016;14:600-8.
8. He, M, Du, Y, Liu, Q, et al. Effects of orthokeratology on the progression of low to moderate myopia in Chinese children. BMC Ophthalmology. 2016;16:126.
9. Young G, Sulley A, Hunt C. Prevalence of astigmatism in relation to soft contact lens fitting. Eye Contact Lens. 2011 Jan;37(1):20–5.
10. Chen C, Cheung SW, Cho P. Myopic control using toric orthokeratology (TO-SEE study). Invest Opthalmol Vis Sci. 2013;54:6510–7.
11. Luo M, Ma S, Liang N. Clinical efficacy of toric orthokeratology in myopic adolescent with moderate to high astigmatism. Eye Sci. 2014 Dec;29(4):209-18.
12. Ruston D, Van Der Worp E. Is ortho-k ok? Optometry Today. 2004 Dec;17:25-32.
13. Chen CC, Cheung SW, Cho P. Toric orthokeratology for highly astigmatic children. Optom Vis Sci. 2012;89:849-55.
14. Mountford J, Pesudovs K. An analysis of the astigmatic changes induced by accelerated orthokeratology. Clin Exp Optom. 2002;85:284–93.
15. Cheung SW, Cho P, Chan B. Astigmatic changes in orthokeratology. Optom Vis Sci. 2009;86:1352–8.
16. Baertschi M, Wyss M. Correction of high amounts of astigmatism through orthokeratology. A case report. J Optom. 2010;3:182-4.
17. Chan B, Cho P, Cheung SW. Orthokeratology practice in children in a university clinic in Hong Kong. Clin Exp Optom. 2008;91:453–60.
18. Chan B, Cho P, De Vecht A. Toric orthokeratology: a case report. Clin Exp Optom. 2009;92:387-91.
19. Mountford J, Pesudovs K. An analysis of the astigmatic changes induced by accelerated orthokeratology. Clin Exp Optom. 2002;85:284–93.
20. Mountford J, ed. Orthokeratology: Principles and Practice. Oxford: Butterworth Heinemann; 2004;69–107.
21. Pauné J, Gardona G, Quevedo L. Toric double reservoir contact lens in orthokeratology for astigmatism. Eye Contact Lens. 2012;38:245-51.
22. Pauné J. From bowtie to casual: dealing with toric corneas in ortho-k. Lecture at GSLS, January 21-24, 2016; Las Vegas, NV.
23. Kojima R, Caroline P, Morrison S, et al. Should all orthokeratology lenses be toric? Poster presented at GSLS, January 21-24, 2016; Las Vegas, NV.
24. Baertschi M. Short and long term success with correction of high astigmatism in OK. Lecture at the Global Orthokeratology Symposium, July 28-31, 2005; Chicago, IL.
25. Beerten R, Christie C, Sprater N, Ludwig F. Improving orthokeratology results in astigmatism. Poster presented at the Global Orthokeratology Symposium, July 28–31, 2005, Chicago, IL.
26. Chen C, Cho P. Toric orthokeratology for high myopic and astigmatic subjects for myopic control. Clin Exp Optom. 2012;95:103–8.
27. Calossi A. Mixed astigmatism treated with a dual-toric ortho-k design. Contact Lens Spectrum. 2013 Feb;28:49.
28. Fadel D. Unusual clinical cases in orthokeratology. Review of Cornea & Contact Lenses. Jun, 2016:22-27.


