A 50-year-old Caucasian female presents to the clinic reporting that she is tired of her reading glasses. She has perfect ocular health, no distance vision complaints and a distance manifest refraction of -0.5D in both eyes. She wants to know what her options are to reduce her dependence on reading glasses. This scenario is not unusual, and with the recent increased interest in reducing reading spectacle dependence, it will become even more common.
Traditional surgical approaches of monovision with laser-assisted in situ keratomileusis (LASIK), photorefractive keratectomy (PRK) or intraocular lenses (IOLs) following a refractive lens exchange are reasonable options. Contact lenses are less of a commitment than surgery but have downsides of their own. With presbyopia affecting an estimated 1.04 billion people worldwide, options continue to emerge and introduce new advantages.1
Among the newer additions for presbyopic correction are corneal inlays, which feature their own unique array of benefits and limitations. This article focuses on corneal inlays in the marketplace and how they are making a difference in the lives of presbyopic patients.
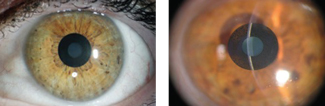 |
| Kamra inlays, shown here, are implanted into a corneal pocket made with a femtosecond laser. Photos: Vance Thompson, MD |
Inlays Today
Corneal inlays have a variety of mechanisms of action, including index of refraction change, corneal curvature change and small-aperture optics.2 They are most often placed in the nondominant eye, but–unlike in monovision–a significant decrease in distance visual acuity does not occur in that eye. This allows for continual good binocular vision, which means little to no decrease in stereoacuity.3,4 Other benefits of corneal inlays include removal and repositioning abilities, and since the procedure is limited to the cornea, risks associated with intraocular procedures are not a concern.
Corneal inlay implantation is achieved with the assistance of a femtosecond laser, which helps create a dependable stromal pocket or flap where the inlay is placed. This improves the accuracy of the depth at which it is implanted, as well as centration.5,6 Creating a pocket has several advantages over a flap, such as saving peripheral corneal nerves (which maintain corneal sensation and reduce the incidence of dry eye) and preservation of corneal biomechanical stability.6,7
Research reports glare and halos in the early postoperative period, but these tend to become less intense during follow-up visits.7,8 The literature also shows a loss of contrast sensitivity, something that is believed to occur because of increased total higher-order aberrations (HOAs).7,8 An increase in HOAs can also occur with slight decentration of the corneal inlay.7,8
Preoperatively, examining for and identifying dry eye disease is crucial when preparing a patient for a corneal inlay procedure. The cornea makes up two-thirds of the refractive power of the eye, so if the ocular surface is not healthy, especially in a unilateral procedure, the image quality will be degraded, resulting in a loss of quality of vision that cannot be compensated for with the fellow eye.
Here is a closer look at some specific cornea inlays:
Kamra. Using a small aperture to increase depth of field in a patient’s nondominant eye, the Kamra corneal inlay (AcuFocus) was FDA approved in 2015. The 1.6mm aperture in the central optical zone acts as a pinhole, blocking peripheral rays of light to enhance depth of focus.9 The inlay is 5µm thick and has an outer diameter of 3.8mm.9 Its design maintains metabolic flow—holes or “fenestrations” in the disc allow movement of nutrients—and continued hydration of the cornea, which prevents epithelial decompensation and corneal thinning.10
The Kamra inlay can be used in emmetropes, post-LASIK emmetropes, in pseudophakic patients or combined with LASIK correction, but the ideal patient to consider for the procedure is one with refraction between plano and -0.75D, as well as astigmatism less than 0.75D.10,11 The procedure involves implanting the inlay into a corneal pocket made with a femtosecond laser at a depth of 250µm or, if previous LASIK has been performed, at least 100µm below the LASIK flap.
Complications of the Kamra inlay are consistent with those typical for any refractive procedure. There have been reports of corneal epithelial iron deposits and haze that is visually significant.10 When these cases are caught early enough, the inlay can be removed with no loss of corrected visual acuity.11,12 In patients with light-colored irides, the implant can be visible to the naked eye from an angle; in most other patients, visualization is negligible.
Research has shown improved near vision, stable or improved intermediate vision and stable or mildly worsened distance vision in the implanted eye.12 A recent study of 50 eyes with Kamra inlays showed significant improvement of uncorrected near visual acuity (UNVA) from J8 to J2 and median uncorrected distance visual acuity (UDVA) improved from 20/32 to 20/22 at 12 months.12 Complications were minimal and only included one implant removal due to unsatisfactory UNVA and UDVA as well as slight corneal haze.12 There was no loss of best-corrected distance visual acuity after removal.12
Raindrop Near Vision. Another FDA-approved option is the corneal-reshaping Raindrop Near Vision inlay (ReVision Optics). The Raindrop is a 30µm-thick permeable hydrogel lenticule. It allows natural nutrient flow, has no refractive power itself and expands depth of focus by increasing central cornea curvature.13,14 Because the inlay makes a hyperprolate corneal shape and features epithelial remodeling, a multifocal cornea is created.13,14 This improves both near and intermediate vision.13,14 Distance visual acuity remains largely unchanged as light rays pass paracentral to the 2mm diameter of the inlay and remain focused on the retina.2
Through the use of a femtosecond laser, the Raindrop is inserted under a LASIK flap or corneal pocket at a shallow depth of 120µm to 130µm in the nondominant eye.2
Like the Kamra inlay, the Raindrop can be repositioned or removed if necessary.15 Complications related to this inlay include blurred vision, glare and halo.15
In a study of 373 presbyopic subjects implanted with the Raindrop in the nondominant eye, results showed UNVA improved by five lines, uncorrected intermediate visual acuity (UIVA) improved by 2.5 lines and UDVA decreased by 1.2 lines at a one-year follow up.15 From three months through one year, 93% of subjects achieved UNVA of 20/25 or better, 97% achieved UIVA of 20/32 or better and 95% achieved UDVA of 20/40 or better.15 Binocularly, the mean UDVA exceeded 20/20 from three months through one year.15 Eleven cases required inlay explantations, but all of those patients achieved a corrected distance visual acuity of 20/25 or better by three months after explant.15
Flexivue Microlens Inlays. Designed to change the refractive index of the cornea, the Flexivue Microlens (Presbia) is a refractive optic corneal inlay that provides distance vision through a central plano zone surrounded by one or more rings of varying additional powers for intermediate and near vision.6,16 The Flexivue is a transparent, 3mm-diameter hydrogel implant with a 0.15mm opening to allow nutrient flow and oxygen transfer.7 The opening is surrounded by an optically neutral central zone and a refractive peripheral zone that has add powers between +1.25D and +3.5D in +0.25D increments.7 The Flexivue is placed in a femtosecond-created corneal pocket at a depth of 280µm to 300µm.2 Changes to the corneal topography are usually not seen due to the depth at which the inlay is placed.2
The Flexivue Microlens received a “Conformité Européene” mark, which represents standards of safety, health and environmental protection met for marketability in the European Economic Area, in 2009 and is currently undergoing FDA clinical trials in the United States. In a prospective study of 47 emmetropic presbyopes with a Flexivue Microlens inserted inside a corneal pocket in the nondominant eye, UNVA was 20/32 or better in 75% of operated eyes 12 months after surgery, and mean UDVA decreased three lines from 20/20 preoperatively to 20/50 postoperatively.7 Mean binocular UDVA was not statistically significantly affected, and there were no postoperative complications noted, as well as no inlay explantation or replacement.7 Patient satisfaction and spectacle independence was high, but 12.5% of patients experienced halos and glare at one year.7
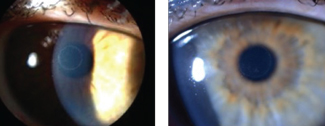 |
| Through a hyperprolate corneal shape and epithelial remodeling, Raindrop Near Vision Inlays, shown here, create a multifocal cornea. Photos: Vance Thompson, MD |
Postoperative Management
Managing a patient with an inlay postoperatively differs from managing a LASIK patient postoperatively. The healing time is longer, and it generally takes one to three months for complete visual recovery. Patients should be made aware of probable fluctuations in vision and halo or glare secondary to mild corneal edema during the initial healing period. As a result, it is important to place them on a broad-spectrum antibiotic for one week and a topical corticosteroid tapered over a three-month period. Also, make sure to check intraocular pressure at each follow-up visit, as patients are at risk for pressure spikes secondary to the topical corticosteroid use.
If any signs of ocular surface disease exist, aggressive treatment should be initiated immediately. The inlay and cornea need to be examined closely for areas of irregularity, damage, epithelial ingrowth, stromal inflammation and striae. An increase in corticosteroid treatment will be needed in the case of any haze formation. Frequent manifest refractions should be performed to monitor for hyperopic shifts or myopic shifts that could indicate a central steepening or flattening over the inlay. These occur as a result of tear film irregularities caused by ocular surface disease or corneal haze.
How Do They Hold Up?
Corneal inlays are a relatively new treatment option competing directly against lens-based surgeries such as multifocal IOLs, accommodating and enhanced depth of focus IOLs, and monovision approaches such as LASIK or PRK—not to mention the externally worn corrective lens options of multifocal contact lenses, progressive addition spectacle lenses and simple reading glasses.
Advantages of corneal inlays over traditional monovision correction and lens-based surgeries include improved UNVA and maintained or improved UIVA, as well as minimal effects on UDVA, contrast sensitivity and stereoacuity. There are also fewer risks associated with corneal inlay surgery compared with lens-based surgery, as corneal inlay surgery is limited to the cornea.
Corneal inlays are not without their disadvantages, such as unpredictable wound healing and tear film health. The procedures is not covered by insurance and patients pay out of pocket. As a result, patient selection and education is critical. A patient with a mild or early cataract is going to be better suited for a lens-based surgery, while a patient just entering presbyopia is likely better suited for a mild monovision correction. For corneal inlays to continue to be successful, there will need to be continual advancements in material biocompatibility with the cornea, reduced rates of complications, expanded indications beyond emmetropes/low myopes and continued attention to careful patient selection with predictable outcomes.
Dr. Schweitzer practices at Vance Thompson Vision in Sioux Falls, SD, and is an adjunct clinical professor at the Illinois College of Optometry.
1. Murphy SL, Xu JQ, Kochanek KD. Deaths: preliminary data for 2010. Natl Vital Stat Rep. 2012;60:30.
2. Greenwood M, Bafna S, Thompson V. Surgical correction of presbyopia: lenticular, corneal, and scleral approaches. Int Ophthalmol Clin. 2016;56(3):149-66.
3. Alarcon A, Anera RG, Villa C, et al. Visual quality after monovision LASIK. J Cataract Refract Surg. 2011;37:1629-35.
4. Linn S, Hoopes PC. Stereopsis in patients implanted with a small aperture corneal inlay. Invest Ophthalmol Vis Sci. 2012;53:1392.
5. Papadopoulos PA, Papadopoulos AP. Current management of presbyopia. Middle East Afr J Ophthalmol. 2014;21(1)10-7.
6. Binder P. New femtosecond laser software technology to create intrastromal pockets for corneal inlays. ARVO. 2010;51:2868.
7. Limnopoulou AN, Bouzoukis DI, Kymionis GD, et al. Visual outcomes and safety of a refractive corneal inlay for presbyopia using femtosecond laser. J Refract Surg. 2013;29:12-8.
8. Pallikaris IG, Bouzoukis DI, Kymionis GD, et al. Visual outcomes and safety of a small diameter intrastromal refractive inlay for the corneal compensation of presbyopia. J Refract Surg. 2012;28:168-73.
9. AcuFocus. Kamra Inlay. https://kamra.com/kamra-inlay/. Accessed July 24, 2017.
10. Dexl AK, Jell G, Strohmaier C, et al. Long-term outcomes after monocular corneal inlay implantation for the surgical compensation of presbyopia. J Cataract Refract Surg. 2015;41:566-75.
11. Yilmaz OF, Bayraktar S, Agca A, et al. Intracorneal inlay for the surgical correction of presbyopia. J Cataract Refract Surg. 2008;34:1921-7.
12. Jalali S, Aus der Au W, Shaarawy T. AcuFocus corneal inlay to correct presbyopia using femto-LASIK. One year results of a prospective cohort study. Klin Monbl Augenheilkd. 2016;233(4):360-4.
13. Garza EB, Gomez S, Chayet A, Dishler J. One-year safety and efficacy results of a hydrogel inlay to improve near vision in patients with emmetropic presbyopia. J Refract Surg. 2013;29(3):166-72.
14. Lang AJ, Holliday K, Chayet A, et al. Structural changes induced by a corneal shape-changing inlay, deduced from optical coherence tomography and wavefront measurements. Invest Ophthalmol Vis Sci. 2016;57(9):154-61.
15. Whitman J, Dougherty PJ, Parkhurst GD, et al. Treatment of presbyopia in emmetropes using a shape-changing corneal inlay: one-year clinical outcomes. Ophthalmology. 2016;123:466-75.
16. Arlt E, Krall E, Moussa S, et al. Implantable inlay devices for presbyopia: the evidence to date. Clin Ophthalmol. 2015;9:129-37.


