 |
Contact lenses, whether rigid or soft, are a foreign object on the ocular surface. They interact with the tear film, cornea, bulbar conjunctiva and palpebral conjunctiva; not surprisingly, complications may arise on any of these ocular structures as a result of contact. Additionally, the tear film is separated into a pre- and post- contact lens film with different thicknesses, which can initiate a variety of issues.1
3 and 9 o’clock Staining
A common complication with corneal GP lenses is 3 and 9 o’clock staining, which is a result of epithelial punctate staining of the peripheral cornea near the edge of the GP lens.2 These so-called 3 and 9 o’clock areas may not be adequately resurfaced with tears after a blink, thus resulting in small desiccated regions. At first the staining is mild, but over time the epithelial defects may become larger and denser. In severe cases, those portions of the cornea may become vascularized and even form an opacity.
When treating, be sure to check the edge of the contact lens first. If you have a modification unit within the office, you can alter the edge of the lens to be rounded or a “plus” shape to help with edge-cornea interaction.3 If your patient has a particularly high plus or high minus lens, be sure to use lenticular lens designs to improve the edge of the lens.4
Inferiorly centered GP lenses are another major cause of 3 and 9 o’clock staining, so improving the centration of the GP lens is key.3 Additionally, selecting a GP lens material with good wettability may help to decrease peripheral erosion by reducing friction between the lens and ocular surface. Artificial tears and gels can also help increase lubrication, but will need to be used consistently to prevent further complications.
If all other modifications fail, try altering the diameter of the lens. Smaller diameters may decrease 3 and 9 o’clock staining, though going larger is also an option. A scleral lens will resolve the issue completely because of the fluid layer between the cornea and the contact lens, which will act as a lubricating cushion between the lens and ocular surface. Switching the patient to a hydrogel material may also be an answer.
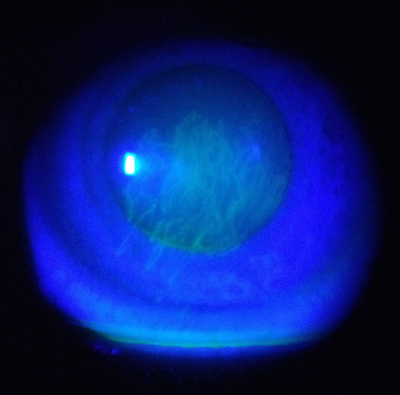 | |
| Fig. 1. Foreign body entrapment under GP lens shows track marks on the corneal epithelium. |
Foreign Bodies
Foreign body tracking—when dirt, dust or another small object adheres to the ocular surface and ends up underneath the lens—can be an extremely frustrating issue for both soft and GP lens wears alike.
Even the smallest foreign body can result in ocular surface damage, as with every blink, the trapped object scratches the delicate epithelium. This can lead to track marks, which are both very uncomfortable and potentially painful for the patient (Figure 1).
Lens edge design plays a major role regarding foreign body entrapment; for example, if the edge is poorly finished or has unpolished secondary curves, this can lead to more occurrences.5 Thus, rolling the edge and polishing the secondary curves can help reduce foreign body entrapment. Be sure to also check the edges for chipping, as it can also increase risk of foreign body entrapment.5 If the problem persists, consider switching to a larger diameter lens, such as a scleral lens, to reduce or eliminate this issue.
Spectacle Blur
Every once in a while, a patient comes in who complains that when they remove their contacts and put on their glasses, their vision is blurred. One reason this so-called spectacle blur may occur is from the accumulation of fluid within the epithelial cells. When contact lenses are removed, the swelling of these cells slowly decreases, and the spectacle blur usually resolves after an hour.6
Spectacle blur can also result from changes in corneal curvature that is not related to edema. This is due to mechanical molding of the cornea (resulting from lens fit) or prolonged metabolic stress. This issue is particularly common in patients who wear flat-fitting or hybrid lenses.
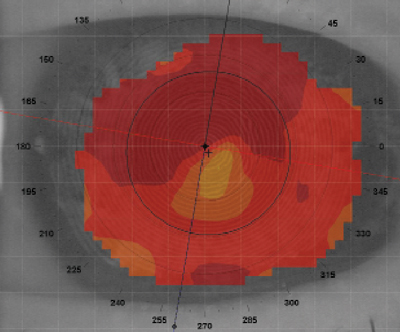 | |
| Fig. 2. Topography of a poorly fitting tangent streak GP lens caused corneal steepening. | |
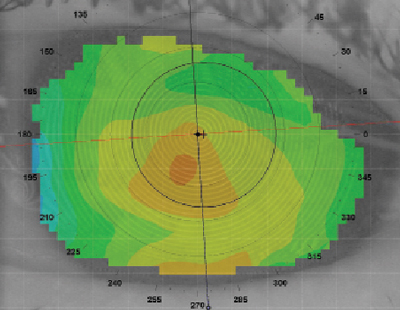 | |
| Fig. 3. Corneal topography after discontinuing GP lens wear for several months. |
In the case of corneal molding, when the fit of the contact lens is poor, the lens reshapes the cornea, thus resulting in spectacle blur (Figure 2). Spectacle blur is usually not a large issue, unless the primary cause is because the contact lens fit is inappropriate. For example, in more extreme cases, deep stromal striae or opacification of the cornea can be seen, which is indicative of further potential issues. In most cases, however, the cornea will eventually remold to a stable shape if the lens is removed (Figure 3).6 Regardless, education on spectacle blur and what to expect usually eases patients so they do not get upset or anxious.
Lens Adhesion
Lens adhesion is the most common complication of extended wear GP lenses.7,8 Upon examination, the lens will be immobile with mucous/lipid deposits present underneath. When fluorescein is instilled, none will be seen under the lens, indicating no tear exchange or lens movement. When the lens is removed, an arcuate ring pattern is visible around the edge of the lens.7 Patients usually do not have any complaints with lens binding; in fact, they may report better comfort (except late in the day) because of the decreased lid interaction and movement.
If an extended wear patient exhibits lens adhesion, changing their wearing schedule to daily wear will likely resolve the issue. During sleep, the pressure from the eyelids squeezes out the tear layer under the GP lens, which results in lens binding.7 If lens binding occurs with a daily wear patient, however, the fit of the lens will need to be altered. When the lens decenters, the secondary and peripheral curve junctions contact the flatter areas of the cornea.7,8 This, combined with pressure from the eyelids, leads to lens adherence. Try altering the centration and curvature of the lens to achieve a more centered fit and check to make sure the curves are well blended. If normal modifications do not work, consider switching to an aspheric back surface design.
Note that another potential cause of lens adherence is dry eye, specifically aqueous deficient dry eye, so it is important to check your patient for any type of dry eye during their exam.
1. Nichols J, King-Smith PE. Thickness of the pre- and post-contact lens tear film measured in vivo by interferometry. Invest Ophthalmol Vis Sci. 2003 Jan;44(1):68-77.
2. Van der worp E, de Brabander J, Swarbrick HA, Hendrikse F. Evaluation of signs and symptoms in 3 and 9 o’clock staining. Optom Vis Sci. 2009 Mar;86(3):260-5.
3. Holden T, Bahr K, Koers D, et al. The effect of secondary curve liftoff on peripheral corneal desiccation. Am J Optom Physiol Opt 1987;64:113.
4. Henry VA, Bennett ES, Forrest JM. Clinical investigation of the Paraperm EW rigid gas permeable contact lens. Am J Optom & Physiol Opt 1987;64:313-320.
5. Bennett, E. et al. Clinical Contact Lens Practice. Lippincott, Williams, and Wilkins. Philadelphia, PA. 2005. Pp 351.
6. Bailey SC. Contact lens complications. Optometry Today. June 4 1999.
7. Bennett, E. et al. Clinical Contact Lens Practice. Lippincott, Williams, and Wilkins. Philadelphia, PA. 2005. Pp 346-8.
8. Swarbrick HA, Holden BA. Rigid gas permeable lens binding: significance and lens factors. Am J Optom Physiol Opt. 1987;64(11)815-823.


