 |
Case Report
A five-year-old female presented for a contact lens evaluation to correct irregular astigmatism from a corneal scar. Her pediatric ophthalmologist referred her for a unilateral contact lens fit over an eye that had a corneal dermoid removed at age three. She was currently managed with glasses and was patched two hours per day with good compliance. Medical history was positive for Goldenhar syndrome and negative for systemic medications. She exhibited no other ocular history and neither did her family. Presenting best-corrected visual acuity (VA) was 20/20 OD, 20/50 OS. Her current spectacle Rx was -0.50+0.50 x168 OS: +3.00+3.75x070.
Pupils were round and reactive to light, with no relative afferent pupillary defect in either eye. Extraocular movements were full OU. A slit lamp exam demonstrated that the lids were clear, the conjunctiva white and quiet, the iris and lenses clear, and the anterior chamber deep and quiet OU. Exam of the corneal surface revealed a clear right cornea and an elevated 2.7mm horizontal inferior temporal scar on her left cornea—no staining or vessels OU. Manifest refraction OD was plano VA 20/20, OS was +4.25+5.50x075 VA 20/30-. Corneal topography revealed a flat cornea with steepening at the corneal scar (Figure 1). Sim K measured 46.17/40.62 OS and 5.62D of astigmatism.
Diagnostic Fitting
Although we started with a scleral lens due to the irregularity of the periphery, insertion was unsuccessful. The patient was very reactive and could not fixate her eyes so that the lens could be inserted without a bubble inside the lens. After several attempts, I decided to try a corneal gas permeable (GP) lens instead. I chose a large diameter intralimbal GP design (GBL, Concise) as the diagnostic lens. This lens also features a reverse geometry design in the mid periphery, which would allow it to clear the steep elevation in the mid periphery without adding too much clearance over the central cornea. I first tried a 45.00D (7.50) lens based off the average of the steeper curvature readings over the scar. The lens was slightly flat over the cornea scar with a somewhat tight edge and pooling superior nasal. Over-refraction resulted in VA of 20/25. I ordered the lens 0.75D steep to take the lens pressure off the scar with flatter peripheral curves than standard to assist in distributing the weight of the lens across the cornea.
First lens: Base curve 7.38, power: +3.25, diameter:11.2, P1:0.4/9, P2:0.4/10.5, P3:0.4/12.
Dispensing
The patient presented with her mother with no new complaints and I inserted the lens (Figure 2). The lens exhibited light one-third touch inferotemporally with pooling over the rest of the cornea. The peripheral edge was wide with good overall centration of the lens and movement with blink. VA measured 20/25 with the GP in place OD. The patient’s mother was instructed on care, insertion and removal, and advised to build wearing time, starting at two hours a day with the goal of eight to 10 hours a day.
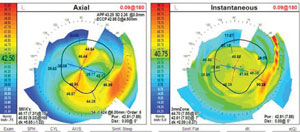 |
| Fig. 1. Topography of left eye. An overall flat cornea with inferior temporal steepening at the corneal scar. |
One week later, the patient presented with complaints that the lens hurt after a few hours of wear, and she was unable to wear it more than three hours per day. Some redness, but no discharge, was observed. Presenting VA was 20/25 OD with the contact lens. No over-refraction was measured. Fluorescein was instilled, and I observed that the lens had adhered to the cornea, exhibiting little movement and was decentered temporally over the scar. With the lens removed to evaluate the cornea, there was 1+ punctate staining over the corneal scar.
Modifying the GP would unlikely achieve better results, as opening the periphery to increase movement and increasing the vault over the scar would likely still result in the lens migrating towards the steep elevation of the scar. I decided to piggyback the GP with a soft lens.
I used a +3.00 Air Optix Night & Day (Alcon) to create a buffer between GP and eye. I chose a higher plus lens to aid in shifting the steep area centrally so the lens would decenter less. On slit lamp exam, the GP moved well over the soft lens. VA was 20/30. Over-refraction of the combined system (-0.50) would be added to the GP if the patient did well. I prescribed Polytrim (polymyxin B/trimethoprim, Allergan) for a few days to prevent infection and advised her to start lens wear after finishing the antibiotic course. Mom was again trained on insertion and removal and instructed to have her daughter wear the lens no more than four hours per day as long as the lens is comfortable.
Follow-Up #2
The patient presented the next week. Though lens tolerance was much improved, she didn’t think she could wear it more than four hours per day, as she needed frequent lubrication with artificial tears. On slit lamp exam and instillation of fluorescein, the lens was again decentering temporally with little movement. When the lens was removed, no staining was observed. Other than the scar, the cornea was clear.
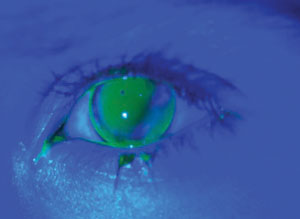 |
| Fig. 2. GBL lens on first dispense. Note the light touch of the lens over the area of the corneal scar. |
Because any GP would most likely shift towards the elevation, we discussed using a scleral lens again and I performed an in-office evaluation, during which the patient was very cooperative. I used a Europa (Visionary Optics) fitting set and chose a 45.00D/16.0 diameter lens as the first diagnostic lens simply because it was in the middle of the set. Upon insertion, the child noted an immediate improvement in comfort.
Slit lamp exam revealed excessive clearance of about 450μm. When I tried a 42D lens, it exhibited about 200μm of central clearance on initial evaluation, which was ideal. The lens landed outside the limbus and centered well. The periphery appeared tight, exhibiting slight conjunctival vessel compression. Given the child’s positive initial reaction, I ordered a 42.50/+6.25/16.0 diameter, 1 flat periphery lens to be dispensed the next week. The base curve was slightly steepened to compensate for the change in the sagittal depth with a 1 flat periphery.
Scleral Lens DispenseAt the second lens dispense a week later, the patient hadn’t been wearing any lenses for the past week. The scleral lens cleared the central cornea by about 200μm. The fluorescein extended from limbus to limbus and the lens landed on the conjunctiva without impinging on the sclera. VA was 20/25 OS. Mom was trained on insertion, removal and care. The patient was instructed to return the following week.
Follow-Up #3
One week later, the patient said she was able to wear the lens for 10 hours a day without any complaint (Figure 3). Uncorrected VA measured 20/20 OD and 20/25 OS. No over-refraction was noted over the left lens. The lens was finalized and the patient was asked to return in six months for a follow-up.
Discussion
Several studies show that vision rehabilitation of irregular astigmatism or high refractive error with contacts lenses is more effective than spectacles.1-4 GPs are able to correct irregular astigmatism as well as eliminate the aniseikonia from unequal prescriptions when the irregularity is unilateral.5,6 For children, the high oxygen material of the lenses combined with involving the parents in the care lowers the risk for contact lens complications.7
 |
| Fig. 3. Scleral lens in place at first follow-up. A white and quiet eye after eight hours of successful wear. |
Using a soft approach is ideal, and you should always tell the child what you are doing and why. If you can, show them that you and their parents wear contact lenses. If a child is particularly resistant to anything being inserted in the eye, send them home with artificial tears or even a soft contact lens to practice. This will help acclimate the child to the task, as with this patient.
The process of fitting a contact lens can vary from child to child. With younger or less cooperative children, GP diagnostic lenses of known base curves and their fluorescein patterns can help determine corneal curvature.
To fit a corneal scar, the fluorescein pattern of an GP should exhibit two-thirds pooling and one-third light touch over the entire cornea. The lens should center well and move adequately to provide tear exchange for optimal corneal health. In cases where GPs fail, sclerals can be effective, as they are tolerated well in the pediatric population.10,11 The lens can often compensate for GP issues such as ocular surface disease, decentration or intolerance.12
Education is Essential
Despite vision improvement for most children, studies indicate a contact lens dropout rate as high as 36.8% in patients with unilateral irregular astigmatism.13 To help avoid this, clinicians should ensure parent buy-in and educate them on why the contact lens is necessary. They also need to understand the risk of amblyopia and why a contact lens is preferable to a spectacle correction.
Additionally, the process of acclimating a child to lens wear can be emotionally taxing on the parents, and they need to be reassured they are not hurting their child. Spending time on this conversation is essential to the child’s visual success.
For children with irregular astigmatism or high refractive error, vision rehabilitation should begin right away to prevent amblyopia. This case emphasizes the importance of using your full arsenal of contact lens options to address the different needs of each child.
1. Luo W, Tong JP, Shen Y. Rigid gas permeable contact lens for visual rehabilitation in aphakic following trauma. Clin Exp Optom. 2012;95:499-505.
2. Pieramici DJ, Sternberg P Jr, Aaberg TM Sr, et al. A system for classifying mechanical injuries of the eye (globe). The Ocular Trauma Classification Group. Am J Opthalmol. 1997;123:820-31.
3. Netto AL, Fioravanti Lui AV, Fioravanti Lui GA. Visual rehabilitation with contact lenses after ocular trauma. Arq Bras Oftalmol. 2008;71:23-31.
4. Lin PW, Chang HW, Lai IC, Teng MC. Visual outcomes after spectacles treatment in children with bilateral high refractive amblyopia. Clin Exp Optom. 2016;99:550-4.
5. Jupiter DG, Katz HR. Management of irregular astigmatism with rigid gas permeable contact lenses. CLAO J. 2000;26:14-7.
6. Kanpolat A, Ciftci OU. The use of rigid gas permeable contact lenses in scarred corneas. CLAO J. 1995:2.
7. Shaughnessy MP, Ellis FJ, Jeffrey AR, Szcotka L. Rigid gas permeable contact lenses are a safe and effective means of treating refractive abnormalities in the pediatric population. CLAO J. 2001-27:195-201.
8. Pradhan Z, Mittal R, Jacob P. Rigid gas-permeable contact lenses for visual rehabilitation of traumatized eyes in children. Cornea. 2014;33:486-9.
9. Walters JL, Paules MG. Review of preclinical studies on pediatric general anesthesia-induced developmental neurotoxicity. Neurotoxicology and Teratology. 2016 Nov 18. [Epub ahead of print].
10. Rathi V, Mandathara P, Vaddavalli P, et al. Fluid filled scleral contact lens in pediatric patients: Challenges and outcome. Contact Lens and Anterior Eye. 2012;35(4):189-92.
11. Gungor I, Schor K, Rosenthal P, Jacobs DS. The Boston scleral lens in the treatment of pediatric patients. J AAPOS. 2008:12(3):263-7.
12. Pullum KW, Whiting MA, Buckley RJ. Scleral contact lenses: the expanding role. Cornea. 2005:24(3):269-7.
13. Ozkan B, Elibol O, Yuksei N, et al. Why do patients with improved visual acuity drop out of GP contact lens use? Ten year follow-up results in patients with scarred corneas. Eur J Opthalmol. 2009:19:343-7.


