 |
Case
A 54-year-old female scleral lens wearer with a history of dry eye and s/p LASIK OU presented with complaints of constant lens fogging. Her medical history was positive for allergic rhinitis. She had no significant family history. Her medications included Flonase (GlaxoSmithKline) and Zyrtec (AstraZeneca), omega-3 fish oil supplements and Restasis (Allergan).
She reported that her scleral lenses fogged “constantly” and she had to remove and rinse them several times a day. For this reason, she limited her wear to three to four hours at night when her vision was at its worst. She would clean her lenses with Boston Advance cleaner (Bausch + Lomb) at night, store the lens in Boston conditioner and fill the lenses with Unisol 4 (Alcon) before insertion. Her presenting visual acuity in spectacles was OD -2.50 +0.50x067 VA 20/25- and OS -1.50 +1.00x118 VA 20/25- +2.00 add J1 OU.
Her pupils were round and reactive to light, with no relative afferent pupillary defect in either eye, and her extraocular movements were full OU. A slit lamp examination revealed clear lashes and 1+ inspissated meibomian glands bilaterally. Punctal plugs were in place in the inferior puncta OU. Examination of the corneal surface revealed 1+ inferior punctate staining, a tear break-up time of two seconds and a low tear lake OU.
The conjunctiva was white and quiet, irides and lenses were clear, and the anterior chamber was deep and quiet OU. Her intraocular pressure was 12mm Hg OU. Undilated posterior segment evaluation revealed a normal fundus OU with trace nuclear sclerosis OU.
Manifest refraction OD was -2.75 +0.50x060 VA 20/25 and OS -1.00 +0.50x118 VA 20/25 +2.25 add near acuity J1 OU. Topographical evaluation of the cornea revealed flat, plateau-shaped corneas OU and simulated keratometry read OD 36.76/34.23 at 175, OS 35.60/34.33 at 124 (Figure 1).
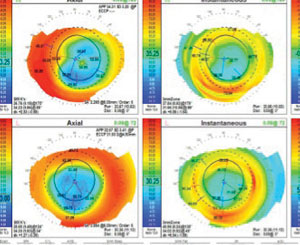 |
| Fig. 1. Flat plateau shape indicating post refractive surgery OU. |
Contact Lens Evaluation
The patient’s presenting contact lens parameters, measured in office, were OD 8.0BC/-11.00/15.7 CT 0.3mm diameter VA 20/20- and OS 8.0BC/-10.25/15.7 CT 0.3mm diameter VA: 20/25-. Once she inserted her lenses, we instilled fluorescein to evaluate the fit. The fluorescein immediately entered the lens chamber at 10 o’clock in the right eye and two o’clock in the left eye, completely filling the lens within 10 seconds of instillation. Each time the patient blinked, fluorescein pumped into the lens chamber of both eyes along with mucous strands from the patient’s eye. The lenses were visibly flexing with each blink. This, combined with the fact that the patient had an apparent toric sclera, was causing tear film debris to be pumped into the lens.
Diagnostic Contact Lens Fitting
For the patient’s diagnostic contact lens fitting, we used a Europa (Visionary Optics) scleral fitting design. Since she was post refractive surgery, the first diagnostic lenses used were slightly flatter than average. A 42D/16.0 diameter lens was chosen for her right eye and a 43D/16.0 lens was chosen for her left eye, both of which were of standard spherical periphery.
Fluorescein was instilled and the lenses immediately filled with dye from the superior temporal edge of each lens (Figure 2).
The right lens exhibited 250μm of central corneal clearance, while the left lens was roughly 350μm. Both lenses had adequate limbal clearance, but excessive superior and inferior edge lift, causing the lens to move along the vertical meridian. The over-refraction of both lenses brought the vision to 20/20 OU.
To reduce lens flexure, we increased the center thickness of the lenses. A 2D toric periphery was added to both lenses to align them to the conjunctiva, create tighter seals and reduce lens movement. The initial lens measurements were OD 42.00/-11.25/16.0 2D toric periphery center thickness 0.35mm and OS 42.00/ -9.25/16.0 2D toric periphery center thickness 0.35mm.
Finally, we addressed inferior band staining, which was likely due to nocturnal lagophthalmos. We advised the patient to add to her care regimen a gel tear at night and again in the morning, consider taping the lids to sleep and continue using Restasis OU. We also advised her to be diligent with daily lid hygiene and warm compresses.
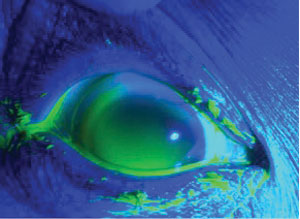 |
| Fig. 2. Immediate fluorescein uptake in a scleral lens with spherical peripheral landing on a toric sclera. This was taken just after fluorescein instillation. |
Follow-Up #1
The patient presented for a dispensing visit two weeks later. She reported that her eyes felt less dry in the morning as a result of the gel tears. When we inserted the lenses with fluorescein, they exhibited central 250μm of clearance OU on the initial insertion with good limbal clearance and centration. The right lens had slightly excessive superior edge lift and moved easily when the lid was pushed up. The left lens was aligned to the conjunctiva with minimal movement. The patient’s vision was measured at 20/20 OU with no over-refraction. We advised the patient to switch to a peroxide-based solution and use preservative-free sodium chloride to fill the lens.
Follow-Up #2
At her next follow-up a week later, the patient had noticed a 50% improvement in fogging in the right eye and about 75% improvement in the left eye. She was able to wear the lenses for 10 to 12 hours a day while only rinsing them once or twice. Her right lens would become foggy faster than the left lens, however. A slit lamp examination revealed mild surface debris on the outside of both scleral lenses and some tear debris inside the chamber of the right lens. The central clearance was estimated at about 150μm to 200μm. After instilling, the right lens filled completely in 20 to 30 seconds, while the left lens did not fill within a one-minute period (Figure 3).
The left lens was finalized, but we recommended 3D of peripheral toricity in the right lens to reduce movement and improve alignment to the conjunctiva. We advised the patient to add Progent cleaner (Menicon) to her cleaning regimen every two weeks and remove surface debris with a moistened cotton swab or wipe the lens with a plunger edge midday instead of removing the lenses.
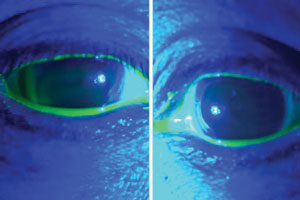 |
| Fig. 3. OD: Fluorescein slowly trickling in superior temporal. OS: No uptake. Image captured 15 seconds after fluorescein instillation. |
Follow-Up #3
After another two weeks, the patient presented with no new complaints. She was removing her right lens two times a day to clear fog and cleared the surface debris on the left lens with a cotton swab. We placed the new right lens into the left eye to evaluate. A slit lamp examination revealed central 250μm clearance, and the lens did not move with blink. We then added fluorescein into the lens and there was no uptake within one minute of instillation (Figure 4). Her vision measured 20/20 OS. We sent her home with the new lens to try.
Follow-Up #4
One week later, the patient was able to wear both lenses successfully with significantly less mid-day fogging. Occasionally she would have to remove the lenses to rinse the debris off, but most of the time she was able to wear the lenses all day without refreshing the fluid and she was happy with her vision and comfort. Her finalized contact lens prescription was OD 42.00/ -11.25/16.0 3D toric periphery center thickness 0.35mm and OS 42.00/-9.25/16.0 2D toric periphery center thickness 0.35mm.
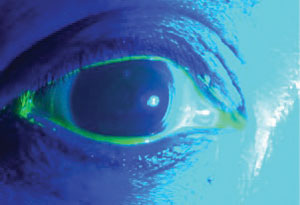 |
| Fig. 4. Scleral lens sealed off from fluorescein entry. OD: Scleral lens with 3D toric periphery. Image captured 30 seconds after fluorescein instillation. |
Discussion
When troubleshooting midday fog, it is important to first aggressively treat any lid disease or giant papillary conjunctivitis. Preservatives in solutions can also cause a buildup of matter in the lens, so preservative-free, peroxide-based solutions should be used. Introducing a regular deep cleaner like Progent can also be effective.
Central vaults should also not exceed 150 to 200 microns to minimize fogging. If a patient has a toric sclera, toric haptics can be used to create a greater seal.
Another consideration is the diameter of the lens. The farther sclera gets from the limbus, the more toric it becomes.6 Some believe the debris is related to the scleral lens placing pressure on the goblet cells of the conjunctiva, causing more mucin to be released into the eye.1,4-5,7 Smaller diameter lenses (16mm or less) will reduce the amount of misalignment of the conjunctiva, creating a better seal to prevent debris from entering the lens.
Lens flexure should be minimized to reduce movement of the lens against the conjunctiva by increasing the center thickness of the lens.8-10 In cases where fogging persists and the fit and care are optimized, patients can use a solution with higher viscosity to fill the lens and keep debris out of the lens chamber.
1. Caroline P, Andre M. Cloudy vision with sclerals. Contact Lens Spectr. 27(2012),:56.
2. Miller W. Scleral contact lens fog. Contact Lens Spectr. 28(2013):52.
3. McKinney A, Miller W, Leach N, et al. The cause of midday visual fogging in scleral gas permeable lens wearers. Invest Ophthalmol Vis Sci. 2013;ARVO E–Abstract:5483.
4. Walker MK. Scleral lenses, clearing the fog. ISITE Online J. October 2014. Available at www.netherlens.com/october_2014.
5. Walker MK, Bergmanson J, Miller W, et al. Complications and fitting challenges associated with scleral contact lenses: a review. Cont Lens Anterior Eye. 2016 Apr;39(2):88-96.
6. Ritzmann M, Caroline P, Walker M, et al. Understanding scleral shape with the Eaglet Eye Surface Profiler. Scientific Poster presented at 2015 Global Specialty Lens Symposium, January 2015; Las Vegas, NV.
7. Hemmati R, Walker MK, Bergmanson J. Scleral lens tear film reservoir analysis: protein and lipid concentrations in midday fogging. Paper presented at 2016 Global Specialty Lens Symposium, January 21-24, 2016; Las Vegas, NV.
8. Ritzmann M, Caroline P, Walker M, et al. Understanding scleral shape with the Eaglet Eye Surface Profiler. Scientific Poster presented at 2015 Global Specialty Lens Symposium, January 2015; Las Vegas, NV.
9. Harris MG. Contact lens flexure and residual astigmatism on toric corneas. J Am Optom Assoc. 1970;41(3):247-248.
10. Harris MG, Chu CS. The effect of contact lens thickness and corneal toricity on residual astigmatism and flexure. Am J Optom Arch Am Acad Optom. 1972;49(4):304-307.
11. Corzine JC, Klein SA. Factors determining rigid contact lens flexure. Opt Vis Sci. 1997;74(8):639-645.
12. Sindt CW. The great silicone cover up. Review of Cornea and Contact lenses. 2015 Apr;152(3):7.


