The Soft Lens, 50 Years OnCheck out articles commemorating the soft lens's anniversary:Material Gains: 50 Years of the Soft Contact Lens Manufacturing a Brand-New Industry Replaceable Lenses, Irreplaceable Progress |
By the 1960s, corneal lenses made using PMMA could be manufactured to correct myopia, hyperopia, astigmatism and even novel bifocal designs for presbyopia correction, but wearing times were often limited by the loss of vision caused by light scatter in the corneal epithelium, reported as “Sattler’s veil.” Ironically, the good optics of these lenses were compromised by the poor physiological response of the cornea to typical periods of wear.
It was the physiological response of the cornea to contact lens wear that became the primary focus of contact lens research during this time.
In 1960, Wichterle and Lim, two Czechoslovakian chemists, researched hydrogels and began to formulate the world’s first “soft” contact lenses from their newly invented HEMA hydrogel material.1,2 This 38% water content material was highly flexible, more oxygen permeable and significantly more comfortable than the rigid PMMA corneal contact lenses that were available. Wichterle’s new hydrogel materials and a novel molding process called “spin casting” were ultimately licensed to Bausch + Lomb, and in 1971 the company obtained approval from the Food and Drug Administration to sell hydrogel lenses in the United States.3
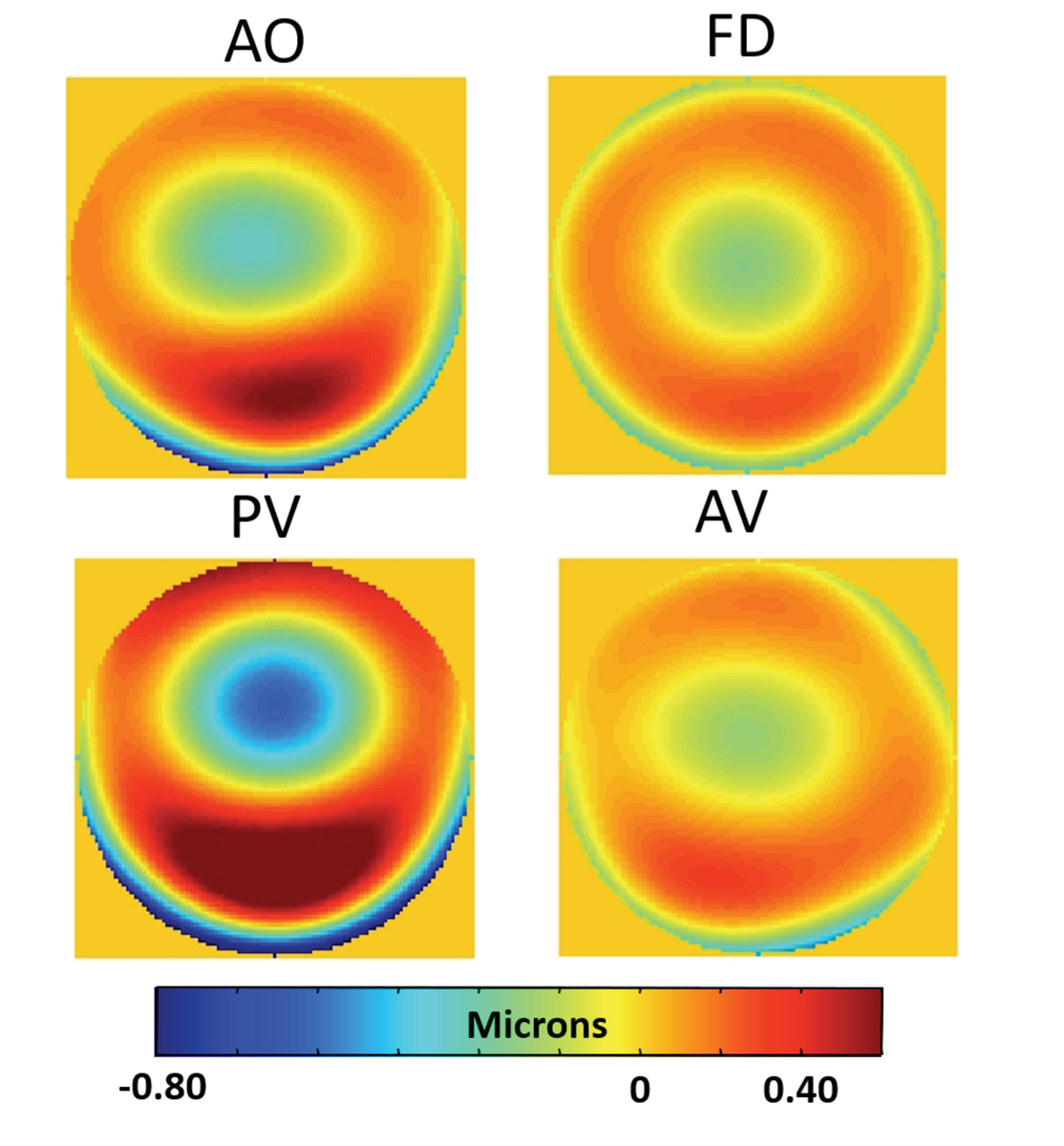 |
Higher-order wavefront error maps (6mm pupil) of four different soft toric contact lenses (all -3.00D nominally labeled power) as measured with an aberometer off of the eye in a saline-filled wet cell. Lower-order aberrations, including sphere and astigmatism, have been zeroed to show only the higher-order aberrations. AO: AirOptix for Astigmatism (Alcon); FD: Focus Dailies Toric, now discontinued (Alcon); PV: PureVision for astigmatism (Bausch + Lomb); AV: Acuvue Oasys for Astigmatism (Johnson & Johnson Vision Care). Click image to enlarge. |
The first lens made commercially available was the Bausch + Lomb C-series contact lens. This fit the eye with considerable decentration and movement due to its 12.5mm diameter modeled from the traditional hard lens fitting philosophy. Although the optics were compromised by the wildly aspheric posterior lens surface produced by the spin-casting manufacturing process, the lens was extremely comfortable compared with the PMMA corneal lenses it competed against in the marketplace.4
The rapid commercial acceptance of soft contact lenses quickly led to development of additional designs by Bausch + Lomb and others. It was over this time that soft lenses become manufactured with larger diameters and greater sagittal depths to provide a more centered, less mobile lens fitting. In addition, spherical optical surfaces were now generated to minimize unwanted optical aberrations of those first, uncontrolled, aspheric designs. Comfort was no longer an issue for all waking hours of wear, and compared with PMMA lenses, the physiological response of the cornea was greatly improved.
Exclusive ExcerptThis article is excerpted from “How Contact Lenses Have Influenced Research Developments in Optics and Vision Science” by the same authors, to be published in Hindsight: Journal of Optometry History later this year. Readers interested in obtaining copies of Hindsight should contact David Goss, OD, at [email protected]. |
Soft lenses were initially only available in spherical powers to correct myopia and later hyperopia, but by the mid to late 1970s soft lenses to correct astigmatism became available.5 Unlike rigid lenses that mask the astigmatic component of the cornea, soft lenses largely conform to the underlying corneal shape, and so the toric shape of the cornea is transferred to the front surface of the soft lens. The addition of an astigmatic correction to the soft lens required a method of stabilization and orientation to be built into the physical shape of the lens.
The most successful designs used an increasing thickness profile in the vertical meridian of the lens, allowing the squeeze force of the upper eyelid to stabilize the lens on the eye between blinks. While successful, lenses manufactured for this approach were difficult to make repeatedly, and so toric soft lenses were not widely accepted until the mid 1980s. At this time, Bausch + Lomb developed a lathe that could generate a toric surface without distorting the button, eliminating the inherent stress that plagued the optical quality of earlier designs and contributed to the consistency that clinicians expect with modern toric lenses.
The toric-generating lathes were the forerunners of today’s computer numeric control (CNC) lathing technology that is the backbone of the contact lens industry. Ultimately, many soft lenses were cast molded between two rigid plastic mold surfaces in the 1980s. This process was also adopted for toric soft lenses within a decade, to provide lenses with little lens to lens variance and high optical quality surfaces. However, the tooling creating the molds for these lenses is still generated using the same CNC lathes often used for directly lathing precise, and sometimes quite complex, lens surfaces.
Multifocal Lenses for Presbyopia
Correction of presbyopia was a new optical frontier for soft contact lenses during the 1980s and ’90s.
Such products were introduced by Bausch + Lomb and Ciba Vision in 1982.6 In B+L’s case, experience with significant spherical aberration in their first lenses for myopia helped them manufacture a lens with spherical aberration aimed to expand the depth of field of the wearer.
Ironically, after spending years trying to eliminate spherical aberration inherent in their spin-cast lens products, they purposely reintroduced positive spherical aberration into the design of their PA1 single (center distance) add bifocal to extend the depth of focus of the wearer. The Ciba “BiSoft” bifocal lens was a center-distance annular bifocal design with multiple add powers available. Both lenses were designed to provide improved distance and near vision for presbyopic patients using a “simultaneous imaging” concept.
In this approach, light from both distant and near objects passes through the pupil simultaneously. Those light rays most conjugate to the retina and the field object will provide the most in-focus image on the retina, while those that are out of focus for that object-plane will reduce the contrast, and potentially even the resolution of the retinal image. In these simultaneous image lenses, theoretically no movement or decentration of the lens is required to provide the visual transition from distance to near focus. Patients demonstrated acceptable distance and near visual acuity in the exam room, but reports of glare, haloes and poor vision in dim light, particularly while driving, led to low levels of acceptance with these and later multifocal contact lenses of the era.
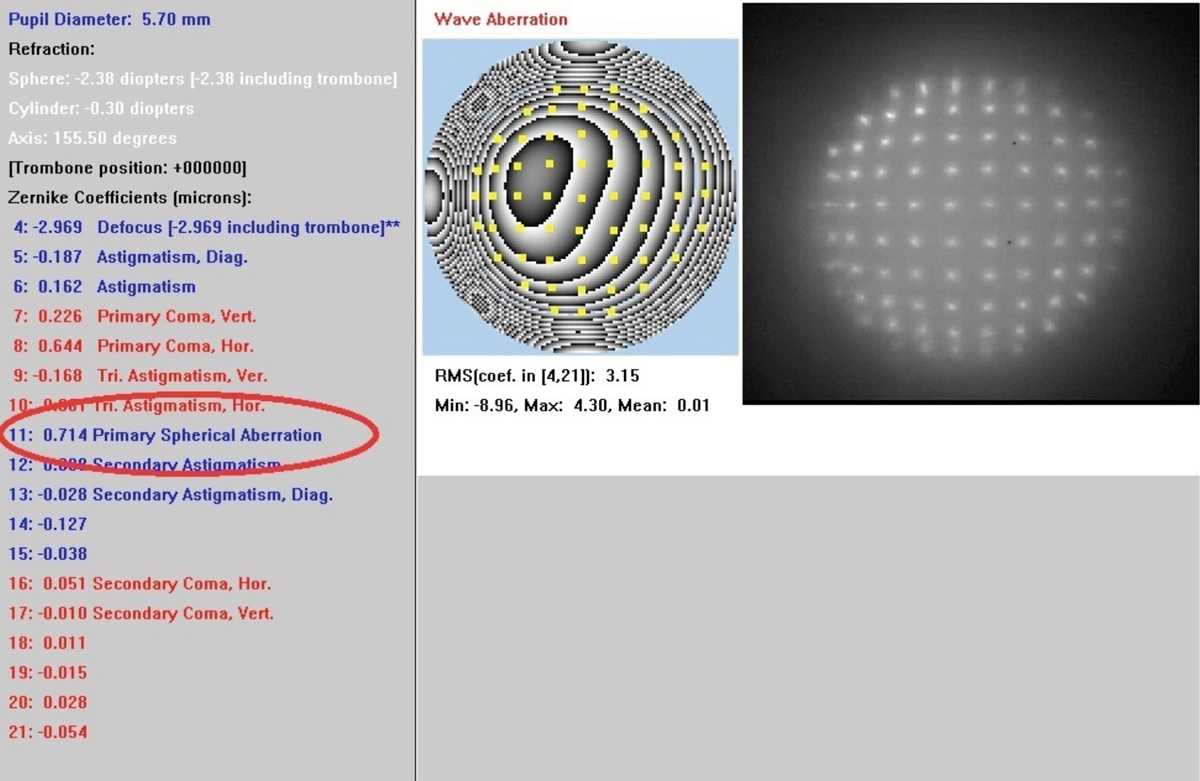 |
Early prototype Shack-Hartmann wavefront image and Zernike output for a positive spherical aberration multifocal aspheric soft contact lens on eye. Note that the different spot size spacing indicates leads to the high Zernike spherical aberration value. Click image to enlarge. |
An alternative form of correction for presbyopes—monovision, where single vision lenses are used to correct one eye for distance and the other for near—was rarely prescribed amid concerns from practitioners that the compromise in binocularity was too severe and that the patients were effectively monocular at both distance and near focus.
In the late 1980s and early 1990s, the introduction of an alternative simultaneous image design, the diffractive lens, reignited interest in bifocal contact lenses. Specifically, the unique diffractive designs of the rigid Pilkington Diffrax and soft Hydron Echelon lenses, respectively, eliminated the impact of pupil size on the proportion of light dedicated to the distance and near retinal images that plagued more traditional refractive optics solutions.7,8 While clinical use demonstrated that the performance of the lenses was not pupil dependent, diffractive optics suffered from other problems. Most significant, and perhaps the main reason that they were not more successful, is that an inherent limitation of diffractive optics occurs when light is divided between the distance and near foci.
At this point, a significant proportion of light (up to 20%) is lost to other, higher orders of diffraction.9 From a practical standpoint, this light might be considered “scattered” across the retinal image, causing a reduction in contrast.10 Wearers perceived this scattering as a “graying” or a “washing out” of the visual scene and sometimes complained of reduced vision in conditions of low illumination or contrast. When combined with their relatively expensive cost at the time, these difficulties limited uptake of the concept in the marketplace. Interestingly, diffractive intraocular lenses are now quite common despite the design’s lack of success within contact lenses.
HOAs & the Prime of Better Vision
The development of clinically applicable Hartmann-Schack wavefront sensors in the late 1990s provided the breakthrough needed to understand the link between the theoretical design and visual performance of single vision and multifocal soft contact lenses and the clinical reality of the retinal image quality that these lenses were providing.
Early population measurements of the wavefront error of the eye of large contact lens wearing age populations, identified the presence of significant levels of higher order wavefront aberrations over and above the defocus and astigmatism that traditional refraction methods had identified.11 For many patients who exhibited large amounts of these higher-order aberrations (HOAs), retinal image quality was significantly compromised even with a best sphero-cylindrical correction in place, and especially under low illumination, large pupil conditions.
This aberrometry technique was quickly adopted to measure the true optical performance of rigid and soft, single vision and multifocal contact lenses in vivo, but also proved to be an ideal method to evaluate the optical performance of contact lenses off the eye.12-15 Wavefront sensor technology combined with the next generation CNC lathing technology allowed the potential for new and varied optical designs for contact lenses to be imagined and developed.
Clinical and laboratory wavefront sensors became available commercially in the early 2000s and ignited significant research interest in the potential of altering the optics of contact lenses to improve vision in patients. This work has largely focused on either obtaining some improvement for the average eye within the population or more significant improvement in individual eyes with more significant higher order aberrations (e.g., older eyes and those with corneal shape-related pathologies such as keratoconus).
Of course, the combination of the eye plus contact lens optics are what provide the resulting vision for the wearer. Clinically, this result is typically verified by an in-office contact lens over-refraction, but there are several variables that may complicate this seemingly simple combination. As is well known, the eye contains inherent lower-order (e.g., sphere and astigmatism) as well as HOA.
Several population studies have determined that many eyes have varying amounts of positive or negative higher-order aberration. However, due to some eyes having positive and other eyes negative amounts of these aberrations, when averaged across the population the resultant magnitude is largely zero.16 This is not true for spherical aberration, however, where the average ocular spherical aberration for the typical young adult population is positive and approximately 0.18µm in magnitude (over a 6mm pupil).17
Additionally, the lens itself could be made with aberration by chance or by design. Specifically, spherical contact lenses, by design, contain spherical aberration due to their highly curved anterior and posterior surfaces; minus lenses containing negative spherical aberration and plus lenses positive spherical aberration.18-20
In theory, either the spherical aberration of the lens, the eye or both could be corrected by creating a precise, radially symmetric asphericity in the contact lens. Interestingly, because of its inherent spherical aberration, a spherically surfaced soft contact lens of around -7.00D has a magnitude of spherical aberration sufficient to counteract the average spherical aberration of the population.
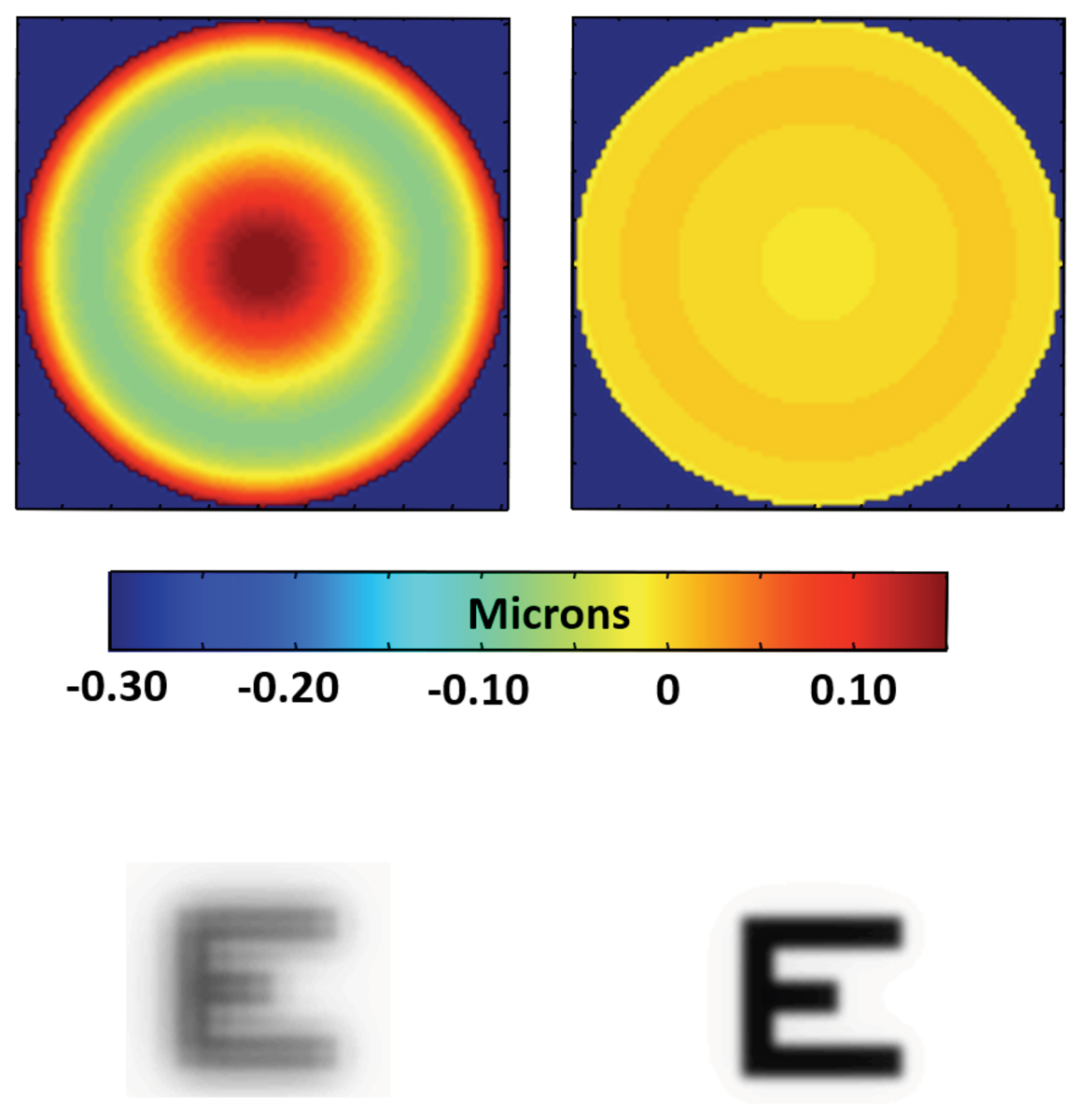 |
Higher-order wavefront error (top row) and the resulting image simulations (bottom row) of the sum of the contact lens spherical aberration and that of the average eye while wearing a spherical lens that is of -1.00D (left) and and -7.00D power (right) with a 6mm pupil. Click image to enlarge. |
Since substantial amounts of negative spherical aberration occur for powers as low as −4.00D, many myopic contact lens-wearing patients may have some spherical aberration corrected even by a typical single vision soft contact lenses.21 Those outside this range may experience little change, or a worsening, of their eye plus lens aberration.
For instance, patients with positive defocus corrections (i.e., hyperopes) will experience even greater levels of positive spherical aberration, due to the combined effect of their inherent, ocular, spherical aberration and that induced by their spherical contact lens. Alternatively, it is possible to minimize the visual effects of spherical aberration by providing an appropriate, aspheric correcting surface on the contact lens, tailored for all defocus corrections. Indeed, several manufacturers (Bausch + Lomb, CooperVision) did just this, starting in the late 2000s, by commercializing products, both spherical and toric, that used aspheric surfaces to minimize total eye plus lens spherical aberration for the average eye. The intention was to improve the quality of vision under low illumination conditions.
However, if this correcting lens (or any lens) is not centered on the eye, other visually degrading aberrations are introduced. Specifically, in the case of a lens with spherical aberration, coma is introduced in amounts directly proportional to the magnitude of the decentration.22 As decentrations can be as much as 1mm horizontally and vertically in some lenses, this could have a substantial negative visual impact.23,24 Also, it is well-known that rigid lenses (e.g., corneal GP) do not conform to the cornea, so introduce a tear film with optical power and aberration. However, although assumed to conform completely to the cornea, it has been shown that soft lenses do not always do so, but rather exhibit some partial flexure. This flexure, therefore, induces aberration when on the eye.
For example, high power lenses may not induce the desired levels of sphere correction, and also induce unintended levels of spherical aberration.25-27 Specifically, they may introduce spherical power errors as high as 0.50D to 1.00D, and spherical aberration errors up to around 0.20µm (for a 6mm pupil). These levels of error are more than sufficient to degrade vision. Also, importantly, these levels of aberration are dependent on the lens power, thickness and material/modulus.22
All the issues described above need to be addressed if the optical performance of the contact lens-wearing eye is to reach its maximum potential. Some manufacturers have attempted to minimize these issues. For example, aspheric lenses that have no spherical aberration as a function of lens power have been created to make them resistant to on-eye positioning errors and not introduce further aberration.
Another approach combines the issue just described to create a lens that also accounts for on-eye flexure changes.28 Additionally, as mentioned above, while spherical aberration is clearly the largest higher-order ocular aberration in the general population, it is quite often not the dominant aberration in individual eyes. Third-order Zernike aberrations, such as coma and trefoil, are frequently problematic, even though their population average is close to zero.
Unlike the approaches described above, these aberrations must be corrected by a rotationally stable contact lens, manufactured using a process capable of creating non-rotationally symmetrical surfaces. Clearly then, a contact lens must be designed to correct both symmetrical and non-rotationally symmetrical HOAs of the eye plus contact lens system, if visual benefit is to be maximized across a substantial proportion of the population.
Several research groups have attempted making customized higher-order wavefront aberration correcting soft contact lenses to minimize the effects of some of the problems described above.29,30 Due to the amounts of on-eye movement, even in soft contact lenses, limiting some of the achieved benefit, other groups continue working on similar concepts for scleral lenses with smaller on-eye movements.31,32 Results have been promising to date, with significant reductions in eye plus lens HOAs from these custom aberration-correcting contact lenses. Interestingly, however, the improvement in visual performance recorded by subjects wearing these lenses, while measurable, does not correlate well to the magnitude of HOA reduction observed.31 It has been demonstrated that some patients with chronic HOAs, caused by corneal pathology, may adapt to their reduced retinal image quality and therefore, will require a period to “re-adapt” to the improvement provided by a custom correction.33
Clinical and laboratory wavefront sensors have also improved the design and manufacturing quality of multifocal contact lenses during the 2010s with most current designs incorporating multiple zones of continuous curvature to provide an increased depth of focus, from distance through intermediate and near.
These improved multifocal designs aim to better meet the visual needs of the current era in which computers and hand-held electronic devices dominate the work environment, while simultaneously reducing the impact of glare and halos caused by sharp optical junctions between the power zones of previous lenses. In addition, many earlier presbyopic contact lenses were designed by adding the multifocal optical component to the single spherical surface of a single vision lens, without taking into consideration the inherent spherical aberration of the base lens design. This led to lenses having different optical power profiles depending upon their back-vertex power.31
Current generation multifocal lenses can be designed and tested with wavefront sensing metrology to ensure that all back-vertex powers have the same multifocal power profile across the optical zone. The resulting hope is that this leads to a consistent fitting experience for contact lens practitioners as they work with patients across a wide range of refractive corrections. Clinically, multifocal lenses now have an increased acceptance over monovision for presbyopic patients seeking a contact lens correction. This confirms the improved optical performance of these lenses that enhanced metrology and manufacturing has made possible.
Conclusion
Industry and clinicians alike have made great strides in understanding the optical challenges of a soft material over the past 50 years.
Today’s lenses address nearly all refractive challenges with at least some success, and often complete avoidance of the need for spectacle lens wear. The work continues apace and future generations of lenses will no doubt exceed today’s standards.
Dr. Cox, a researcher with over 30 years’ experience in ophthalmic medical devices, is an adjunct professor at the Center for Visual Science, University of Rochester, NY.
Dr. Kollbaum is associate dean for research, director of the Borish Center for Ophthalmic Research and an associate professor at the Indiana University School of Optometry.
Dr. Papas is a professor in the School of Optometry and Vision Science at the University of New South Wales in Sydney, Australia.
1. Wichterle O, Lim, D. Hydrophilic gels for biological use. Nature 1960;185:117-8. 2. Wichterle O, Lim D. Process for producing shaped articles from three-dimensional hydrophilic high polymers. US Patent 2,976,576. March 28, 1961. 3. Lamb J, Bolton T. History of Contact Lenses. In Phillips T and Speedwell L, eds. Contact Lenses, 6th Ed. Elsevier; 2019:12. 4. Newman S, Clamp J. Contact Lens Manufacturing, In Phillips T and Speedwell L, eds. Contact Lenses, 6th Ed. Elsevier; 2019:511. 5. Lamb J, Bolton T. History of Contact Lenses. In Phillips T and Speedwell L, eds. Contact Lenses, 6th Ed. Elsevier; 2019:12. 6. Ellis D, Grimsrud R. Soft bifocal contact lenses for presbyopia (Thesis). College of Optometry. 1983. 637. commons.pacificu.edu/opt/637. Accessed March 31, 2021. 7. Freeman MH. Ophthalmic lens with diffractive power. US Patent 4,641,934. February 10, 1987. 8. Bradley A, Rahman HA, Soni PS, Zhang X. Effect of target distance and pupil size on letter contrast sensitivity with simultaneous vision bifocal contact lenses. Optom Vis Sci. 1993;70(6):476-81. 9. Young G, Grey CP, Papas EB. Simultaneous vision bifocal contact lenses: a comparative assessment of the in vitro optical performance. Optom Vis Sci. 1990;67(5):339-45. 10. Back A, Grant T, Hine N. Comparative visual performance of three contact lens corrections. Optom Vis Sci. 1992;69 (6):474-80. 11. Porter J, Guirao A, Cox IG, Williams DR. Monochromatic aberrations of the human eye in a large population. J Opt Soc Am. A 2001;18:1793-1803 12. Bakaraju RC, Ehrmann K, Ho A. Extended depth of focus contact lenses vs. two commercial multifocals: Part 1. Optical performance evaluation via computed through-focus retinal image quality metrics. J of Optom 2018;11:10–20. 13. Lu F, Mao X, Qu J, et al. Monochromatic wavefront aberrations in the human eye with contact lenses. Optom Vis Sci 2003;80(2):135-41. 14. Kollbaum PS, Bradley A, Thibos LN. Comparing the optical properties of soft contact lenses on and off the eye. Optom Vis Sci. 2013;90(9):924-36. 15. Kim E, Bakaraju RC, Ehrmann K. Reliability of power profiles measured on NIMO TR1504 (Lambda-X) and effects of lens decentration for single vision, bifocal and multifocal contact lenses. J of Optom. 2016;9(2):126-36. 16. Thibos LN, Hong Xin, Bradley A, Cheng Xu. Statistical variation of aberration structure and image quality in a normal population of healthy eyes. J Opt Soc Am A Opt Image Sci Vis. 2002;19:2329-48. 17. Kingston AC, Cox IG. Population spherical aberration: associations with ametropia, age, corneal curvature and image quality. Clin Ophthalmol. 2013;7:933-8. 18. Westheimer G. Aberrations of contact lenses. Optom Vis Sci 1961;38:445–8. 19. Bauer GT. Longitudinal spherical aberration of modern ophthalmic lenses and its effect on visual acuity. Appl Opt. 1980;19(13(:2226-34. 20. Cox IG. Theoretical calculation of the longitudinal spherical aberration of rigid and soft contact lenses. Optom Vis Sci. 1990;67(4):277–82. 21. Dietze HH, Cox MJ. On- and off-eye spherical aberration of soft contact lenses and consequent changes of effective lens power. Optom Vis Sci. 2003;80:126–34. 22. Guirao A, Williams DR, Cox IG. Effect of rotation and translation on the expected benefit of an ideal method to correct the eye’s higher-order aberrations. J Opt Soc Am A Opt Image Sci Vis. 2001;18(15):1003-15. 23. Tomlinson A, Ridder WH, Watanabe R. Blink-induced variations in visual performance with toric soft contact lenses. Optom Vis Sci. 1994;71(9):545–9. 24. Chen M, Sabesan R, Ahmad K, Yoon G, Correcting anterior corneal aberration and variability of lens movements in keratoconic eyes with back-surface customized soft contact lenses. Opt Lett. 2007;32:3203-5. 25. Plainis S, Charman WN. On-eye power characteristics of soft contact lenses. Optom Vis Sci. 1998;75(1):44-54. 26. Holden BA, Siddle JA, Robson G, Zantos SG. Soft lens performance models: the clinical significance of the lens flexure effect. Aust J Optom 1976;59:117-29. 27. Kollbaum, PS, Bradley A, Thibos LN. Comparing the optical properties of soft contact lenses on and off the eye. Optom Vis Sci 2013;90(9):924-936. 28. Payor RE, Kollbaum P, Ye Ming, Bradley A. Optimizing optical aberrations in ophthalmic lenses. US Patent Application 2011/0102737 A1. May 5, 2011. 29. Marsack JD, Parker KE, Applegate RA. Performance of wavefront-guided soft lenses in three keratoconus subjects Optom Vis Sci. 2008;85(12):1172–8. 30. Sabesan R, Jeong TM, Carvalho L, et al. Vision improvement by correcting higher-order aberrations with customized soft contact lenses in keratoconic eyes. Opt Lett. 2007;32(8):1000-2. 31. Marsack JD, Ravikumar A, Nguyen C, et al. Wavefront-guided scleral lens correction in keratoconus. Optom Vis Sci. 2014;91(10):1221-30. 32. Sabesan R, Johns L, Tomashevskaya O, et al. Wavefront-guided scleral lens prosthetic device for keratoconus. Optom Vis Sci. 2013;90(4):314-23. 33. Sabesan R, Yoon G. Perceptual learning after correcting the eye’s aberration with adaptive optics. Invest Ophthalmol Vis Sci. 2013;54:ARVO Abstract 1282. |


