Often, patients believe they are not candidates for contact lenses because of their chronic dry eyes. Lens-induced dry eye can cause associated symptoms to appear or even worsen, while pathologic causes of dry eye include more common etiologies such as evaporative meibomian gland dysfunction (MGD).1,2 Aqueous deficiency is another less common cause of dry eye due to lacrimal gland dysfunction associated with systemic diseases, such as Sjögren’s syndrome or chronic graft-vs.-host disease (GVHD).
In addition to ocular surface and tear quality concerns, other factors contribute to the complexity of fitting contact lenses, such as patient’s refractive error, corneal or conjunctival irregularities and poor blink function. Perhaps they have tried contact lenses in the past and were not successful due to comfort, vision or handling. However, much has changed with contact lens materials and design over the last 10 years in regards to access, comfort and variety.
Dry eye patients who are not great candidates for refractive surgery should consider the appropriate contact lens as an alternative.3 Improving the ocular surface and tear film prior to contact lens fitting is the key to success.
 |
| Fig. 1. A depression in this patient’s conjunctiva, due the removal of a tube shunt, allowed debris to be sucked under the loose scleral lens edge, clouding vision. Click image to enlarge. |
Treatment and Prep
Start dry eye treatment as early as you can in the fitting process, and take the time to assess the severity of the patient’s condition. If you provide them the optimal dry eye treatment while stressing the importance of compliance, you will be giving them the tools they need to achieve the highest level of contact lens wear success and adherence.
Determining the root cause of dry eye will help make the contact fitting process successful. Review the patient’s symptoms with the Ocular Surface Disease Index (OSDI) questionnaire and medical history and note any inflammatory conditions, such as rheumatoid arthritis, thyroid disease and allergies, as well as the medications they use that may contribute to dry eye, such as anti-anxiety/antidepressant medications, anti-hypertensives and oral antihistamines. Consider all the different behavioral and environmental factors that could exacerbate their dry eyes. Ask them how much of their day is spent looking at their computer. Then, thoroughly assess their ocular surface and tear film with numerous tests, including Oculus Keratograph 5M imaging. After thoroughly assessing and determining the patient’s dry eye severity, prescribe treatments to manage the condition and prepare the eye for contact lens success.
Lastly, determine the patient’s visual demands. We want to provide them the best possible vision, ease of handling, comfort and relief of dry eye symptoms.
 |
| Fig. 2. The patient in Figure 1 was refit with a scleral lens with a lower edge to better align with the conjunctival depression. The patient reported better vision throughout the day. Click image to enlarge. |
Soft Lens Benefits
This lens type may be the preferred choice for patients with mild dry eye or patients who are consistent with their dry eye treatment. These lenses are made of flexible materials that drape over elevations or depressions in the conjunctiva, often making them easier to fit. One key measurement for fitting contact lenses is corneal diameter. For example, with smaller corneas, select smaller diameter soft lenses and flatter base curves to improve edge alignment and tear flow under the lens for improved comfort.4 Soft lens handling may be easier for patients with previous soft lens experience. Unfortunately, some may still need instruction on better techniques.
Daily disposable lenses provide fresh, clean and convenient lenses. In my practice, I have found this option better for people with allergies. Also, storage solutions used with reusable lenses may result in toxicity.5-7
Soft lenses are available in new breathable silicone hydrogel materials with high-water gel-like surface treatments (Precision1 and Dailies Total1, Alcon) for enhanced comfort and increased wearing time. Fortunately, new daily disposable lenses are available to correct higher prescriptions, astigmatism as well as presbyopia with multifocal designs.
Consider trying soft lenses first if you note irregular conjunctival anatomy on the slit lamp exam. Also consider lenses such as Acuvue Transitions (Johnson & Johnson) for patients who are light sensitive due to retinal or macular dystrophy or albinism.
 |
| Fig. 3. This presbyopic dry eye patient placed their scleral multifocal lens with a decentered add on the eye upside down (left). After rotating the lens 180 degrees, the reading add was positioned correctly (right). Click image to enlarge. |
Scleral Benefits
Scleral lenses made of rigid, gas permeable (GP) materials provide crisper vision to patients with irregular corneas due to keratoconus or other corneal diseases, or due to corneal trauma or refractive surgery such as radial keratotomy, photorefractive keratectomy, LASIK or cataract surgery.8-11
Still, fitting scleral lenses often requires additional follow up to fine tune the fit and monitor lens settling. Another deterrent to this modality is the higher cost attributed to doctor training, equipment and multiple scleral lens trial sets and replacement costs.
In my practice, patients with moderate to severe dye eye often find scleral lens often more comfortable than soft lenses for the following reasons:
- The thick 0.25mm tear layer across the back surface of the contact lens and over the cornea provides constant lubrication. Only use preservative-free saline in the bowl of the lens before application. Consider preservative-free Nutrifill (Contamac) saline solution or even autologous serum in the bowl of lens for severe dry eye patients.
- Breathable high-oxygen transmissible materials such as Boston XO2 (Bausch + Lomb) and Optimum Infinite (Contamac) provide superior corneal health by allowing more oxygen to reach the cornea.
- New Hydra-PEG (Tangible Science) surface treatments improve wettability and reduce protein deposition.12 Patients notice significant improvement in dryness, lens comfort and vision.
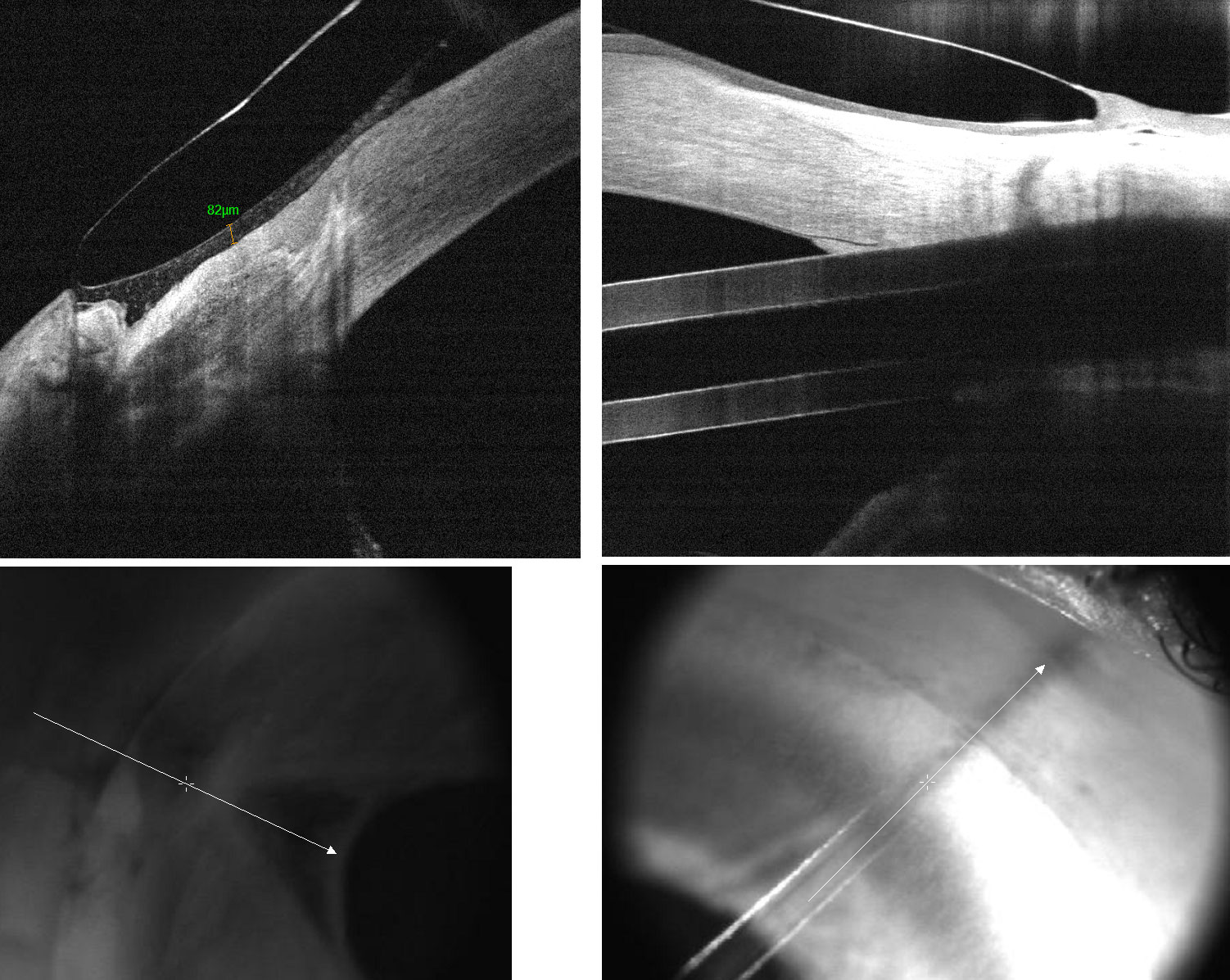
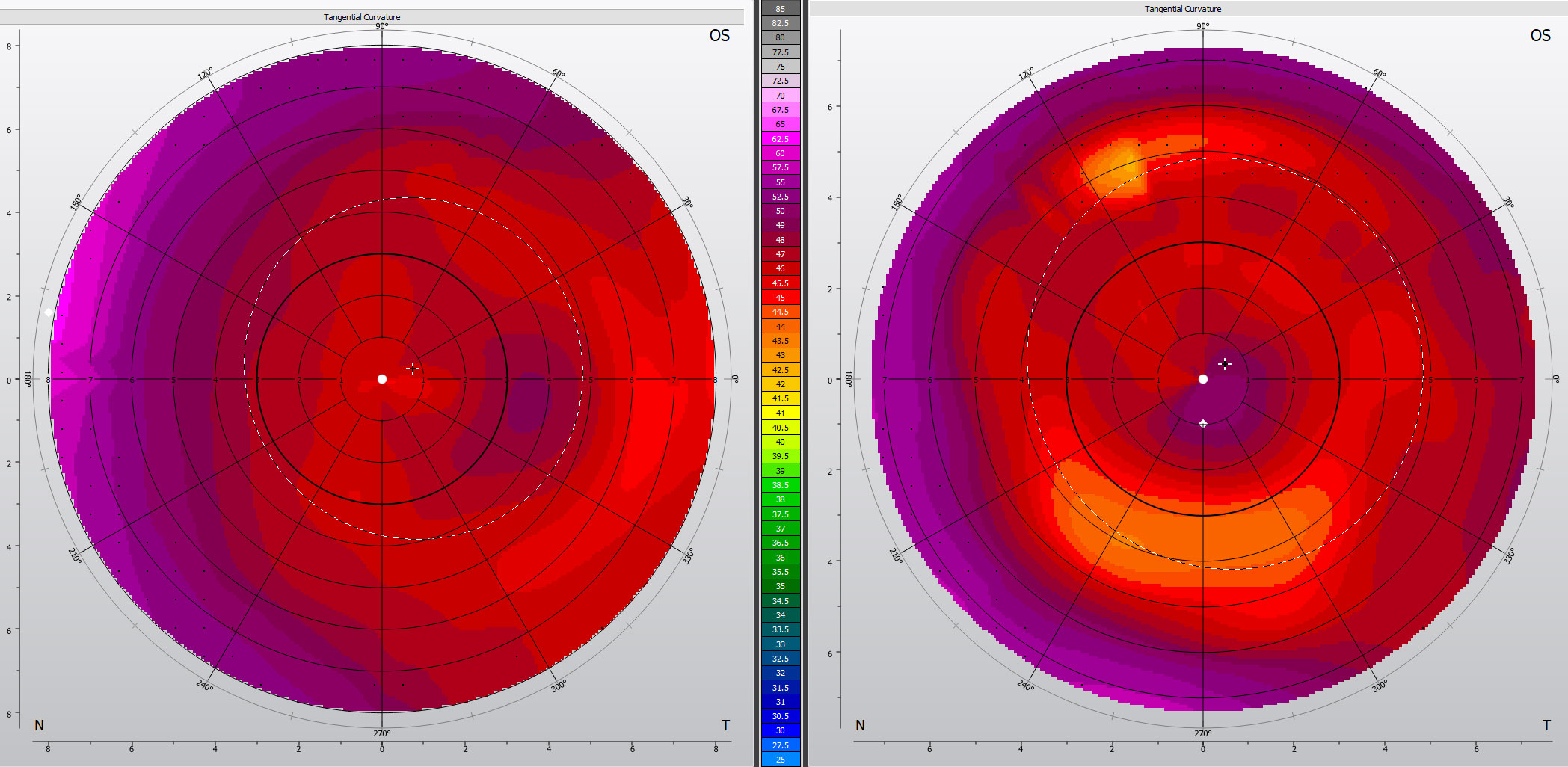
Scleral lenses should be large enough to not touch the cornea. However, selecting a scleral lens diameter that is too large may complicate the fit as the conjunctival anatomy gets more irregular further from the limbus.13-15 Alignment with the conjunctiva can be perfected with use of toric peripheral curves, custom vaults over pingueculas and custom depressions if there is a valley following surgery (Figures 1 and 2).
OCT imaging can guide where edge alignment needs to be enhanced to avoid tear debris getting sucked under a loose edge. Tear layer debris under the lens will blur vision after just a few hours of wear. Corneal topography over the scleral lens can be helpful to assess multifocal add location and to determine the need to decenter the reading add for better distance and near vision (Figure 3).
A well-aligned scleral lens will be more difficult for the patient to remove. However, if they rotate the lens 90 degrees with their finger to misalign the lens with the sclera, the lens is easily removed with a lens remover.
Patients with Sjögren’s or GVHD will do best with well-fitted scleral lenses because of their ability to relieve their disabling dryness by bathing the ocular surface with a tear reservoir between their compromised ocular surface and back surface of the scleral lens.16-18 Scleral lenses provide a smooth ocular surface over irregular or diseased corneas, resulting in best possible vision and greatly improving quality of life.
 |
| Fig. 4. To correct edge lift in the vertical meridian in this trial fit spherical scleral lens, we ordered toric peripheral curves flatter along the horizontal and steeper along the vertical meridians. Click image to enlarge. |
Case 1
A 36-year-old Caucasian male presented to the office requesting a scleral lens fit. He complained of dry eye, discomfort and severe light sensitivity, which made him unable to function at work and play with his three young children. He was diagnosed with GVHD after an allogeneic stem cell transplant to treat his leukemia diagnosed three years ago.
Ocular history was remarkable for LASIK surgery to correct his -3.00D myopia in each eye. He used autologous serum eye drops Q2H to QID OU and Pred Forte (prednisolone acetate ophthalmic suspension 1%, Allergan) 1% eye drops BID OU. He had discontinued Restasis (cyclosporine A 0.05%, Allergan) and Xiidra (lifitegrast 5%, Novartis) due to increased burning with use. To improve his ocular surface and prepare it for scleral lens wear, we prescribed erythromycin antibiotic ointment two to three times a day. His Pred Forte was changed to Lotemax SM (loteprednol etabonate 0.38%, Bausch + Lomb) TID, as it has less risk of intraocular pressure spikes and cataract development.
During the course of the scleral lens fitting we addressed severe meibomian gland obstruction, inflammation, eyelid biofilm formation and tear film instability to help repair the cornea and conjunctiva.
We selected Jupiter scleral lenses with initial trial lens diameter of 16.6mm with spherical peripheral curves. To improve comfort and prevent tear debris due to edge lift in the vertical meridian (Figure 4), we ordered toric peripheral curves that provided better alignment.
The final lens noticeably improved the patient’s comfort and protected his cornea. He noted better visual quality, as the scleral lens provided a smooth surface over his compromised cornea. Scleral lenses helped relieve his severe dry eye, and his drop frequency eventually reduced and light sensitivity improved. He could function better at work and have fun with his children.
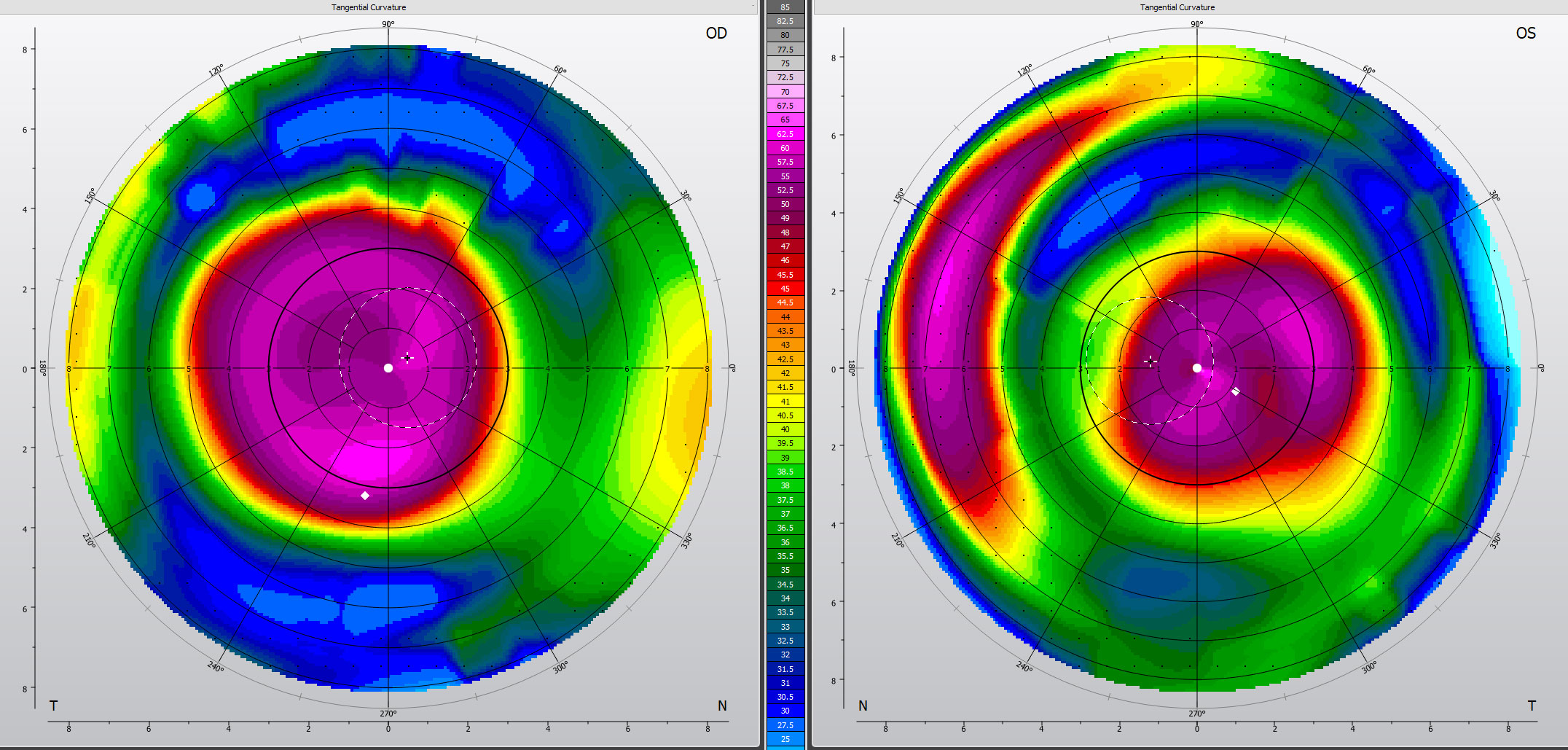 |
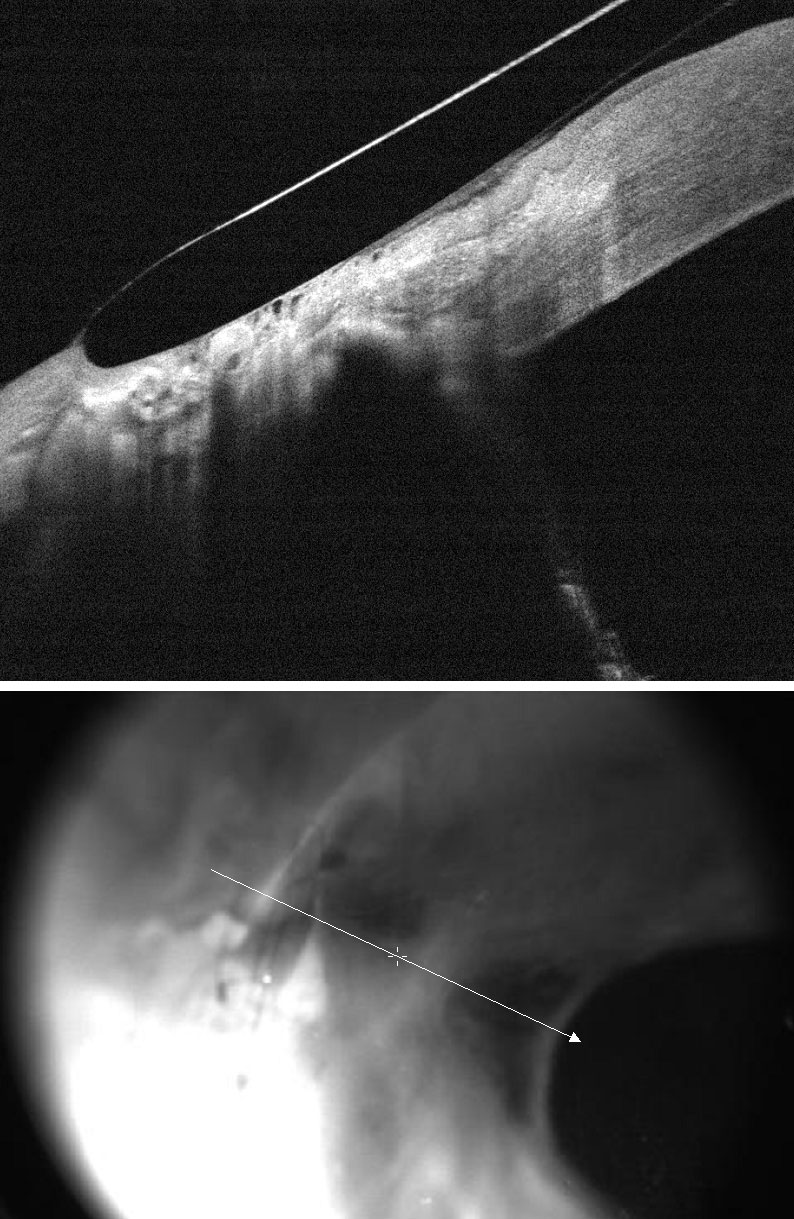
| Fig. 5. Corneal topography of advanced keratoconus OU successfully fit with Kerasoft IC Toric lenses. Click image to enlarge. |
Case 2
An 84-year-old Caucasian female was referred by her optometrist for scleral lens fitting to treat her advanced keratoconus and discomfort with corneal GP lenses. She reported spending only 30 minutes per day on her computer. Her ocular history was positive for cataract extraction with peripheral-curve IOL implantation and nodules were removed from her left cornea. She had contact lens-induced dry eye resulting in her corneal GP lenses becoming less tolerable over the years. Her manifest refraction was +3.75 – 1.00 x 125 20/50 OD and +6.50 – 1.50 x 180 20/30 OS with +1.50 add OU. Autorefractor K’s were 54.00/56.75 @48 OD and 58.50/62.50 @98 OS. Her corneal diameter was 11.90mm, she was OD dominant and pupil size was 3mm OU. Oculus K5M revealed mild MGD and keratoconus, worse in OD (Figure 5).
We initially tried improving the GP fit with custom corneal topography-based lenses, but comfort did not improve significantly. She was successful for the first couple of weeks using scleral lenses, with good 20/30 vision in each eye. But on two occasions in the first month, she had difficulty removing the lens. Unfortunately, she lived about three hours from the office, which worried her enough to strongly request a different solution.
To improve her success with contact lenses, we recommended: warm compresses and lid massage for her moderate MGD, triglyceride form of omega-3s for inflammation, 0.01% hypochlorous acid lid hygiene spray for her eyelid biofilm and artificial tears for tear film instability.
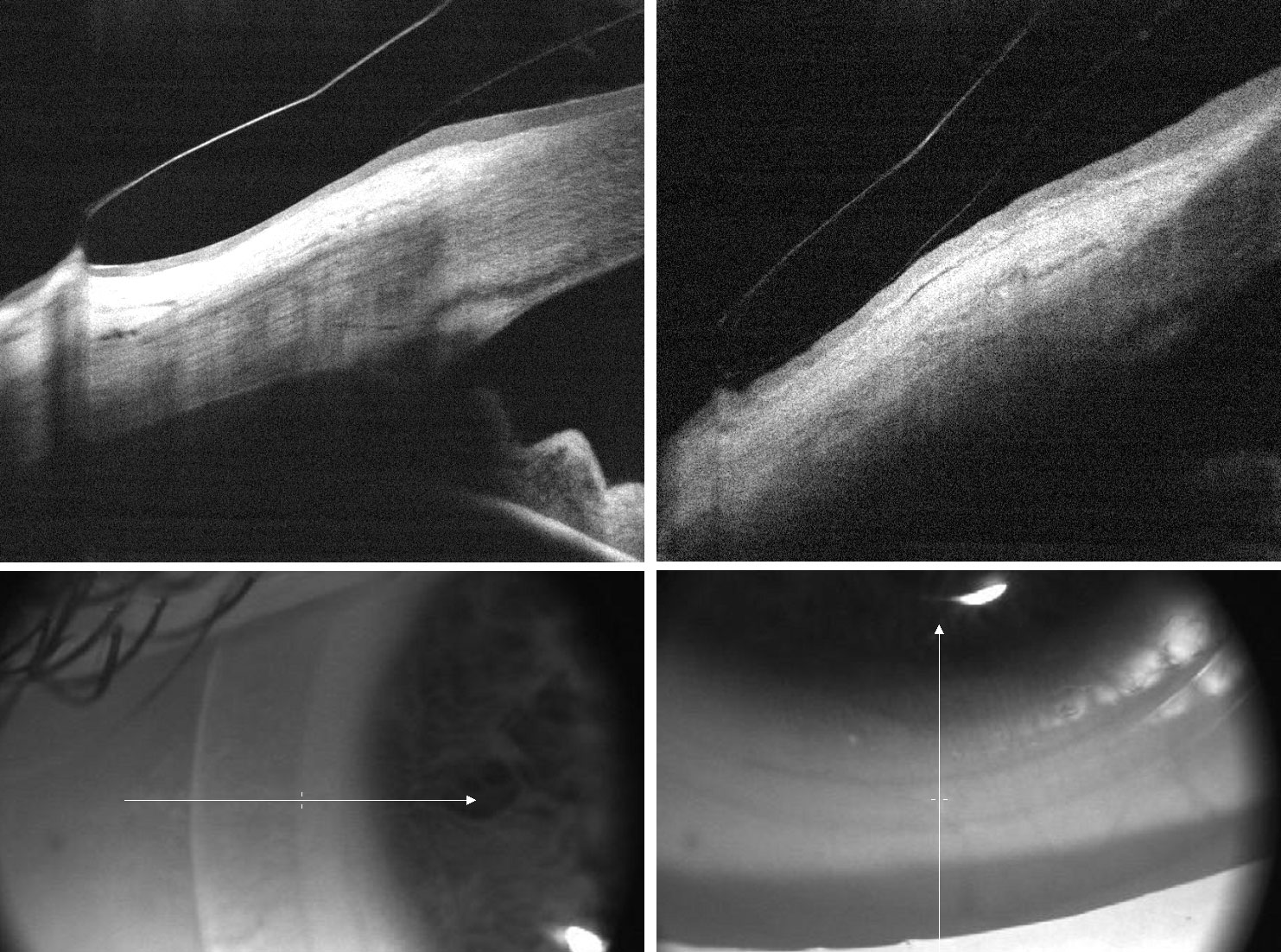
We then offered her Kerasoft IC Toric (Bausch + Lomb) soft lenses that are designed to correct keratoconus and other irregular corneas.19 Single lenses were ordered and then second lens dispensed with final prescription and vision: 8.0 base curve, 14.50 +5.50-1.25 x 138 20/25 OD and 7.80 base curve, 14.50 +7.25 - 1.75 x 176 20/40 OS with standard peripheral curves. She was delighted with her vision, all-day lens comfort and handling (Figure 6). With her small pupils, she only needed +1.50D readers for fine print.
Her toric silicone-hydrogel contact lenses provided conservative dry eye therapy, and she found lens wear to be comfortable all day. The high plus power she needed resulted in a thicker lens that corrected her irregular astigmatism and maintained excellent vision despite her irregular cornea from keratoconus.
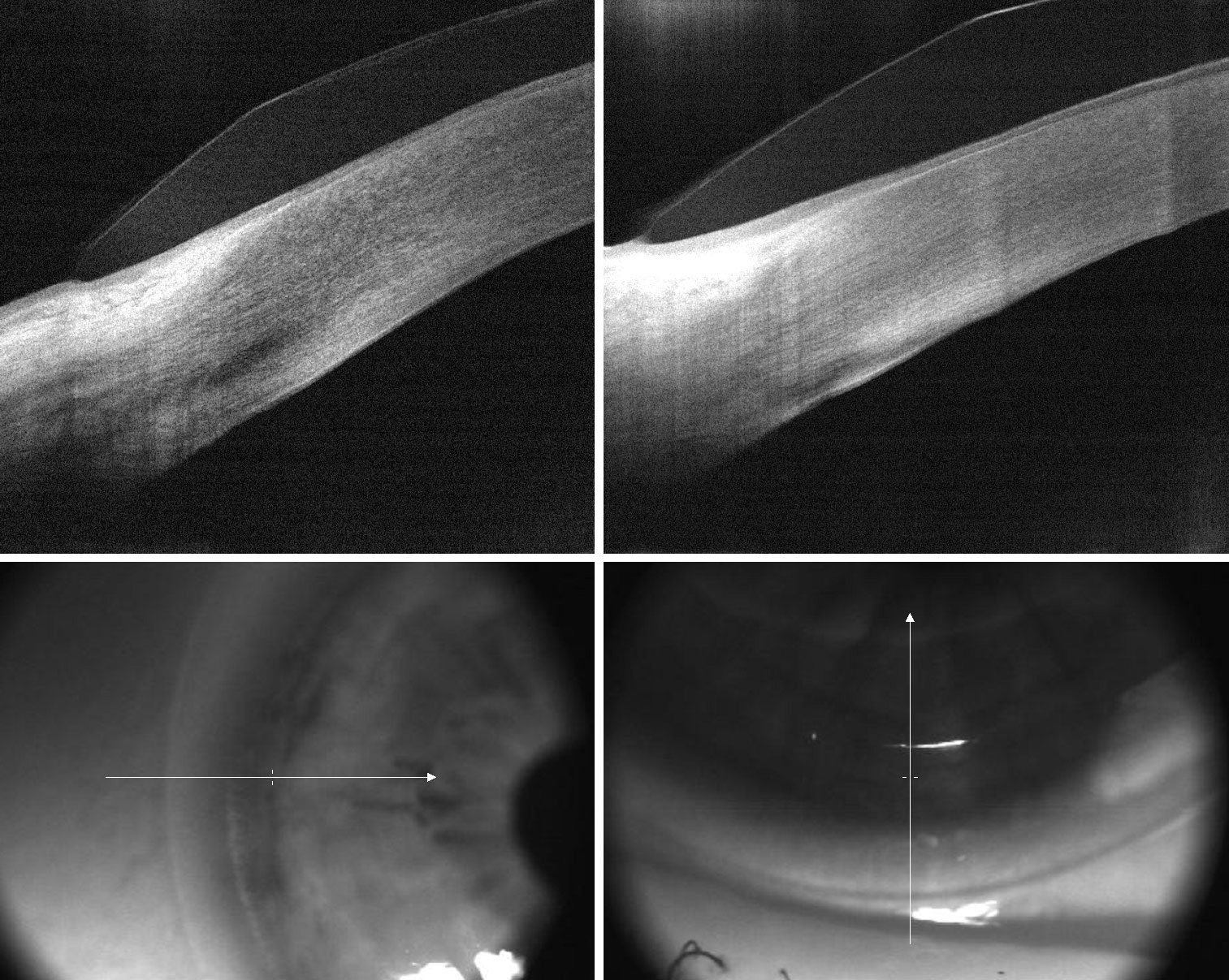 |
| Fig. 6. This toric lens has a thicker edge profile for improved lens stability, while the edge is parallel to the conjunctiva for good comfort. Click image to enlarge. |
Contact lenses can improve quality of life at work, home and play for many dry eye patients. They are happy seeing well with more comfortable eyes while free of glasses during the day. You can improve your patient’s contact lens success by reducing symptoms of dry eyes with timely diagnosis and appropriate treatment. Determining whether soft or scleral lenses will better address the patient’s problems due to dry eye will help provide your patients the vision and comfort they need and improve their quality of life.
Dr. Sweeney practices at Vision Source Insight in Atlanta and is a member of both the Georgia Optometric Association and American Optometric Association (AOA). He is a member of the AOA’s Cornea and Contact Lens and Low Vision sections.
| 1. Molina K, Graham AD, Yeh T. et al. Not all dry eye in contact lens wear is contact lens-induced. Eye Contact Lens. September 10, 2019. [Epub ahead of print]. 2. Lemp MA, Crews LA, Bron AJ, et al. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea. 2012;31(5):472-8. 3. Chuck RS, Jacobs DS, Lee JK, et al. Refractive errors & refractive surgery Preferred Practice Pattern. Ophthalmology. 2018;125(1):P1-P104. 4. Caroline PJ, André MP. The effect of corneal diameter on soft lens fitting, part 1. Cont Lens Spectrum. 2002;17(4):56. 5. Stapleton F, Naduvilath T, Keay L, et al. Risk factors and causative organisms in microbial keratitis in daily disposable contact lens wear. PLoS One. 2017;12(8):e0181343. 6. Wu YT, Teng YJ, Nicholas M, et al. Impact of lens case hygiene guidelines on contact lens case contamination. Optom Vis Sci. 2011;88(10):e1180-1187. 7. Wu Y, Carnt N, Willcox M, Stapleton F. Contact lens and lens storage case cleaning instructions: whose advice should we follow? Eye & Cont Lens. 2010;36(2):68-72. 8. Alipour F, Kheirkhah A, Jabarvand Behrouz M. Use of mini scleral contact lenses in moderate to severe dry eye. Cont Lens Anterior Eye. 2012;35(6):272-6. 9. Walker MK, Bergmanson JP, Miller WL, et al. Complications and fitting challenges associated with scleral contact lenses: a review. Cont Lens and Ant Eye. 2015;39:88-96. 10. Visser E-S, Visser R, van Lier H, Otten H. Modern scleral lenses part II: patient satisfaction. Eye Contact Lens. 2007;33:21-5. 11. Romero-Rangel T, Stavrou P, Cotter J, et al. Gas permeable scleral contact lens therapy in ocular surface disease. Am J Ophthal. 2000;130:25-32. 12. Mickles C, Harthan J, Barnett M. A surgace treatment solution for scleral lens wearers with dry eye. Presentation at the Global Specialty Lens Symposium. Las Vegas. January 2019. 13. van der Worp E, Graf T, Caroline PJ. Exploring beyond the corneal borders. Cont Lens Spectrum. 2010;25(6):26-32. 14. Ritzmann M, Morrison S, Caroline P, et al. Scleral shape and asymmetry as measured by OCT in 78 normal eyes. Poster presented at the Global Specialty Lens Symposium, Las Vegas, January 2016. 15. van der Worp E. A Guide to Scleral Lens Fitting, Version 2.0. Forest Grove, OR: Pacific University; 2015. Available: commons.pacificu.edu/mono/10/. Accessed April 21, 2020. 16. Jacobs DS, Rosenthal P. Boston scleral lens prosthetic device for treatment of severe dry eye in chronic graft-versus-host disease. Cornea. 2007;26(10):1195-9. 17. Schornack MM, Baratz KH, Patel SV, Maguire LJ. Jupiter scleral lenses in the management of chronic graft versus host disease. Eye Cont Lens. 2008;34(6):302-5. 18. Alipour F, Kheirkhah A, Jabarvand Behrouz M. Use of mini scleral contact lenses in moderate to severe dry eye. Cont Lens Anterior Eye. 2012;35(6):272-6. 19. Kumar P, Bandela PK, Bharadwaj SR. Do visual performance and optical quality vary across different contact lens correction modalities in keratoconus? Cont Lens Anterior Eye. March 29, 2020. [Epub ahead of print]. |


