 |
A 47-year-old male presented with poor vision. He had a corneal transplant 2.5 years ago to his right eye and a penetrating keratoplasty (PK) 10 years ago to his left eye for keratoconus. His right eye declined to the point where he could not wear contact lenses, so he had a deep anterior lamellar keratoplasty (DALK). He reported healing uneventfully from the recent transplant but said his vision was not satisfactory and he had not been able to correct it with contact lenses.
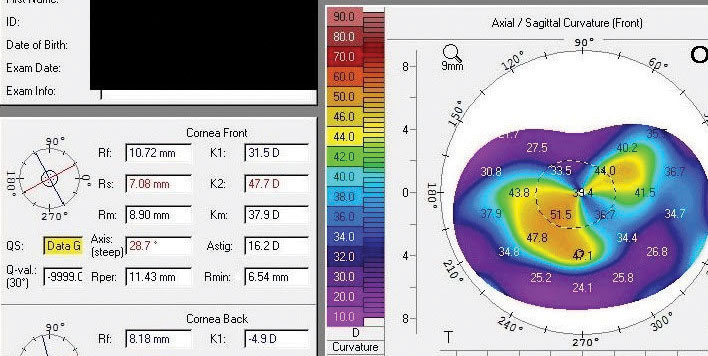 |
| The patient’s topography upon presentation. |
Preliminary Testing
The patient had an uncorrected visual acuity (VA) of 20/400 OD and a well-corrected VA of 20/25 OS with a hard lens. His entrance test results were normal, and he had intraocular pressures of 18mm Hg OU. I was unable to perform autorefraction on his right eye. After removing the rigid gas permeable (RGP) lens in his left eye, he was -1.50 -2.25x096 to 20/30. Manifest refraction yielded no measureable improvement in VA.
The slit lamp exam showed a DALK graft on the right eye, which was secured by a running suture around the circumference of the graft. It was healthy, clear and compact, as was the PK with no sutures. Deeper ocular structures were normal in both eyes.
Based on topography, the patient had 18.8D of astigmatism in his right eye, which was relatively regular centrally but became progressively more irregular the further from the central cornea.
The Problem
I diagnosed the patient with pathologic irregular astigmatism. The magnitude of this case deemed vision correction with an optical device unfeasible. If left untreated, the transplant would constitute an optical failure.
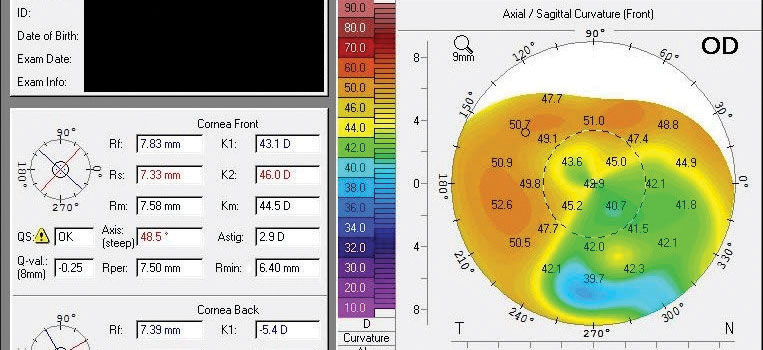 |
| The patient’s topography after total suture removal, subsequent corneal relaxing incisions at eight weeks post-suture removal and subsequent PRK. |
Solutions
Postoperative care for corneal transplants aims to achieve graft preservation and visual rehabilitation. We need to diagnose and treat allograft rejection to prevent the need for subsequent transplant. Visual rehabilitation beyond being fit with a hard lens is often an afterthought. However, high levels of astigmatism commonly follow these transplants, limiting uncorrected vision and, in extreme cases, correctable vision.
High astigmatism after PK and DALK is usually explained by the unequal tension placed on the sutures that secure the transplant, resulting in irregular corneal curvature. Discussed less frequently is host and donor graft trephination. The process of trephinating the donor and host tissues necessitates some pressure on the cornea, causing it to deform slightly as the blade passes through. This deformation occurs with both cuts (opening the host central cornea and creating the donor button) and is not uniform between them. Attempts are then made to join the two slightly different, imperfect circles, resulting in varying amounts of astigmatism.
Astigmatism could also be caused by “shaving” the anterior portion of a DALK graft or transplant to roughly match the thickness of the host cornea at the interface, which could be very thin in cases of keratoconus, to prevent an anterior overhanging ledge of the graft at the interface. In full-thickness grafts, this ledge can be placed in the anterior chamber where it doesn’t cause any issues. If left anterior in a DALK where it cannot be pushed posteriorly by the presence of the patient’s own Descemet’s membrane, this ledge can result in problems with epithelization. Manually “shaving” the donor tissue can result in scar tissue, producing irregular astigmatism.
Combining these elements causes varying degrees of astigmatism. In cases of worse-than-average astigmatism, surgical remediation may be required before using an RGP or scleral lens. In extreme cases, a single intervention effort may not be able to treat the magnitude of cylinder, so it is important to understand the surgical steps to take and the order in which to take them.
Our facility approaches extreme levels of post-transplant astigmatism in a stepwise fashion, moving from less precise to more precise options, that begins with removing all remaining sutures.
Your options include:
- Suture adjustment or removal to create long-term corneal stability.
- Corneal relaxing incisions to induce flattening. Because corneal relaxing incisions are more central (just central to the graft host interface), they tend to be more impactful than limbal relaxing incisions.
- Compression sutures to induce steepening.
- Wedge resections to induce marked steepening. Removing a thin (0.1mm to 0.2mm) wedge of donor tissue from near the graft host interface with subsequent suturing causes steepening.
- Excimer laser ablations, or phototherapeutic keratectomy, to treat transplant eyes that have pathologic refractive with LASIK or photorefractive keratectomy (PRK).
Though suture adjustment with running sutures or selective suture removal with interrupted sutures may fine-tune astigmatism early on, the magnitude of the effect of these interventions is usually smaller later in the postoperative course. Further, if surgical intervention is pursued to treat pathologic astigmatism prior to suture removal and a suture breaks, the effect of surgery will be diminished. Removing all sutures creates long-term stability for the cornea, which is important if a subsequent refractive surgery is performed. Though sutures with DALK grafts can often be removed safely one year postoperative and those with PK grafts by 36 months, a corneal specialist should determine when and if sutures can be removed to avoid creating graft dehiscence if they are removed prematurely.
The impact of suture removal on astigmatism is unpredictable, so we must inform patients that removal may result in their astigmatism worsening but is performed to create a stable cornea for subsequent treatments. After sutures are removed, the patient should not undergo further treatment for several months as the cornea stabilizes. Repeat the process of manipulating the cornea and waiting for stability after each subsequent procedure.
In my opinion, these efforts should conclude with excimer laser ablation, which is the most precise technique. Post-transplant excimer laser ablation limitations, however, do exist. First, treatment accuracy with excimer laser ablation is far from the level achieved with conventional treatments in normal eyes, with one study reporting an average cylinder reduction of less than 50%.1 Second, the ability to treat high amounts of astigmatism is limited by the treatment zone of all excimer laser applications. As the magnitude of cylinder increases, the treatment zone becomes more oval-shaped. At significantly high levels of treatment, the size of this oval becomes thin enough to create diminishing returns in treatment. Thus, the amount of cylinder you treat with excimer laser-based treatments should be no greater than 6.0D to 7.0D. Due to the limited magnitude of treatment offered by laser vision correction, we begin with incisions, compression sutures and/or wedges and move to PRK as needed.
Aftermath
We followed these steps to treat this patient. All sutures were removed, and relaxing incisions were placed four months later. Six months later, PRK was performed. At the conclusion of this process, the patient’s uncorrected vision was 20/60, and he had 2.9D of moderately irregular cylinder and could correct to 20/40 with glasses and 20/20 with contact lenses.
As ODs, we put a lot of pressure on ourselves to fit post-transplant eyes with contact lenses; but, sometimes, the magnitude of cylinder precludes the ability to fit a hard lens. Unless a surgery center is able to mitigate the astigmatism, the graft will fail. Knowing your options and being aware that astigmatism improvement, but not always cylinder elimination, is attainable will allow you to educate patients appropriately and refer them in a timely fashion.
| 1. Bilgihan K, Ozdek SC, Akata F, et al. Photorefractive keratectomy for post-penetrating keratoplasty myopia and astigmatism. J Cataract Refract Surg. 2000;26(11):1590-5. |


