  |
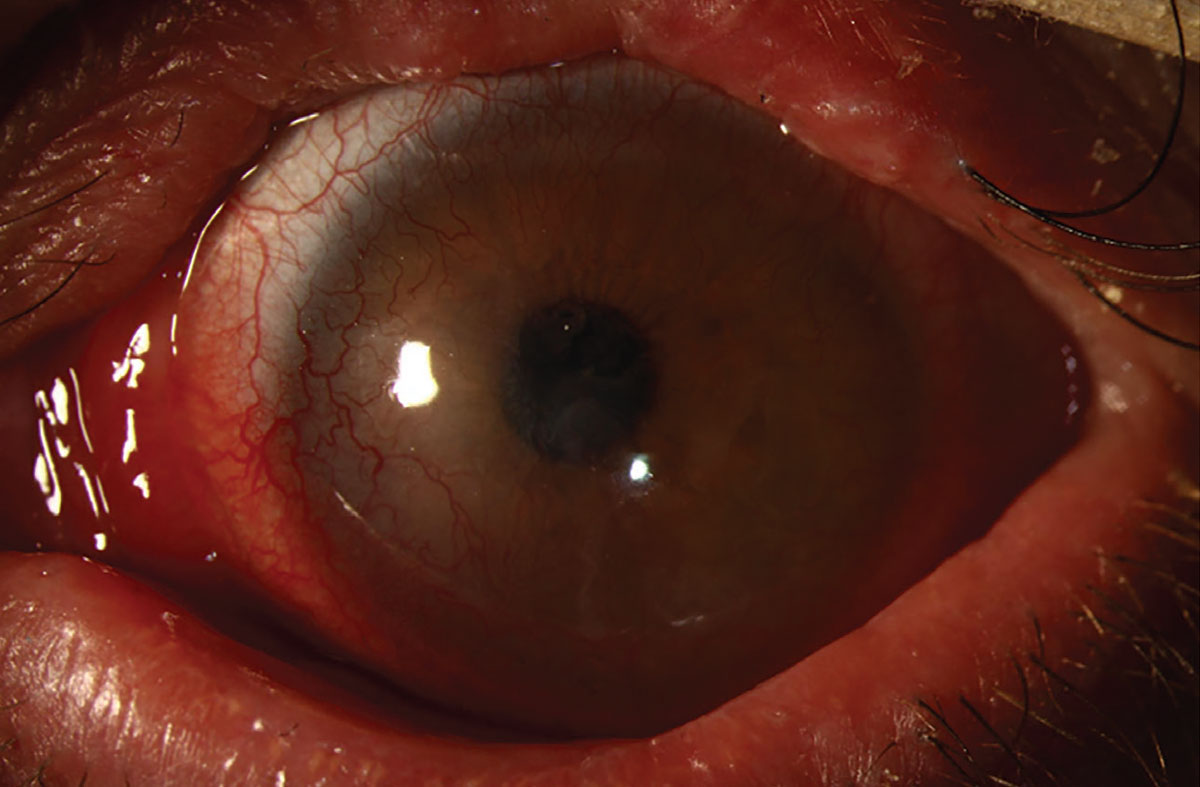
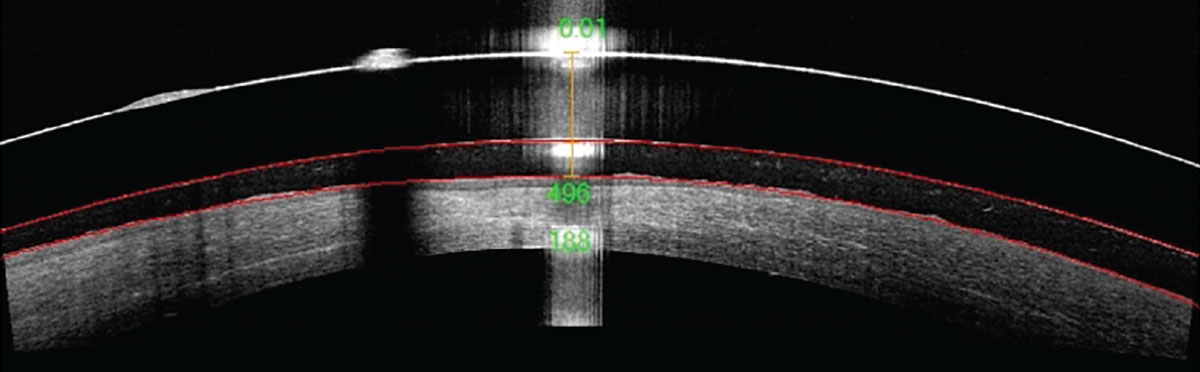
A 30-year-old patient presented to the contact lens (CL) clinic with a history of Stevens-Johnson syndrome (SJS). His chief complaints included chronic pain, blurry vision and dryness of the left eye. His entering best-corrected visual acuity (BCVA) was 20/20 OD and 20/200 OS. Slit lamp findings OD were grossly normal; however, the left eye revealed diffuse peripheral interstitial neovascularization and pannus with diffuse punctate epithelial erosions and a central, round opacity about 0.75mm in diameter. He was then fit into a scleral lens in the left eye only, achieving a BCVA of 20/60 (Figures 1 and 2). He successfully underwent proper insertion and removal training along with lens hygiene instructions.
Considerations
Here, we highlight our thought process and consider how we would proceed:
Dr. Noyes: Ocular surface disease patients, such as those with SJS, can be very difficult to manage, especially when there are high levels of inflammation. The eye is a living, breathing tissue and can easily change shape when inflammation is present. This can sometimes go as far as causing the development of symblepharon, nodules, significant corneal thinning and/or scarring. These patients require close observation to maintain the integrity of their ocular surface, and proper lens care instructions are vital to prevent further inflammation and infection.
 |
|
Fig. 1. Slit lamp photo of the patient’s left eye with a scleral lens in place. Click image to enlarge. |
Dr. Su: One of the most distressing aspects of SJS is its impact on the eyes, causing SJS-associated ocular surface disease. This can lead to significant complications, including severe dry eye, conjunctivitis, corneal erosions and scarring. Scleral lenses can play a crucial role in managing these patients—they offer several benefits by providing a smooth optical surface that masks the irregularities on the cornea, improving visual outcomes. The reservoir of saline solution under the lens helps to maintain a stable tear film, reduce dryness and protect the surface by allowing healing. Large-diameter soft lenses can also be helpful in providing relief by covering a greater area of the cornea and surrounding sclera.
In addition to CLs, other treatments of lubricating or serum tears, amniotic membranes, anti-inflammatory medications and surgical interventions may be necessary to manage ocular complications and optimize visual outcomes in individuals with SJS. A multidisciplinary approach involving eyecare practitioners and rheumatologists is essential to address the complex visual and ocular health needs of these patients.
Dr. Pfeifer: Working with patients suffering from SJS and examining their eyes can reveal how difficult dealing with the condition can be. Many of these patients are so desperate for relief of their symptoms. They will often need numerous therapies from drops to plugs to amniotic membranes and beyond. In addition to symptoms of dryness and pain, insults to the cornea may result in opacities or irregularities that cause visual distortion or blur. Luckily, one treatment modality aims to combat both of these challenges, that being scleral lenses.
 |
|
Fig. 2. OCT of the patient’s scleral lens fit on the left eye. Click image to enlarge. |
Ideally, patients with SJS will be fit using a “large and loose” philosophy to cover as much of the ocular surface as possible. A looser fitting lens or one with incorporated fenestrations or channels will ensure a greater supply of oxygen to the cornea to reduce the stimulus for greater neovascularization. As many patients feel relief in these lenses, it’s important to stress that they should not overwear the lens and should refresh the scleral filling solution multiple times throughout the day to ensure good quality and clarity of the post lens tear film. Cleaning should be emphasized, with importance placed on rubbing the lens to ensure removal of deposits. Patients should also be educated on the importance of monitoring for any change in their symptoms, including redness, tearing, pain and light sensitivity, as well as be advised to seek urgent care if change or worsening occurs.
These patients should be followed closely, and frequent communication with doctors comanaging their condition will give them the best chance at stabilization and improvement.
Dr. Gelles: SJS patients go through a lot, and lifelong issues can be a lot to bear; being able to provide improved comfort and vision can improve their quality of life more than you may imagine. SJS patients are generally in some level of pain, so relieving it and allowing the ocular surface some time to heal is our number one goal—if we can improve vision too, this will be an especially impactful treatment.
In these cases, scleral lenses are my first choice. The large diameter provides significant protection from the trichiasis, scarred lids and scarred palpebral conjunctiva. The fluid reservoir underneath can provide an opportunity for the cornea to heal and break the pain cycle. Generally, the more tissue covered the better, but some of these patients will have formed a symblepharon that can limit lens diameter. The big issue to look out for is interaction with symblepharon and resting on the limbus, causing further exacerbation of limbal stem cell deficiency—this is the double-edged sword of scleral lenses. If a scleral lens is just not possible, I would consider either large diameter soft lenses to achieve protection by ocular surface coverage or standard bandage soft lenses.
Results
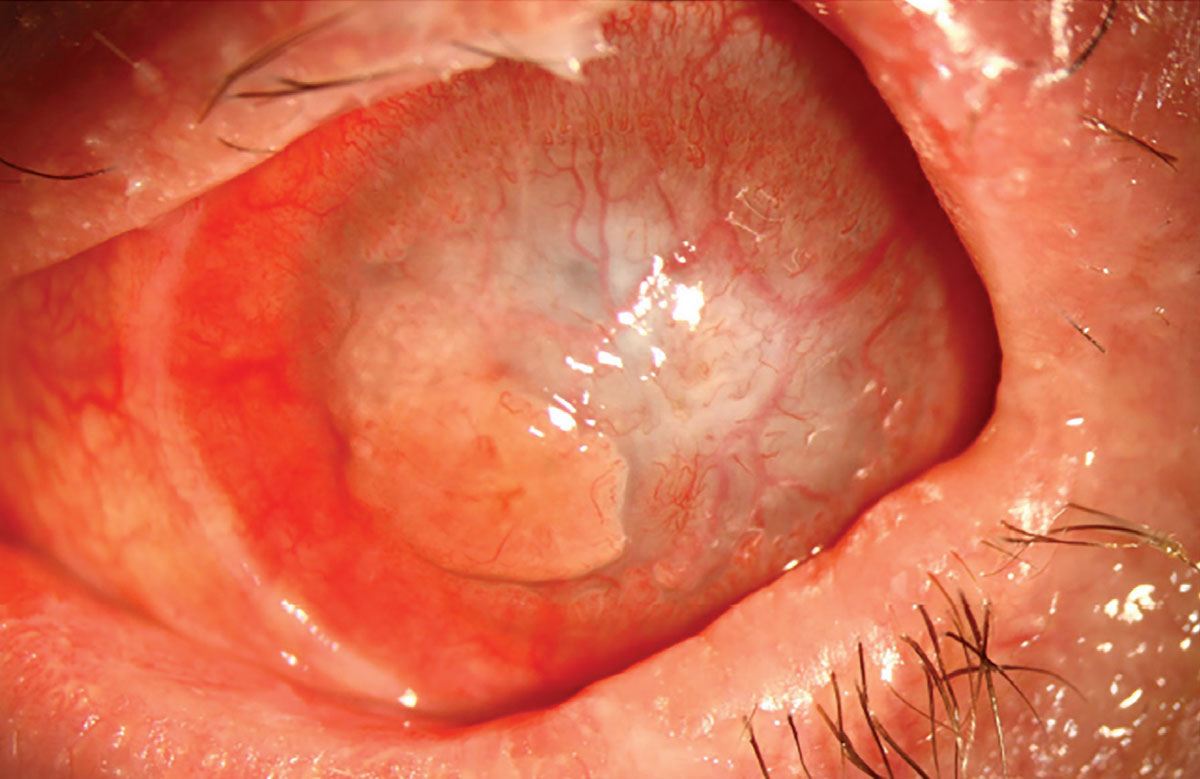
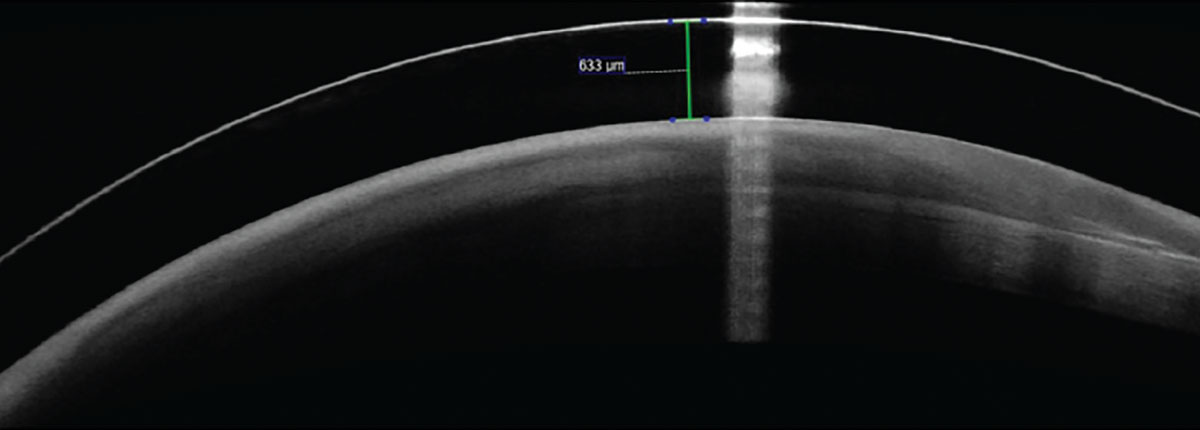
The patient was unfortunately lost to follow-up but returned six years later for another evaluation with the chief complaint of reduced vision. His entering BCVA was light perception and he reported that he had not removed his scleral lens since his previous visit six years prior. His entire cornea had become conjunctivalized, diffusely opaque and he had a large pyogenic granuloma concentrated inferiorly (Figures 3 and 4). At this point, he was referred to our cornea and oculoplastics services for evaluation and treatment, ultimately ending in complete tarsorrhaphy OS. The final outcome remains unknown but may include transplantation or even keratoprosthesis.
 |
|
Fig. 3. Slit lamp photo of the patient’s left eye six years later, showing conjunctivalized cornea and pyogenic granuloma. Click image to enlarge. |
Discussion
SJS is an acute, severe and potentially fatal mucocutaneous hypersensitivity reaction causing widespread epidermal detachment and necrosis. This blistering of the skin and mucous membranes is immunologically mediated and most commonly caused by medications—specifically anticonvulsants, antibiotics, sulfonamides, acetaminophen and nonsteroidal anti-inflammatory drugs.
SJS is characterized by the extent of surface area of the body affected. When less than 10% of the body is involved, the reaction is called SJS; when more than 30% of the body is involved, it is called toxic epidermal necrolysis (TEN), and SJS/TEN is the classification for cases that fall between 10% and 30% of affected area.
Acute management relies on intensive care, but mostly supportive therapies with wound care, pain control and fluid resuscitation. The most critical part of acute management is identifying the cause of the reaction and stopping exposure. Long-term issues associated with SJS are mostly the result of significant scarring of affected areas. Those with ocular sequelae suffer from a variety of issues, from symblepharon, conjunctival and corneal scarring, conjunctivalization of the cornea, trichiasis and even sequelae of each of those conditions. The result is pain, and any lens that can act as a bandage can be a miracle for the patient.
 |
|
Fig. 4. OCT of a scleral lens over the patient’s left eye. The corneal surface has become completely conjunctivalized. Click image to enlarge. |
However, this relief can lead to overwear and complications—too much of a good thing. Seeing these cases can often be disheartening from a practitioner perspective, as this outcome can be entirely avoided by maintaining proper follow-up on the condition and care of the CLs. All CLs require a proper care regimen, as poor hygiene can lead to a plethora of complications, from giant papillary conjunctivitis, inflammatory infiltrates, microbial keratitis, limbal stem cell deficiency and more. We must remind our patients that contact lenses are medical devices, and in this case a medical device crucial in restoring ocular health and reducing ocular pain, but if not cared for correctly, one which can worsen the situation. In this scenario, the resultant lack of care and follow-up led to a disastrous outcome.
Dr. Su is the Cornea and Contact Lens Fellow at the Cornea and Laser Eye Institute (CLEI) Center for Keratoconus. She has no financial interests to disclose.


