 |
I have always been fascinated by this rare complication of keratoconus, and recently it has come up more frequently in my practice. Hydrops, a complication of corneal ectasia, presents as a sudden onset of corneal edema following a rupture of Descemet’s membrane and endothelium, leading to an influx of aqueous humor into the stroma.1 Overall, acute corneal hydrops is exceedingly rare, but do consider differentials such as infectious keratitis, uveitis, post-surgical trauma, endothelial dysfunction and acute transplant rejection episodes.1
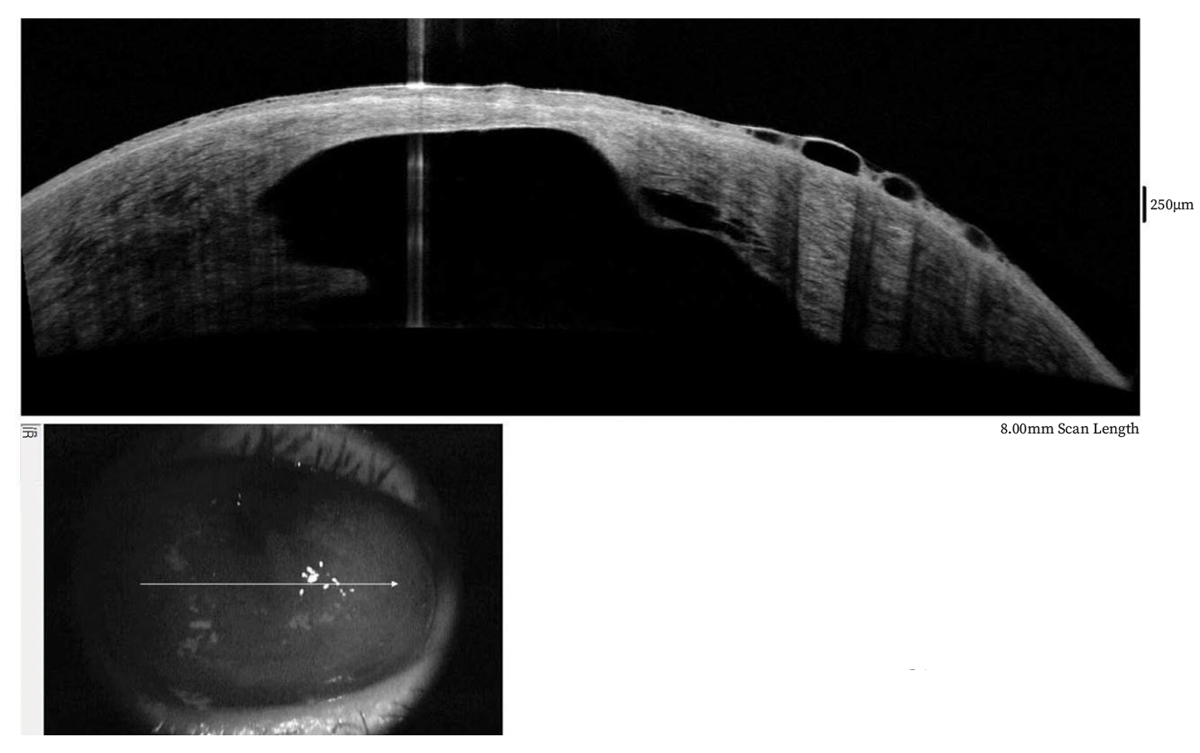
Along with a history suggestive of a sudden loss of acuity, a slit lamp examination is often all that is needed to make a diagnosis. However, anterior segment OCT, in vivo confocal microscopy, ultrasound biomicroscopy and tomography can also help (Figure 1).1,2
The rate of acute corneal hydrops ranges from 0.2% to 2.8% in keratoconus and other non-inflammatory thinning disorders, more commonly seen in ages 20 to 40 and doubly so for males.1-3 Risks for acute hydrops include eye rubbing, elevated IOP, steep corneas, Down syndrome and corneal variances, such as stromal thinning, hyperreflective abnormalities and absence of scarring.1-3 Patients typically present with a spontaneous decrease in acuity as well as pain and light sensitivity precipitated by coughing, sneezing, nose blowing and other activities that can increase IOP.2 To minimize risk, tell patients to avoid eye rubbing, treat their allergies and reduce chance of thinning and steepening in keratoconus early with crosslinking, when appropriate.
 |
|
Fig. 1. OCT was taken three weeks after initial loss of acuity. Note surface epithelial edema/bullae and large posterior corneal defect with irregular contour. A water cleft separates the posterior stroma from Descemet’s membrane. Click image to enlarge. |
Peculiar Combination
It’s simply an observation, but I have documented three new cases of acute corneal hydrops in my scleral lens wearers with keratoconus in the past seven months compared with two new cases in the past decade. I’m not suggesting scleral lens wear is causative, but with this uptick, scleral lenses are all that’s changed for me. Still, it’s interesting that my last three patients have all been neophytes younger than 40 with no previous scarring. Might these lenses in some fashion increase risk for acute hydrops in a select group?
In a case series, hydrops was noted in several patients who developed ectasia following penetrating keratoplasty. The authors suggested scleral lens wear played some role in that.5 Maybe new wearers may not fully grasp how to insert and remove without inducing some trauma. Regardless, counsel patients to not rub, massage or even touch their eyes and constantly assess for any precipitating mechanisms for IOP elevation.2 Also, emphasize caution in avoiding hard suction on lens removal.
If hydrops occurs, manage patients carefully. Its pathophysiology, time to resolution and ultimate outcome can vary widely. Topical remedies include steroids, cycloplegia, hypertonics, IOP reduction agents and antibiotic prophylaxis. Eye patching and IOP reduction is helpful with a nonperforation positive Seidel sign.4 Surgical options include pneumatic descemetopexy for reattachment with air/gas, compression sutures to reapproximate Descemet’s membrane, as well as endothelial, anterior lamellar and penetrating keratoplasties.
Am I just imagining this increase or is it truly happening? Are you seeing more hydrops now compared with years past? I’d love to hear from you.
1. Bunya BY, Bernfeld E, Hakim F. Acute corneal hydrops. EyeWIki. eyewiki.aao.org/acute_corneal_hydrops. Updated September 11, 2022. Accessed April 19, 2023. 2. McMonnies CW. Mechanisms for acute corneal hydrops and perforation. Eye Contact Lens. 2014;40(4):257-64. 3. Barsam A, Brennan N, Petrushkin H, et al. Case-control study of risk factors of acute corneal hydrops in keratoconus. Br J Ophthalmol. 2017;101(4):499-502. 4. Sharma N, Maharana PK, Jhanji V, Vajpayee RB. Management of acute corneal hydrops in ectatic corneal disorders. Curr Opin Ophthalmol. 2012;23(4):317-23. 5. Murillo SE, Shariff A, Lass JH, Szczotka-Flynn, LB. Acute corneal edema decades after penetrating keratoplasty for keratoconus in eyes wearing scleral contact lenses. Cont Lens Anterior Eye. 2021;44(1):108-14. |


