Offering optimal visual acuity and contrast sensitivity, as well as a lower risk of complications, gas permeable (GP) lenses are an effective option for many patients, particularly those with high corneal astigmatism. Evidence also suggests this modality is better tolerated among patients with dry eye compared with soft contact lenses.1 However, only about 10% of contact lens wearers use these lenses.1 This discrepancy is thought to be a result of a combination of challenges, including the initial discomfort associated with rigid lenses and the time it takes to successfully fit and manage patients who must deal with the adaptation period.
“GP lenses should be a key component of any contact lens practice, especially for those who offer specialty contact lenses and manage presbyopia and irregular corneal surfaces,” notes Joseph Shovlin, OD, of Northeastern Eye Institute in Scranton, PA. “You just can’t satisfy most patients with soft lens options when the cornea is severely distorted.”
Dr. Shovlin urges optometrists to recognize that they do have the time and knowledge to fit these lenses. “Yes, they are more challenging most of the time and do often require additional chair time, but clinicians are adequately educated to fit GP lenses and will find it incredibly rewarding,” he adds. He emphasizes the variety of resources available to ODs to help them get started, including tutorials and guides.
Given the plethora of research available regarding contact lenses, the British Contact Lens Association (BCLA) gathered more than 100 multidisciplinary experts to review and summarize the current literature in the Contact Lens Evidence-based Academic Reports (CLEAR). In a series of 10 articles, CLEAR covers topics focusing on contact lens materials, designs, optics, medical uses, evidence-based practices and future technologies.1
“BCLA CLEAR is both an impressive compendium and a comprehensive review on all aspects of lens wear with complete discussions on pre-fit considerations and managing contact lens wearers over time,” says Dr. Shovlin. “For example, it helps in making clinical decisions using appropriate evidence ranging from who the most appropriate candidates for assorted types of lens wear are and how we best care for these patients once they start wearing lenses in order to minimize complications and avoid eventual dropouts.”
In this article, we will delve into CLEAR, highlighting key takeaways while also discussing how ODs can use the information and strategies detailed in the report to up their management of GP lenses, or rigid corneal lenses—the terminology recommended by the authors of CLEAR.1
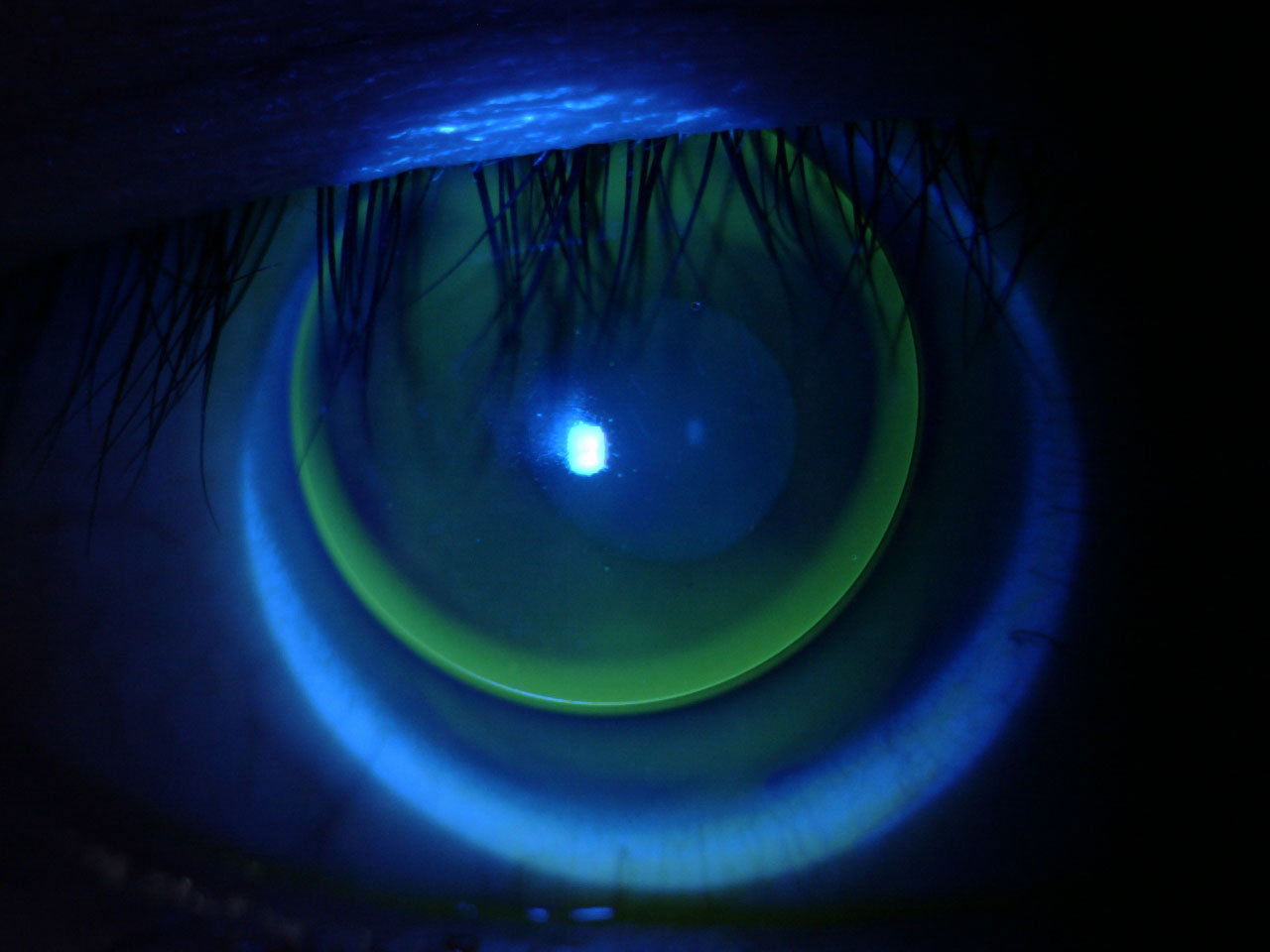 |
The available literature on GPs is extensive, and CLEAR aims to consolidate it all. Photo: Lindsay Sicks, OD. Click image to enlarge. |
Clinical Pearls
Taking an evidence-based approach to rigid corneal lenses is crucial to success for both ODs and their patients because it incorporates not only the best research and scientific evidence from the literature, but also—in theory—the patient’s values, preferences and needs, along with the clinician’s judgment, expertise and experience, explains Lindsay Sicks, OD, of the Illinois College of Optometry.
“This report is rich in content for GPs and sclerals,” she notes. “It’s a comprehensive review of the best strategies and things to think about in terms of case history, anterior segment evaluation, contact lens selection (with ortho-K, scleral lenses and medical use of lenses covered in separate reports), lens fit evaluation, prescribing/dispensing practice and aftercare advice.”
Successful contact lens fitting begins by recognizing the multitude of factors that can impact it, including patient age, thyroid disease, smoking status and medication use. Always discuss family ocular history, since it can inform management of myopia, keratoconus, corneal dystrophies and diabetes—all of which can have an effect on contact lens wear, says Dr. Sicks.
“Eyelid eversion is a necessary component of not only initial fitting but also the aftercare process,” she adds, while discussing the key takeaways from the report. “It’s important to avoid iatrogenic staining when everting the lid, and studies have shown a special everter made of silicone rubber is superior to even our fingers for lid eversion as more of the lid is exposed. Another important factor is instilling NaFl, as the grading of palpebral roughness is significantly higher when assessing with NaFl and blue light vs. just white light.”
Another key component of contact lens fitting is a thorough examination of the anterior eye. “Ocular/anterior segment photography allows for objective grading of digital images, which has the potential to decrease the variability of subjective ratings,” explains Dr. Sicks. “It can also be employed for patient education to help explain ocular changes to patients and keep them fully informed.”
When it comes to rigid corneal and scleral lens fitting, fluorescein dye allows for visualization of the tear film. Also, it penetrates the corneal epithelium to help visualize epithelial disruption, according to the authors of the report. “If excess fluorescein is instilled, the stimulated molecules collide, reducing the fluorescence; hence, the recommended technique is to place a drop of saline onto the paper strip, then shake the strip to remove the excess liquid,” they wrote. They also explained that the strip should be applied flat and at the temporal canthus to avoid damage to the tissues under observation.
The CLEAR report provides evidence to help ODs better determine if soft or rigid contact lenses are the right choice for their patient, depending on health conditions, past treatments/surgeries and medications. For instance, the study authors report strong evidence supporting the use of rigid corneal or reverse geometry lenses when corneal irregularities are present in patients post-refractive surgery.
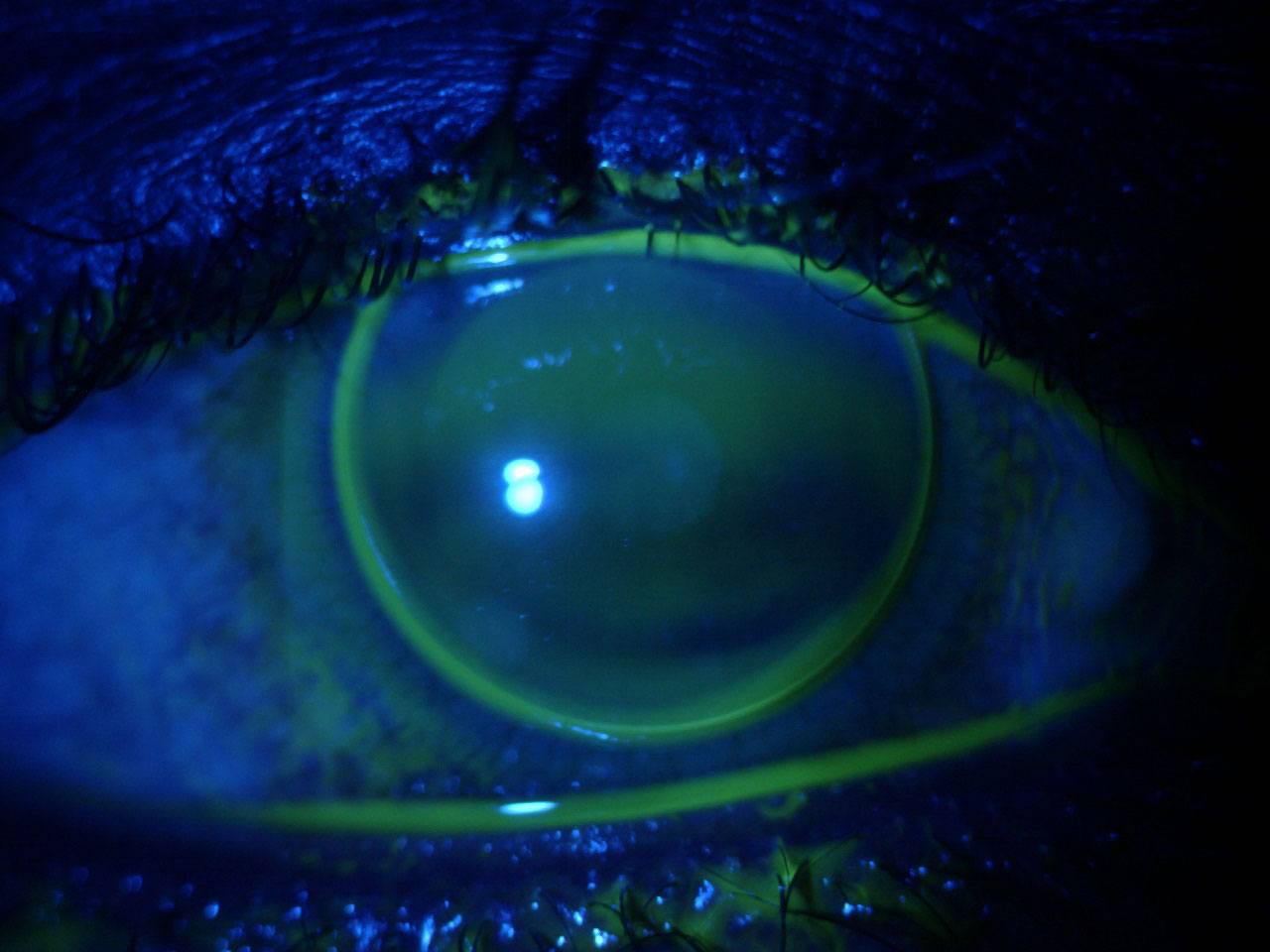 |
The report details how to determine whether a patient is an ideal GP candidate. Photo: Lindsay Sicks, OD. Click image to enlarge. |
A thorough, systematic approach to rigid corneal lens fitting is outlined by the authors as follows:1
- Comfort: 0 (extreme discomfort) to 10 (no lens sensation)
- Coverage: +2 to -2 (based on size relative to the horizontal visible iris diameter)
- Centration: L (crosses limbus)/P (crosses dim pupil)/C (contained within limbus)
- Movement inter-blink: +2/>2mm to -2/<0.5mm
- NaFl pattern with the lens centered: +2 steep to -2 flat
- Edge width: +2/>2mm to -2/not visible
While properly fitting rigid corneal lenses is important, ODs also have to take the time to help set their patients up for success once they leave their office. This should include adaptation advice prior to dispensing the lenses, according to the CLEAR report.
Rigid corneal lenses are more often associated with poorer initial comfort and longer adaptation times; ODs need to identify strategies to meet this challenge. Anesthetic use during rigid lens fitting appointments can improve initial comfort as well as reduce dropouts and anxiety; however, the CLEAR authors report that a survey of UK eyecare providers showed that less than 1.5% used anesthetic regularly and less than one-third considered it a clinically acceptable approach.1
Providing a comprehensive patient education, including a discussion on modifiable risk factors, can make a significant difference when it comes to successful compliance. This includes information on hand-washing, sleeping in lenses, solution use, replacement interval, case cleaning, rubbing and rinsing, use of tap water and annual exams.
“It’s always important to realize there are modifiable factors and non-modifiable factors that ultimately affect lens wear success,” notes Dr. Shovlin. “We have to live and deal with the non-modifiable factors, such as lid anatomy/characteristics and corneal features, to name a few. We can at least attempt to alter modifiable factors in order to maximize comfort and vision.”
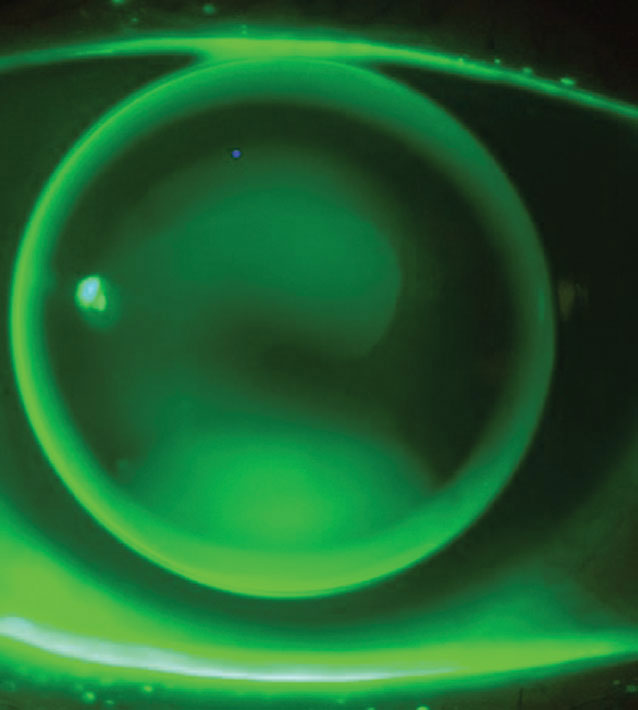 |
The report covers soft vs. rigid corneal lenses and the efficacy of each in different patients. Photo: Tiffany Andrzejewski, OD, and John Gelles, OD. Click image to enlarge. |
Implement the Evidence
Fitting and managing rigid corneal lenses in practice is often a challenge, but using an evidence-based approach can help optometrists lay the foundation for overall success. This includes maintaining a strong understanding of current literature, while also recognizing what seems to work the best for your individual practice and patients.
Staff members also play a key role in the ongoing success and optimization of GP lenses in practice, especially during the aftercare process, according to Dr. Sicks, who urges optometrists to use their team to ensure all the necessary information is gathered so no issues or concerns are missed during follow-up appointments and exams.
“Equally important is the mindset of the optometrist. Success depends not only on the skills of the practitioner, as well as the lens material and design, but also on their attitude and how information is being presented to the patient,” Dr. Sicks concludes. “We have to make sure we are considering these lenses for the right patients. There are definitely individuals who could benefit from GP lenses, and by offering this option, we are providing the highest level of care possible to our patients.”
1. Wolffsohn JS, Dumbleton K, Huntjens B, et al. CLEAR—evidence-based contact lens practice. Cont Lens Anterior Eye. 2021;44(2):368-97. |