The annual Association for Research in Vision and Ophthalmology (ARVO) meeting is always a boon for the eye care profession. Clinicians gain access to an entire year’s worth of research—which can be both exciting and daunting. Here, we have selected studies we feel may be most impactful for practicing optometrists and reviewed a handful of abstracts. While the new tools, therapies and management strategies recapped here only give a small taste of the findings showcased in Vancouver, even this brief showcase—15 abstracts in all—packs in many exciting new ideas.
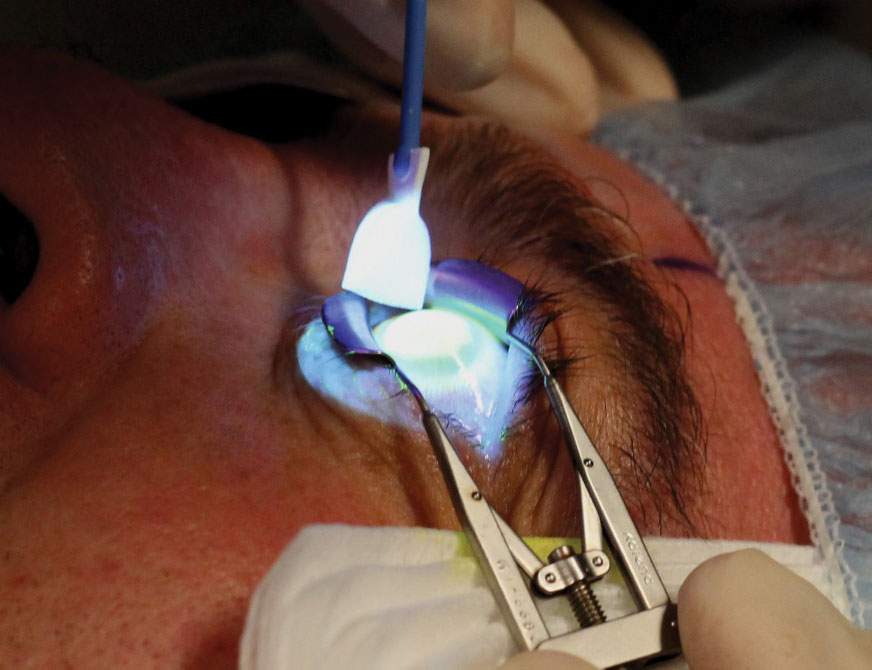 |
| A-CXL, which uses a higher UVA irradiation for a shorter amount of time, was found to have fewer risks of corneal flattening. Photo: Marshall Ford, MD, Pacific Cataract and Laser Institute |
Keratoconus
Several researchers took a close look at the pathophysiology and management of keratoconus:
Pathophysiology. A team of researchers found that keratoconus patients with a European background presented with less severe indicators of disease compared with keratoconus patients of Indian or Asian descent. This observational study recruited keratoconus patients from public and private ophthalmology clinics in Australia, Hong Kong and India. The team evaluated 1,472 eyes of 736 patients. Of these, 55% were European, 18% were Asian, 18% were Indian and 9% were other ethnicities.1
While researchers found no statistical difference in age of onset between European patients compared with each of the other ethnic groups, they did note that Indians tended to be older at onset. The team observed that the mean anterior corneal curvature was flatter among Europeans, and the spherical equivalent was least severe. The mean corneal pachymetry was thinner among Indians than Europeans and Asians at the apex and the thinnest location.1
“These findings have important clinical implications when interpreting studies from different regions and contribute to the understanding of risk factors and future management strategies of keratoconus,” the study authors conclude.1
“A global registry would be helpful to define additional differences that may aid in patient management,” says Joseph Shovlin, OD, of Northeastern Eye Institute in Scranton, PA.
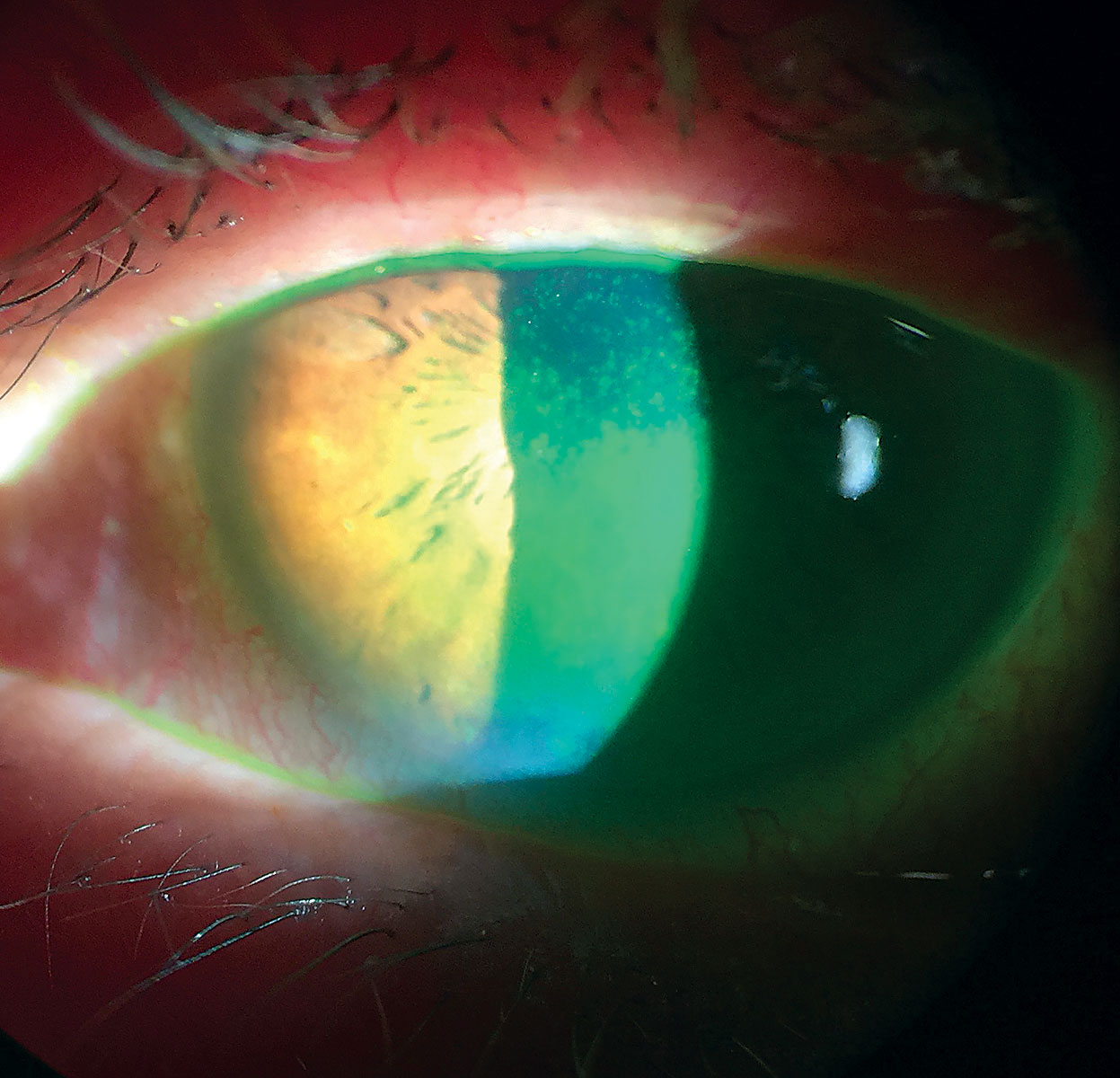
Management. Researchers recently found that patients who wear scleral contact lenses for keratoconus had a significantly lower risk of requiring keratoplasty, which may warrant the lenses’ wide-scale use for the condition.2 The team noted that 2.03% of patients wearing scleral lenses required keratoplasty, compared with 6.82% of those who did not wear scleral lenses.2 Lens wear was also associated with a 72.7% decreased risk of requiring keratoplasty.2 They add that other factors associated with an increased risk for keratoplasty included black race (vs. white), younger age and lower socioeconomic status of a participant’s residential neighborhood.2 “Scleral lenses have changed the treatment paradigm in managing patients with non-inflammatory thinning disorders, such as keratoconus, primarily because they provide exceptional comfort and vision,” says Dr. Shovlin. “Most transplants are a result of patients not achieving comfort or adequate vision with contact lens correction.”
Investigators from Japan say accelerated corneal collagen crosslinking (A-CXL) has the added benefit of causing less haze and fewer long-term risks of continuous flattening. Doctors and patients alike have reason to prefer the A-CXL protocol, they feel, because it reduces procedure time, as long as outcomes aren’t compromised relative to conventional CXL.3
The team of researchers looked at 22 eyes of 21 progressing keratoconus patients who underwent epithelium-off CXL treatment. Twelve eyes of 11 patients underwent conventional CXL, which involves a 0.1% riboflavin instillation and a 3.0mW/mm2 UVA irradiation for 30 minutes. The other 10 underwent A-CXL, which uses a higher-intensity 18mW/mm2 UVA irradiation for only five minutes.3
While best-corrected visual acuity (BCVA), thinnest corneal thickness and corneal endothelial cell densities were similar between the two groups, steepest K values were significantly different, with the conventional CXL patients showing more flattening compared with the A-CXL patients at one year—and the difference increased through the five-year study period. Also at five years, 58.3% of the conventional CXL group had flattening Ks of more than 1D—none in the A-CXL group exhibited the same finding. Finally, corneal densitometry was significantly higher after conventional CXL than A-CXL from one month to one year after the procedure.3
“With similar efficacy, the abbreviated/shorter version should be employed to reduce risk,” says Dr. Shovlin.
Another study discovered that significant changes in the inflammatory molecular profile occur at least one month after CXL. Researchers from Mexico found decreases in proinflammatory cytokines, especially metalloproteinase-9 (MMP-9), c-reactive protein (CRP) and interleukin-19. The study assessed 40 eyes of 20 patients, of which 20 underwent A-CXL. Researchers analyzed patients one day, one week, one month and three months after the procedure. After one month, they found a more-than-twofold decrease in specific cytokines in patient tears. More proinflammatory cytokines also began to decrease by three months. Researchers believe studies with longer follow-up will help prove whether these changes last and how they correlate with clinical outcomes.4
A study conducted in Germany suggests practitioners examine keratoconus patients at regular intervals, especially five years after performing CXL, to recognize and re-treat progression early. Researchers defined a satisfactory response to CXL as a postoperative Kmax stabilization of an increase of more than 2D or any decrease in Kmax. They analyzed 168 eyes of 131 patients who were treated with standard CXL.5
After CXL, median K2 increased by 0.1D after one year but decreased over the remaining 10-year postoperative period by 0.85D. Mean apical corneal thickness decreased by 11µm, 9µm and 3µm after three, seven and 10 years, respectively. Mean BCVA significantly increased by 0.14 after two years and by 0.15 after five and 10 years. One, seven and 10 years post-CXL, 87.8%, 81.1% and 66.7% of eyes met the responder criteria, respectively. The researchers re-treated four eyes. There were no complications in repeating CXL, and keratoconus stabilized afterward.5
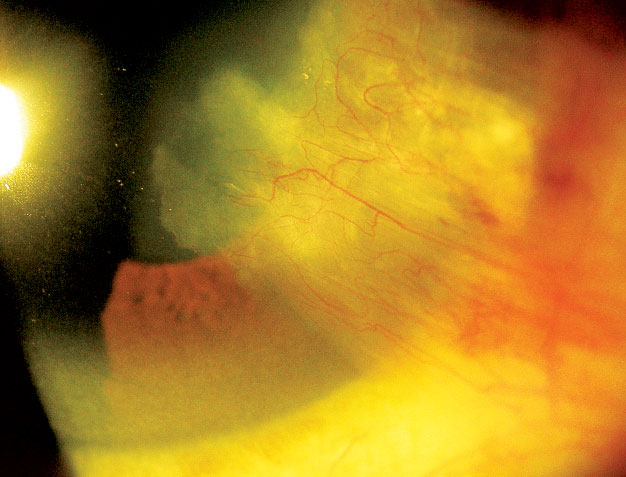 |
| One study disproved the popular peripheral light–focusing effect theory for pterygia formation. Photo: Andrew Gurwood, OD |
Other Corneal Complications
To help differentiate keratoconus from pellucid marginal degeneration (PMD), Iranian researchers found that four fundamental parameters could be considered as diagnostic signs to characterize all stages of PMD, including subclinical disease:6
An inferior flattening island, defined as the flattening area surrounded by steep areas inferior to the horizontal axis.
An apple-shaped pattern formed by mean power area as a yellow strip.
Superior flattest area, defined as the presence of the flattest area at the superior quadrant.
Against-the-rule irregular astigmatism (flat meridians at 45 to 135 degrees).
Additionally, the investigators noticed that measuring the extent of the inferior flattening island could be helpful for staging PMD and identifying early PMD. Based on these parameters, investigators were able to differentiate 36 cases of PMD from keratoconus.6
“Some patients with keratoconus have similar features depending on the level of severity,” says Dr. Shovlin. “The most definitive way to differentiate would be to look at higher-order aberrations where PMD has a high level of trefoil and keratoconus has more vertical coma in general.”
Pterygia are more common on the nasal side of the cornea than the temporal side—15 times more likely, to be precise. But researchers aren’t quite sure why. One group found that total UV irradiation in the nasal limbus is not greater than in the temporal limbus, contrary to popular belief. The team created a corneal model using custom software and the corneal surface and UV refractive index data from a previous study to simulate the impact of the UV across the cornea.7
“This study essentially rules out the peripheral light focusing effect theory for pterygia formation,” explains Dr. Shovlin. The researchers offer an alternative explanation: that the temporal-to-nasal flow of tears over the UV-exposed cornea causes the accumulation of toxins on the nasal limbus.7
“If this theory is correct, additional ocular surface disorders may be explained by the temporal-to-nasal tear flow dynamics to facilitate drainage to the punctal area,” adds Dr. Shovlin.
 |
| A cytokine coating for soft lenses could provide sustained dry eye treatment. Click image to enlarge. Photo: Scott G. Hauswirth, OD |
Dry Eye
Many of the dry eye advances presented at ARVO focused on new diagnostic tools:
A new hyperspectral imaging method can measure the mucoaqueous layer thickness as well as other tear film functions. The tear film imager (TFI) is designed to give doctors objective and observable measures to aid the diagnosis and management of dry eye disease (DED). The TFI, which takes approximately 40 seconds, can measure patients’ aqueous layer thicknesses and averages at a nanometer level. Additionally, it can measure the lipid layer thickness at a sub-nanometer level and establish average thickness and lipid break-up time (LBUT).8
The international team of investigators found that the TFI method could accurately diagnose DED with 87% sensitivity and 88% specificity. Of particular interest, the reproducibility of the mucoaqueous layer thickness measurement, which has not been evaluated with any prior technology, was significantly correlated with Schirmer scoring, and the LBUT scoring was significantly correlated with tear break-up time (TBUT) scoring.8
To measure a patient’s tear osmolarity, clinicians now have two options: the Tearlab osmometer and the I-Pen (I-Med Pharma) osmometer. However, they should be careful to avoid using the readings interchangeably. Researchers from Ludwig Maximilians University in Munich have found that the I-Pen provides significantly higher osmolarity results compared with the Tearlab device. The team studied 51 healthy subjects—none of whom had clinically evident dry eye—with each device. They speculate that the location of the testing—tear meniscus vs. the palpebral conjunctiva—could account for the difference.9
If clinicians use Tearlab’s cut-off value of 308mOsm/l for normal osmolarity, 98% of the study participants would be considered normal, compared with only 68% when testing with the I-Pen. Thus, the researchers conclude that doctors should consider using a higher cut-off value (between 316mOsm/L and 320mOsm/L) when testing patients with the I-Pen.9
To help optometrists and ocular surgeons better anticipate iatrogenic dry eye in their patients, Italian researchers built a new clinical tool, the Ocular Surface Frailty Index (OSFI). The noninvasive, low-tech procedure can help predict postoperative DED, allowing surgeons and comanaging optometrists to perform useful personalized preoperative risk assessments. This new method includes 20 clinical factors to assess preoperatively that help to uncover any health deficits relevant to dry eye.10
Researchers identified three distinct categories: mild frailty (OSFI ranging from 0 to 161), moderate frailty (162 to 322) and severe frailty (more than 323). Of the total study participants, 16.2% developed DED within one month after surgery, and the rate significantly increased from 10.2% to 38.1% from the lowest to the highest frailty category. They also discovered that OSFI (but not age and gender) was significantly associated with postoperative DED onset.10
“This is a great example of precision medicine delivered in a personalized fashion by providing a frailty risk assessment to predict the likelihood of adverse conditions occurring after a surgical procedure,” says Dr. Shovlin.
A new approach to identifying DED measures the physical properties of the tear film, particularly the effective extensional viscosity, which researchers measured using acoustic rheometry. The Melbourne-based team found this metric is compromised in DED. In addition, a lower effective extensional viscosity is associated with more severe DED, and a moderate positive correlation existed between effective tear film extensional viscosity and noninvasive TBUT. The authors believe their results support the utility of tear effective extensional viscosity as a novel test for diagnosing DED in clinical practice.11
“Other fields in healthcare have used rheometry, and this technology may be employed someday as a device marker for identifying DED and stratifying it by severity,” notes Dr. Shovlin.
A long-term, high-fat diet may reduce the lacrimal gland’s tear secretion ability, which in turn could cause dry eye, a new study claims. The investigation included mice that were given either a standard or high-fat diet for different durations over one to four months. After one month, the study found mice on the high-fat diet had decreased tear secretion.12
This type of diet could induce lipid peroxidation, inflammatory cell infiltration, mitochondria damage, an increase in cell apoptosis and proliferation inhibition in the lacrimal gland. This could result in aqueous tear secretion decrease, which may induce dry eye, the researchers said.12
“Inflammation and associated structural morbidity has been shown to be evident in many DED studies, including this one, and continues to drive home the point that inflammation is both the cause and effect of DED,” explains Dr. Shovlin. “Diet influences many aspects of health, including influences in biomarkers in even more morbid diseases.”
 |
| Patients who wear sclerals for keratoconus had a lower risk of requiring keratoplasty. Photo: Christine Sindt, OD |
Contact Lenses
Researchers from the Brien Holden Vision Institute presented new findings that suggest a patient’s comfort in contact lenses affects their visual satisfaction—and vice-versa. For non-presbyopic patients wearing single vision lenses, changes in vision satisfaction affected their comfort rating, but changes in comfort didn’t necessarily impact their vision ratings. The opposite seems to be true for those wearing multifocal designs. Changes in their ocular comfort during lens wear led to changes in their vision rating more than vision changes impacted their comfort ratings.13
“Consideration of participant characteristics, visual stimulus and contact lens comfort needs to be accounted for when assessing overall contact lens experience,” explains Dr. Shovlin. “Probably not too unexpected, ocular comfort is of greater significance in non-presbyopic lens wearers, while vision satisfaction is of greater significance in the presbyopic group.”
University of Pittsburgh researchers developed a cytokine coating for silicone hydrogel lenses they believe could provide a sustained treatment for dry eye. Interleukin-4 (IL-4) has been shown to polarize macrophages from the inflammatory M1 phenotype—which is prevalent in DED—to the anti-inflammatory M2 phenotype. IL-4 can be incorporated into a nanometer-thick coating to mitigate the foreign body reaction to implantable polypropylene mesh, but the application to other devices has not yet been established, the study observes.14
The study found a uniform and conformal blue stain remained on lenses dipped in oppositely charged polymers (compared with control lenses), which shows successful application of the polymeric coating to the lens, investigators said. Additionally, IL-4 release kinetics from a coated lens incubated with enzymes showed a sustained release of IL-4 over several days, the researchers noted. There was little release of IL-4 from a coated lens in the absence of enzymes, indicating the coating was degraded primarily by enzymatic means, the study noted. “Our results support the hypothesis that our polymeric IL-4 releasing coating can be applied to contact lenses with a resulting sustained release of drug over days vs. the transient burst release seen with eye drops,” the investigators wrote in their abstract.14
Tech Advancements
Treatments for corneal blindness are limited by a high rate of complications and may not be as effective in cases of severe ocular surface damage. With this in mind, researchers invented an intraocular implant that projects light directly onto the retina, bypassing the damaged cornea—an alternative approach for treating corneal opacity. The device captures light via an external camera and then wirelessly sends data to an intraocular microdisplay.15
They found that the intraocular projector can restore vision in people blinded by corneal opacity, possibly providing a more accessible solution to those who may not be ideal candidates for cornea transplantation or keratoprosthesis. The researchers successfully constructed four functioning implants (9.5mm x 7mm x 7mm). With a lens placed 4mm from the microdisplay (focal length of 3mm), they found that the devices produced a visual acuity of up to 20/127.15
“This device appears to provide high levels of functional vision with few complications and should be a viable alternative for patients who are at high risk for failure with currently available surgical options,” Dr. Shovlin says.
This remarkable body of research continues to broaden horizons for practitioners and provide useful knowledge beneficial for the patients under their care. This is just a sampling of the findings presented at ARVO—the conference boasted so much more worth exploring. Check out ARVO’s full listing of abstracts to see for yourself the other latest advances in disease pathophysiology, diagnosis and management.
1. Sahebjada S, Chan E, McGuinness M, et al. Assessment of clinical parameters by ethnicity in patients with keratoconus: a multi-country study. ARVO 2019. Abstract 321. 2. Ling JJ, Mian S, Stein JD, et al. Impact of scleral contact lens use on risk of requiring corneal transplantation for keratoconus. ARVO 2019. Abstract 4779. 3. Kato N, Negishi K, Sakai C, et al. Five year outcomes of corneal collagen crosslinking: accelerated crosslinking induces less corneal haze and less continuous corneal flattening compared to conventional crosslinking. ARVO 2019. Abstract 313. 4. Mendoza-Garcia DLT, Del Valle CP, Robles-Contreras A, et al. Corneal crosslinking effects on tear inflammatory mediators in patients with keratoconus. ARVO 2019. Abstract 336. 5. Seifert F, Seufert F, Hommes D, et al. Ten year results after corneal collagen crosslinking with riboflavin and UV-A irradiation (CXL) for keratoconus—when to repeat CXL? ARVO 2019. Abstract 339. 6. Safi S, Jafarinasab M, Feizi S, et al. A new topographic “quad signs” for diagnosis and grading of pellucid marginal degeneration. ARVO 2019. Abstract 2104. 7. King-Smith P, Mauger T, Begley C, Tankam P. Does the peripheral light focusing effect explain the strong nasal location preference of pterygia? ARVO 2019. Abstract 4701. 8. Gefen R, Segev F, Geffen N, et al. A new hyperspectral imaging method to evaluate dry eye disease—3D-WLT study results. ARVO 2019. Abstract 6780. 9. Messmer EM, Schaumberger MM, Proglinger S, Koenig SF. Evaluation of tear film osmolarity using Tearlab and I-Pen osmometry. ARVO 2019. Abstract 6773. 10. Villani E, Marelli L, Lucentini S, et al. The Ocular Surface Frailty Index as a predictor of dry eye onset after cataract surgery. ARVO 2019. Abstract 6776. 11. Downie LE, Lee J-H, Makrai E, et al. A novel approach to identifying dry eye disease using acoustically-driven microfluidic extensional rheometry. ARVO 2019. Abstract 4189. 12. He X, Zhao Z, Bu J, et al. High fat diet induced functional and pathological changes in lacrimal gland. ARVO 2019. Abstract 1416. 13. Diec J, Naduvilath TJ, Tilia D, Bakaraju RC. The relationship between vision and comfort in contact lens wear. ARVO 2019. Abstract 6366. 14. Jhanji V, Nolfi A, Kulkarni M, et al. Polyelectrolyte multilayer coating for delivery of IL-4 from contact lenses for dry eye disease. ARVO 2019. Abstract 262. 15. Fan V, Rosenblatt M, Sun M, et al. Intraocular microdisplay projection system for treating corneal blindness. ARVO 2019. Abstract 4697. |


