 Contrary to what patients report in the exam room, a recent survey shows more than 50% of current contact lens wearers complain of contact lens dryness.1,2 Since more than half of our current contact lens wearers will likely drop out of lens wear over comfort issues, it is important to increase patient communication to pinpoint problems early.1
Contrary to what patients report in the exam room, a recent survey shows more than 50% of current contact lens wearers complain of contact lens dryness.1,2 Since more than half of our current contact lens wearers will likely drop out of lens wear over comfort issues, it is important to increase patient communication to pinpoint problems early.1
Learning the Symptoms
In order to truly understand the wearing experience, it is critical to appear non-threatening when addressing patients. If patients feel defensive while being questioned, they may hide their symptoms in fear that their prescribing eye care provider will tell them to discontinue lens wear. Consider the following dialogue: “I know that, at times, contact lenses are not as comfortable as we would like. We are fortunate that most contact lens wearers—even those with initial symptoms of discomfort—can now consistently wear lenses with little to no lens awareness. How would you describe your wearing experience? Is there anything that you would like improved upon?”
When patients feel at ease with their eye care practitioner, they are more likely to discuss their symptoms. Additionally, a dry eye questionnaire may, at times, reveal comfort issues that patients may be experiencing. One of the most widely utilized questionnaires is the Ocular Surface Disease Index, available at
http://www.dryeyezone.com/documents/osdi.pdf.
In order to maximize comfort, we have a variety of contact lens materials, designs and care systems available, each aimed at improving the patients’ experience. For many, optimizing these controllable factors will improve comfort.
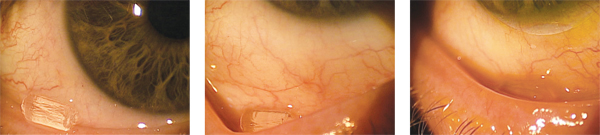
1. An incorrectly positioned Lacrisert resting on a patients lower eyelid margin.
2. A view of a Lacrisert in
the lower fornix of a patient that is properly positioned.
3. A
Lacrisert in the lower fornix of a rigid GP wearer that is properly
positioned.
Treat the Underlying Disease
In addition to optimizing the lens and care system properties, it is just as important to manage any underlying ocular surface disease. Dry eye disease, in particular, can quickly decrease the wearing experience.
By using vital dyes, we can get critical insights into the health of the ocular surface. Fluorescein dye viewed with a cobalt blue light and a yellow barrier filter allows us to accurately assess the presence of corneal and conjunctival staining, lid wiper epitheliopathy and tear film break-up time (TFBUT). A normal TFBUT is usually greater than eight seconds; lower TFBUT can indicate a potentially compromised tear film.3 Lissamine green dye stains dead or devitalized cells on the cornea and conjunctiva, when viewed with traditional slit lamp beam. A number of factors can cause staining with vital dyes in a contact lens wearer: the presence of staining is usually greater on the inferior cornea with either dye and on the nasal conjunctiva with lissamine green, which is often associated with dry eye.4-6
A dry eye patient is initially treated with a number of environmental modifications, starting with artificial tears or contact lens rewetting drops for lens wearers.7 For those using drops greater than four times a day, preservative-free drops will likely work best. For those patients who experience symptomatic relief with artificial tears and do not want to use multiple drops a day, a lacrimal insert may be an ideal solution.
Lacrisert (hydroxypropyl cellulose ophthalmic insert, Aton Pharma) is a lacrimal insert made of hydroxypropyl cellulose. It is 3.5mm in length and placed in the lower fornix once a day by a small applicator. The insert supplements the patients tear film with a robust lubricant as it dissolves over a 24-hour period. Approximately 9% of patients will experience blurry vision.8 For patients who benefit from the ocular comfort but experience blurring, we suggest using Lacrisert in the evening and removing the inserts in the morning.
Lacrisert and Contact Lenses
We have a number of advances in contact lens materials and designs, as well as contact lens care systems, to enhance the wearing experience. Surfactants in today’s multipurpose disinfecting solutions can retain moisture on the surface of contact lenses and promote all day comfort.
Unfortunately, there are a number of patients who cannot wear traditional modality contact lenses. These patients often experience excellent visual acuity with their contacts, but may suffer some discomfort. When vision is good but comfort is sub-optimal and specialty lenses are needed, optimizing the ocular surface and tear film is necessary. For such patients and those who temporarily benefit from rewetting drops or artificial tears, a lacrimal insert may be optimal.
In a recent study, contact lens patients with dry eye using Lacrisert experienced improved comfort after one month of use.8 It is important that Lacrisert patients place the contact lens on the eye first and then place the insert in the lower fornix. If this order is reversed, the insert may fall out when contact lens are placed on the eye.
A Case in Point
“Wendy” is a 44-year-old female who had phototherapeutic keratectomy (PTK) for Salzmann’s nodular degeneration 10 years ago. She presented with poor visual acuity in her left eye—the same eye that was previously treated. Her best-corrected visual acuity measured 20/60 O.S. with +1.00 -4.50 x 140 manifest refraction. Slit lamp examination was remarkable for stromal scarring in the superior nasal quadrant of the left cornea, consistent with the location of her previous PTK. Based on symptoms and slightly reduced tear film break up time, Wendy was diagnosed with mild dry eyes.
The amount of corneal astigmatism made it difficult for her to wear glasses with the manifest refraction. Additionally, the best-corrected visual acuity with that level of correction was 20/60 O.S., significantly less than her other eye which was best corrected to 20/20. Her ophthalmologist referred her to our office for a contact lens fitting.
In the past, she has tried rigid gas-permeable contact lenses and remembers seeing well with the lens, but that the lenses were too uncomfortable to wear. She wanted to explore new contact lens options that may provide her with good visual acuity and comfort.
We fit her left eye with a SynergEyes A hybrid lens with a -3.00D/7.4/8.4. Wendy did relatively well with this contact lens, and her visual acuity measured 20/20 O.S. She said the SynergEyes A lens was significantly more comfortable than the past GP she had tried. Although the hybrid lens was relatively successful, she still needed artificial tears multiple times a day to provide additional comfort.
We placed a Lacrisert in the lower fornix of her left eye. Wendy called back the next day and said that her eye felt significantly more comfortable. We trained Wendy on how to insert the Lacrisert, and she was given a prescription to use them daily. Currently, she wears a hybrid lens successfully and comfortably in her left eye.
It is important to prioritize patient comfort in lens wear; start by maintaining open communication with your patients. When you know the true symptoms—from dry eye to blurry vision—you can work to find a better long-term solution.
1. Young G, Veys J, Pritchard N, Coleman S. A multi-centre study of lapsed contact lens wearers. Ophthalmic Physiol Opt. 2002 Nov;22(6):516-27.
2. Nichols JJ, Ziegler C, Mitchell GL, Nichols KK. Self-reported dry eye disease across refractive modalities. Invest Ophthalmol Vis Sci. 2005 Jun;46(6):1911-4.
3. Moore JE, Graham JE, Goodall EA, et al. Concordance between common dry eye diagnostic tests. Br J Ophthalmol. 2009 Jan;93(1):66-72. [Epub 2008 Sep 9]
4. Andrasko G, Ryen K. Corneal staining and comfort observed with traditional and silicone hydrogel lenses and multipurpose solution combinations. Optometry. 2008, Aug; 79(8):444-54.
5. Jones L, MacDougall N, Sorbara LG. Asymptomatic Corneal Staining with the use of balafilcon silicone-hydrogel contact lenses disinfected with polyaminopropyl biguanide-preserved care regimen. Optom Vis Sci. 2002 Dec;79(12):753-61.
6. Catania LJ. Primary Care of the Anterior Segment. 2nd ed. East Norwalk: Appleton & Lange; 1995:222-6.
7. Behrens A, Doyle JJ, Stern L, et al. Dysfunctional tear syndrome: a Delphi approach to treatment recommendations. Cornea. 2006 Sep;25(8):900-7.
8. Luchs JI, Nelinson DS, Macy JI. Efficacy of hydroxypropyl cellulose ophthalmic inserts (LACRISERT) in subsets of patients with dry eye syndrome: findings from a patient registry. Cornea. 2010 Sep. [Epub ahead of print]


