With more than 30 million American consumers, the versatility of today’s contact lenses has made it an appealing choice for those with the busiest of lifestyles.1 Refractive correction, in this form, can offer cosmetically pleasing results while addressing corneal abnormalities or other pathological conditions and, in many cases, improve basic daily life functions. As optometric physicians, it is our responsibility to ensure that our contact lens wearing patients maintain a healthy and safe care regimen. We do this by evaluating the health, comfort, vision, movement, staining patterns and position of the lenses on our patients prior to writing a prescription. Simultaneously, we empower our patients by reviewing safety practices and explaining the risks of improper lens use. By maintaining open communication with the patient, we can reduce the risk of infection and optimize the lens wearing experience.1,2
Schedule Annual Eye Exams
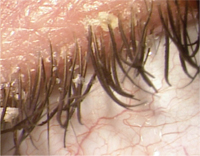
1. Unhygenic practices can lead to a build up eylid debris.
The first step is to determine whether the patient is a good candidate for contact lenses. So, a good starting point is to review your patient’s history. By discussing the systemic, medical and ocular history, you can determine whether your patient’s lifestyle is suited for daily contact lens wear. Red flags in your patient’s history include diabetes, thyroid problems, immune suppression, lid and dermatologic conditions, pregnancy, medications with potential ocular side effects, allergies, dry eyes, active anterior segment disease or prior eye injuries.3
Open communication is vital to properly match the right lens to your patient’s individual needs. Start by asking your patient to discuss his motivation for visiting you and his expectations for long-term contact lens wear. By understanding your patient’s needs and setting mutual realistic expectations, you are taking the extra step to encourage lens compliance and reduce risks of dropouts. Similarly, if your patient currently wears contact lenses, take the time to learn about his experience with a particular brand, his daily lens routine and what additional products he uses as part of his daily cleaning regime. Armed with this information, as practitioners, we are able to prescribe the best match—whether it be daily or extended wear lenses, gas permeable or hydrogel lenses, or a better customized lens.
Take the Time to Educate the Patient

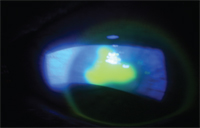
2. Contact lens non-compliance can result in red eye.
Once we select a lens that provides an optimized fit, we must take the time to educate our patients on the type and brand of lens that they are wearing, the recommended wearing schedule for these particular lenses and how to dispose of the lens at the correct time interval.
Patient education is paramount in maximizing the health and safety of the contact lens wearer. When addressing first-time lens wearers, start by reviewing how to properly use the lenses. I suggest offering patients the opportunity to view an in-office interactive video and following the introduction with a detailed handout they can take home with them after the visit.4,5 During your appointment, focus on teaching your patient the proper techniques for the placement and removal of the lenses—as specific to either soft, gas permeable or hybrid lenses.
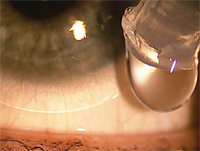
This quick tutorial is absolutely necessary to get the patient on the right track and prevent him from potential complications, such as epithelial erosions and abrasions. For the new contact lens wearer, share some instructions on initial lens awareness or increased lens movement—which may make them feel temporarily uncomfortable. If the patient is young, educate the parents on how to encourage good habits like washing hands before touching lenses and taking out lenses before swimming or showering. By taking the extra time to talk to the parent/guardian, you have established another layer of protective lens handling. Patient education is a key component to successful long-term care of contact lenses and serves as an integral part of lens disinfection and overall compliance.
Encourage Proper Hygiene
3. Avoid corneal abrasions by educating your patients on contact lens safety.
Proper hygiene can minimize ocular complications or infection. Remember to address these three key recommendations for proper hygiene during the appointment.
• Wash your hands. Patients should be advised to always wash their hands before insertion and removal. It is important to remind patients that cleansing soaps should not contain lanolin, creams or oils, as these substances can transfer to the lenses.
• Clean the storage case. Reiterate and emphasize the importance of a clean contact lens storage case. Patients should replace their case at least every three months to prevent significant buildup of biofilm—it can coat the inner surfaces of the case and serve as a breeding ground for bacteria and other microorganisms. Weekly cleaning of the lens case with hot water and air-drying can also help in reducing contamination.
To reduce case contamination, a silver-impregnated lens case was developed and studies show that it measures a statistically significant lower proportion of bacterial contamination than control cases.6 This new alternative is a good option for patients, especially those lens wearers with recurrent inflammations or infections. Tips of solution bottles also serve as a contamination area, particularly if the cap is left open or if the tip is touched by another surface.
Instruct your patients to be proactive in cleaning their cases, ask them to remember to close the caps to their solution bottles and inform them that contamination increases the risk of eye infections.5
• Avoid topping off solution. Contact lens wearers should not “top off” the case, but rather dispose of used solution daily and clean cases or replace them as instructed. Despite the efficacy of current lens disinfectants, lens case contamination is a well-documented occurrence for contact lens wearers. Certain microorganisms have a propensity to attach to lens surfaces and may become more resistant to disinfection upon attachment. Non-compliance with disinfection regimens occasionally occurs in situations when patients store their lenses in saline or in tap water.
Discuss the Importance of Compliance
4. Patients need to be taught how to instill drops without touching the tip of the bottle to their eyes.
A more informed and content patient will likely be more compliant. To ensure a safe fit, offer the patient a pair of diagnostic trial lenses to be tested immediately prior to the next follow-up visit. This trial period allows the patient to assess the comfort of the lenses over the course of several days and up to a week. Any issues or complaints can be addressed at the appointment before a year supply of the lenses is purchased. This also allows the optometrist to look for any staining, hypoxia or other factors—indications that the lens might not be the optimum long-term wear fit. This trial period goes a long way to enhance patient satisfaction, boost confidence and ultimately, retain patient loyalty—which translates to increased revenue for the practice.
Non-compliance—including failure to adhere to prescribed wearing schedules; forgetting to replace the solution on a routine basis or substituting solution with saliva or tap water; lack of hygiene when handling, caring for or cleaning lenses; or substituting prescribed brand lenses for cheaper alternates—can lead to further costs and expenses for the patient.5 Explain to your patient how non-compliance can result in compromised eye health including contact lens papillary conjunctivitis, infiltrative keratitis, microbial keratitis, contact lens acute red eye, corneal erosion or contact lens peripheral ulcer1,2 (see figure 5). Upon slit lamp examination, practitioners may also notice vascularization or stromal folds.11 Corneal infiltrates can present in contact lens wearers as a result of lens overwear, poor lens care or toxic solutions. These patients will often present with chief complaints of discomfort, irritation, redness, watering and photophobia.
Review Proper Lens Care Protocol
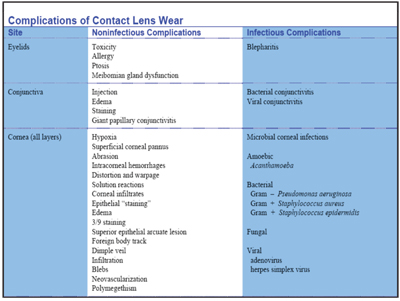
5. The American Optometric Association details contact lens wear complications.7
With so many different contact lens solutions—from multi-purpose cleaners to cleaning/conditioning kits—on the market today, patients question which solution is best to use with their contact lenses. To that end, the Andrasko Corneal Staining Grid offers a reference guide for practitioners by providing a biocompatibility chart of different soft contact lenses paired with differing care systems.8
Today, soft-lens solutions offer a convenient, no-rub, all-in-one, multi-purpose option; however, the label is misleading. Although it reads “no rub,” patients should still be instructed to gently rub the contact lens in the palm of their hand with fresh solution prior to disinfection.9 By doing so, they greatly reduce the bacterial load that accumulates on lens surfaces and enable the disinfection system to work more efficiently. For gas-permeable care kits on the market, we should advise our patients to use both a surfactant cleaner and conditioning solutions—especially if we notice a build-up on the patient’s lenses from improper cleaning. If noticed, practitioners need to address the underlying issue and rule out protein deposits, allergies, dry eye and irritation.
When patients are prescribed rewetting solutions in conjunction with contact lenses, they must be cautioned to avoid contamination and instructed on how to properly instill the drops without touching the tip of the bottle to their eyes. Several marketed rewetting agents offer the patient increased comfort while minimizing complaints of dryness. However, patients should understand that these drops are not substitutes for cleaning solution and, in particular, taught which drops are compatible with their lenses.
Hydrogen peroxide systems are recommended for patients with sensitivity to preservatives in multi-purpose solutions. When using peroxide systems, lenses must be neutralized before use to avoid pronounced stinging and likely corneal staining.3 A peroxide burn from improper use of solution creates a painful, although not sight-threatening, situation.
Products for in-office disinfection and storage of trial contact lenses are intended to reduce the risk of microbial contamination introduced during patient-to-patient use. Due to the increased potential for cross contamination between patients in the office, internal regimens should be made a top consideration and should adhere to ANSI standards.10
Whether it is a returning patient eye exam or a new patient contact lens fitting, we must commit ourselves to meeting the guidelines specified in the AOA’s Optometric Clinical Practice Guideline: Care of the Contact Lens Patient.11 When we use our expertise to educate our patients on hygiene, compliance, lens disinfection and safety, we empower them to become healthy lifetime contact lens wearers.
Jamie C. Wohlhagen is a third year student at the Pennsylvania College of Optometry at Salus University, where she serves as the president of the Class of 2012, the PCO liaison for the National Board of Examiners in Optometry and the administrative assistant to the contact lens department. She hopes to complete a residency in cornea and contact lenses.
1. Contact Lens Institute. Facts and Stats. American Optometric Association. 2003 May. Available at: www.aoa.org/x5231.xml (Accessed October 2010).
2. Focusing on Contact Lens Safety. FDA. 2008 Nov. Available at: www.fda.gov/ForConsumers/ConsumerUpdates/ucm048893.htm (Accessed October 2010).
3. White G. Caring for Soft Contact Lenses. Access Media Group. 2010 Mar. Available at: www.allaboutvision.com/contacts/caresoftlens.htm (Accessed October 2010).
4. Eyemaginations. Animation Comparison. Available at: www.eyemaginations.com/sub.php?navigation_id=782&nav_solution_id=1 (Accessed October 2010).
5. Bennett E, Henry V. Clinical Manual of Contact Lenses. 3rd ed. Philadelphia: Lippincott Williams and Wilkins; 2009:157,281-3.
6. Amos C, George M. Clinical and laboratory testing of a silver-impregnated lens case. Contact Lens and Anterior Eye. 2006 Dec;29(5):247-55.
7. Care of the Contact Lens patient – A quick reference guide. American Optometric Association. Available at: www.aoa.org/documents/QRG-19.pdf (Accessed October 2010).
8. Andrasko G. Andrasko Corneal Staining Grid. The Staining Grid Center. 2006-2009. Available at: www.staininggrid.com (Accessed October 2010).
9. Gasson, A, Morris J. The Contact Lens Manual: a practical guide to fitting. Vol. 1. Butterworth-Heinemann. 2003:341.
10. Benjamin W, Donshik P, Miller M, et al. Proposed ANSI Standards for In-office Disinfection of Contact Lenses. American Optometric Association. Available at: www.aoa.org/x6138.xml (Accessed October 2010).
11. Optometric Clinical Practice Guideline: Care of the Contact Lens Patient. American Optometric Association. 2000. Available at: www.aoa.org/documents/CPG-19.pdf (Accessed October 2010).


