There are many reasons scleral lenses have taken over such a large share of the contact lens market in such a short period of time. These devices offer a life-changing experience by bringing visual improvement and comfort to many patients while avoiding common issues associated with other contact lens modalities. Basic fitting techniques for scleral lenses can be implemented without much difficulty, but advanced troubleshooting takes time and effort to master. This article outlines mistakes and complications that commonly arise from scleral lens fittings and ways scleral lens fitters can navigate them to improve outcomes.
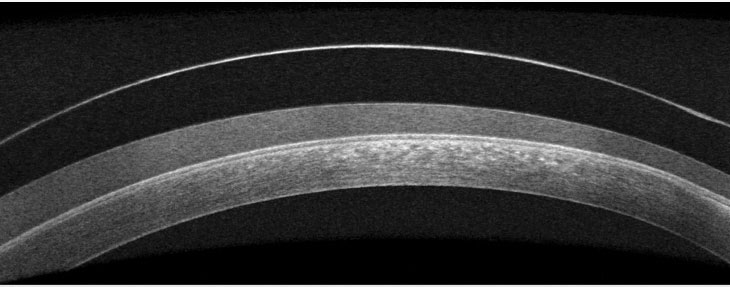 |
| Fig. 1. OCT imaging shows fogging under a scleral lens. Click image to enlarge. |
Unqualified Patients
The importance of carefully choosing appropriate candidates for scleral lenses cannot be overstated, as patient motivation is critical for success. Due to the custom nature of these lenses, patients must understand that more specialized care and several office visits to finalize an optimal fit may be necessary. Diagnostic fittings serve as an opportunity for patients to preview the vision and comfort of the lenses, which helps determine their level of motivation.
Indications for scleral lens wear fall under two main categories: irregular corneal shape and ocular surface disease. The rigid optics of scleral lenses provide clear vision to patients with keratoconus, corneal scarring and other causes of corneal irregularity, while the post-lens tear film continuously lubricates the cornea to treat ocular surface disease.1
Many practitioners now fit scleral lenses on normal corneas due to the optics and comfort they offer. However, it’s important to consider the risks that may be associated with long-term scleral lens wear, especially in eyes that do not require the lenses for vision correction and may be associated with a higher risk-benefit ratio.2-4 Patients with normal, healthy corneas may have less of an incentive to work through complications or setbacks with scleral lenses if other easier, more convenient options also provide clear vision.
Inadequate Education
If a patient is deemed an appropriate candidate for scleral lens wear and is motivated to move forward with the process, it is then the provider’s responsibility to educate them on the expectations and the commitment level involved with lens fitting, wear and care. Fees and insurance reimbursement rates should also be topics of conversation. Having a well-trained staff and detailed protocols makes these discussions simple, efficient and beneficial. Investing time upfront can improve patient outcomes and satisfaction in the long run. It is important that patients first view scleral lenses as unique medical devices distinct from standard soft lenses so that they are fully prepared for what they are signing up for.
 |
| Fig. 2. This lens has poor wettability and a buildup of material on its front surface. Click image to enlarge. |
Fitting Complications
Once a patient is sufficiently educated and has realistic expectations on what is to come, they are then ready to be fit with scleral lenses. The “perfect fit” of a scleral lens involves complete vaulting over the cornea and limbus without excessive clearance and a smooth landing on the sclera.
The ideal amount of central clearance is up for debate but is generally around 200μm to 300μm.5 Highly irregular corneas may have lower or higher amounts of clearance. Corneal touch as a result of inadequate clearance often presents after lens removal as an area of epithelial staining. If this occurs, central clearance can be increased in large steps by increasing the sagittal depth of the lens and in smaller steps by steepening the peripheral curves.
Lens touch at the limbus can be addressed by increasing the diameter of the landing zone or steepening the curve overlying the limbus. Limbal bearing should be minimized as much as possible to avoid damage to the stem cells, although some amount of superior touch may be unavoidable.6 Excess limbal clearance, on the other hand, can induce hypoxia to the area and increase the chance of conjunctival prolapse—when loose conjunctival tissue is pulled anteriorly under the lens and onto the cornea.7
Superior limbal touch is difficult to avoid due to the tendency for scleral lenses to decenter inferiorly and temporally. This is likely related to the elevation of the nasal sclera relative to the temporal sclera as well as gravity and downward force from the upper eyelid.8 Using a smaller lens diameter to decrease weight or toric peripheral curves can often improve lens centration.
Fitting concerns at the edge of the lens usually cause discomfort to the patient and can be addressed by customizing peripheral curves. Lab consultants can provide detailed information on how to best adjust each proprietary design.
Early on in the fitting process, epithelial bogging is sometimes described after lens removal as having a “water-logged” appearance. If lens parameters are appropriate and not causing excessive hypoxia, this complication often resolves on its own after a few weeks of lens wear.1
Handling Challenges
After the practitioner has successfully fit the scleral lens, the rest is up to the patient, and problems are bound to come up. Due to the large size of scleral lenses and the need for fluid to fill them, lens handling can pose a challenge, inconveniencing and frustrating many patients.
Some common aspects of lens care that patients struggle with are keeping both eyelids out of the way when applying the lenses, avoiding bubbles and overcoming Bell’s phenomenon, which causes the eye to close and rotate up and out. There are many devices that hold the lens in place to free both of the patient’s hands so that they’re able to manipulate their eyelids.
If patients struggle with bubbles under the lens, more viscous, preservative-free artificial tears can be used to fill the lens. The lens diameter can also be reduced to allow for easier application as long as adequate limbal clearance is maintained. Unfortunately, handling difficulties are only one of the many issues scleral lenses can cause, and patients need to know how to approach each of them.
 |
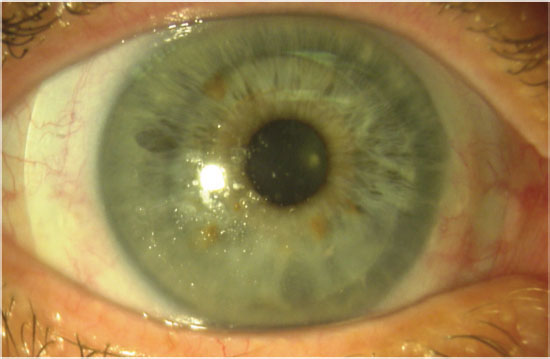
| Fig. 3. Fluorescein dye and bubbles can leak under an area of edge lift. Click image to enlarge. |
Mid-day Fogging
One of the most common complications of scleral lens wear, especially in patients with ocular surface disease or atopic disease, is lens fogging—or the buildup of particulate matter underneath or on the front of the lens (Figures 1 and 2).10 This can greatly inconvenience patients, as it causes a decline in vision throughout the day and often requires patients to remove, clean and reapply their lenses.9 The exact makeup of the lens debris is unknown but likely contains lipids and proteins from the tear film and white blood cells.11,12
To address lens fogging, it helps to first determine if the buildup is occurring on the post-lens tear film, the front surface or both. Post-lens tear film fogging can be minimized by adding a few drops of a viscous, preservative-free artificial tear to the saline in the lens bowl.
Options for treating the front surface of the lens include adding a hydrophilic lens coating, using an enzymatic- or alcohol-based cleaner (do not use either on coated lenses), using preservative-free artificial tears for lubrication and spot-cleaning the lens with a moistened cotton swab.
Adjusting the lens fit can also reduce fogging by improving lens alignment to reduce tear exchange. Toric peripheral curves are usually needed to achieve better alignment, while decreasing corneal clearance minimizes the thickness of the foggy tear film and, therefore, reduces symptoms. Treating meibomian gland disease and ocular allergies and switching to preservative-free cleaning systems can help with both types of lens fogging.1
Corneal Hypoxia
The risk of corneal hypoxia is greater with scleral lenses compared with other lens types for several reasons. Scleral lenses are relatively thick compared with corneal gas permeable lenses to maintain their shape and prevent flexure. Minimal tear exchange occurs under a scleral lens, and oxygen trying to reach the cornea must travel through the lens material and the post-lens tear film.13 The modifiable variables that affect oxygen transmissibility are the lens material’s oxygen permeability, lens thickness and corneal clearance of the lens.
Complications associated with hypoxia include corneal edema, epithelial microcysts and neovascularization. These signs of hypoxia are not common with scleral lens wear and are more likely to occur in patients with predisposing conditions that compromise endothelial function, such as corneal transplants.
Even without clinical evidence of hypoxia on slit lamp exam, low-grade corneal edema after scleral lens wear is measurable using optical coherence tomography (OCT). Therefore, it is important to use materials with high oxygen permeability, keep the clearance of the lens low while preventing corneal touch and avoid excessively thick lenses.14 Although materials high in oxygen permeability tend to have poor wettability, recent advances in lens coating technologies can keep these materials clean and comfortable.
Significant corneal neovascularization from scleral lens wear is rare and may be caused by contact lens over-wear or poor compliance, in addition to lens material and fitting variables. Discontinuation of lens wear along with medical therapy may be required to treat severe neovascularization. However, neovascularization that results from an underlying condition, such as Stevens-Johnson syndrome, may regress with scleral lens wear, so it is important to determine the underlying cause and initiate treatment accordingly on a case-by-case basis.1
If signs of corneal hypoxia appear in a scleral lens wearer, the first step is to adjust the lens parameters to maximize the oxygen transmissibility of the lens system. If this has been done already, it may be wise to consider other contact lenses, such as corneal gas permeable, specialty soft or hybrid lenses. In many cases, however, scleral lenses are the only option that provides comfortable, stable vision. For these patients, a reduced wearing schedule coupled with hypertonic saline drops may be a last resort.1
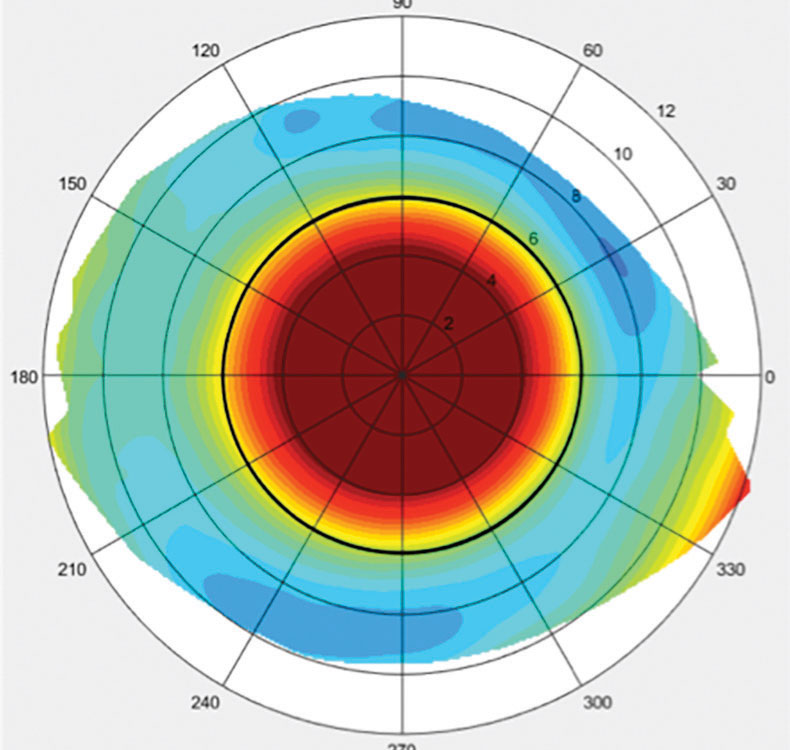 |
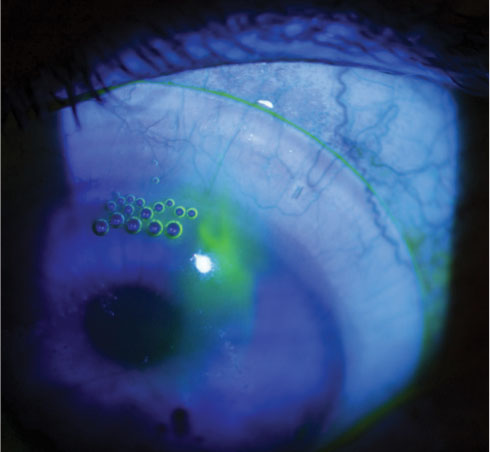
| Fig. 4. This topographical scleral map was taken of an eye with a toric sclera. Click image to enlarge. |
Ocular Irritation
Scleral lenses are often regarded as a comfortable contact lens option, but issues can arise that cause irritation to the ocular surface. Fit-related comfort problems usually occur when the edge of the lens does not align with the sclera. If the edge lifts off the eye, it will rub against the lid when the patient blinks. A solution to alleviate this concern is steepening the peripheral curves. Compression—when the lens lands too abruptly and causes blanching of the conjunctival vessels—is the opposite problem and can lead to redness and irritation after lens removal.1
Often, flattening the landing curves improves lens alignment in this situation, but the curves may need to be steepened if the compression occurs further from the lens edge. A careful slit lamp evaluation of the lens edge can usually detect these issues. Adding fluorescein dye to the anterior lens surface and watching where it flows under the lens can help pinpoint areas where the edge is not in contact with the eye (Figure 3).
Other tools for evaluating fit and optimizing lens alignment with the sclera include OCT and scleral mapping instruments (Figure 4). Toric peripheral curves can often help align the lens to the sclera, but sometimes even more customized peripheries are required.15 To alleviate pressure on a raised area of conjunctival tissue, such as a pinguecula or glaucoma-filtering bleb, many lens designs incorporate a localized vault of the lens edge. Use caution when fitting scleral lenses on eyes with filtering blebs due to the risk of bleb erosion.
Another possible source of discomfort is the lens solution. If punctate staining is noted, solution toxicity is the likely culprit and may indicate that the patient is using a preserved solution to fill the lens prior to application. To minimize solution-related irritation, first ensure patients are only using preservative-free saline to apply the lens, then consider switching to a preservative-free cleaning solution, such as a peroxide-based cleaner.
Blurred Vision
If visual acuity after over-refraction is worse than expected with a scleral lens, there are several possible causes that you can correct. First, check for poor wettability and lens fogging. Next, perform a careful spherocylindrical over-refraction to determine if a front toric lens is required to correct residual astigmatism. Corneal topography can help detect lens flexure, which can be reduced by better aligning the landing zone of the lens with the sclera or by increasing lens thickness.
Visual quality can sometimes be improved with oblate lens designs, as the flatter base curves usually result in lower-powered lenses and less overall distortion.16 If pinhole acuity is not achieved with over-refraction and all other causes of blurred vision have been ruled out, consider higher-order aberrations (HOAs) as a potential cause. Some lens designs have aspheric curves on the front surface to minimize these distortions. Custom-designed lenses that address HOAs may help improve visual quality for these patients but are not commercially available at this time.17
Resource Under-utilization
A major mistake that many new scleral lens fitters make is failing to take advantage of the array of resources available to learn advanced fitting techniques and navigate problems as they arise. Even seasoned fitters should pay attention to new lectures and articles, as scleral lens technology and research is rapidly advancing. Lab consultants are always available to help with difficult fits and are especially beneficial when using front toric lenses, multifocals, localized vaults of the lens edge and other custom options. Online platforms also provide access to opinions and tips, case reports and new information.
Scleral lenses are generally well-tolerated and have relatively low complication rates. However, when challenges arise, steps must be taken to optimize vision, especially if the lenses are a last resort before invasive treatment, such as corneal transplantation. Give your scleral lens patients the best care possible by staying up-to-date in this quickly changing field and taking advantage of the resources available to further enhance your skills.
Dr. Korszen practices in Spokane, WA, and is a fellow of the American Academy of Optometry and the Scleral Lens Education Society. She has a passion for specialty contact lens fitting and ocular surface disease management.
|
1. Barnett M, Johns LK. Ophthalmology: current and future developments (volume 4): contemporary scleral lenses theory and application. In: Sharjah, UAE: Bentham Science Publishers. 2. Michaud L. Beyond irregular: scleral lenses for everyday use. Cont Lens Spec. 2015;30:30-2, 34, 36. 3. Van der Worp E, Bornman D, Ferreira DL, et al. Modern scleral contact lenses: a review. Cont Lens Ant Eye. 2014;37(4):240-50. 4. Ensley R, Miller H. Sclerals: the new normal? RCCL. 2018;155(3):8-10. 5. Van der Worp E. A Guide to Scleral Lens Fitting, Version 2.0. Forest Grove, OR: Pacific University; 2015. 6. Pucker AD, Laurent JM. Scleral contact lens complications. Cont Lens Spec. 2017;32:24-7. 7. Caroline PJ, André MP. A potential effect of conjunctival prolapse. Cont Lens Spec. 2013;28(9):56. 8. Ritzmann M, Caroline PJ, Börret R, et al. An analysis of anterior scleral shape and its role in the design and fitting of scleral contact lenses. Cont Lens Ant Eye. 2018;41(2):205-13. 9. McKinney A, Miller W, Leach N, et al. The cause of midday visual fogging in scleral gas permeable lens wearers. Invest Ophthalmol Vis Sci. 2013;54(15):5483. 10. Sindt CW, Longmuir RA. Contact lens strategies for the patient with dry eye. Ocul Surf. 2007;5(4):294-307. 11. Walker MK, Bergmanson JP, Miller WL, et al. Complications and fitting challenges associated with scleral contact lenses: a review. Cont Lens Ant Eye. 2016;39(2):88-96. 12. Postnikoff CK, Pucker AD, Laurent J, et al. Identification of leukocytes associated with midday fogging in the post-lens tear film of scleral contact lens wearers. Invest Ophthalmol Vis Sci. 2019;60(1):226-33. 13. Morrison S, Walker M, Caroline P, et al. Tear exchange beneath scleral lenses. Poster presented at: The 2014 Global Specialty Lens Symposium; 2014 Jan; Las Vegas, NV. 14. Compañ V, Aguilella-Arzo M, Edrington TB, et al. Modeling corneal oxygen with scleral gas permeable lens wear. Optom Vis Sci. 2016;93(11):1339-48. 15. Visser ES, Visser R, Van Lier HJ. Advantages of toric scleral lenses. Optom Vis Sci. 2006;83(4):233-6. 16. Shovlin JP. Scleral battle: oblate vs. prolate. Rev Optom. 2018;155(3):78. 17. Yoon G, Sabesan R, Johns L, et al. Custom correction of higher order aberration in keratoconus with a scleral lens prosthetic device. Invest Ophthalmol Vis Sci. 2012;53(14):1394. |