Orthokeratology’s (ortho-K) resurgence in popularity is a testament to extensive research efforts, lens design advancements and our growing understanding of the corneal shape and topography. As a specialty that was pioneered and refined by optometrists, clinicians should embrace the technology and continue to learn how current advances better serve our patients.
This article will discuss some dos and don’ts for those interested in using ortho-K in their practice before reviewing several case examples.
 |
|
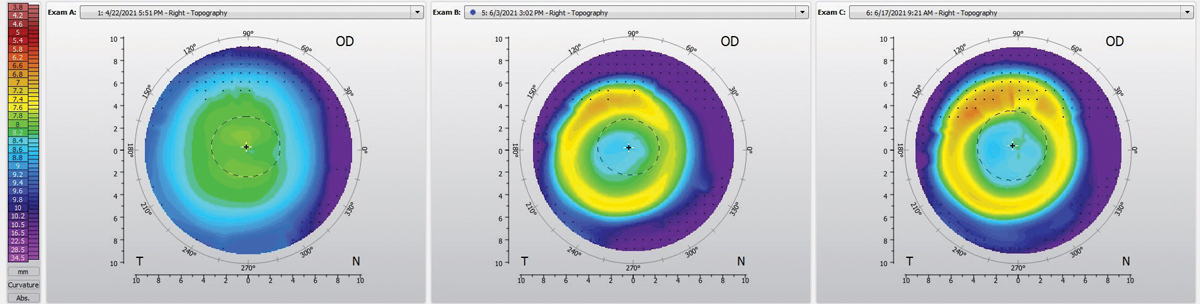
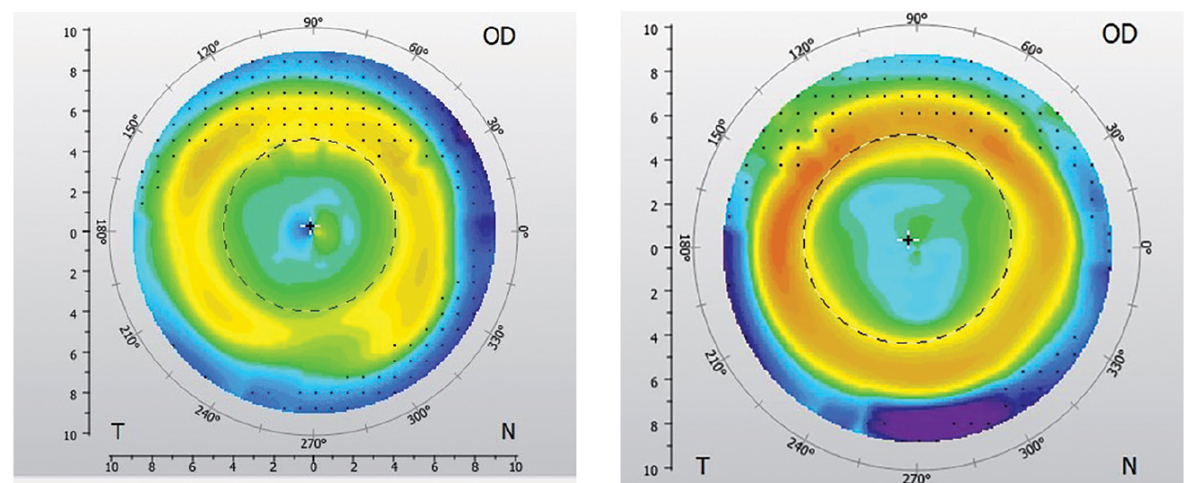
Fig. 1. Pre-ortho-K OD topography (left), post-ortho-K at one-day follow-up (middle) and post-ortho-K at two-week follow-up (right). Click image to enlarge. |
The Principles
Different brands may have different numbers of curves and the curves may have unique names, but the principle is the same. The ortho-K effect is achieved through central corneal epithelial thinning and mid-peripheral stromal and epithelial redistribution.1
Since the cornea determines 60% of the eye’s focusing power, minor changes in the superficial epithelial cells thickness can change the refractive error. For example, 6µm of corneal flattening can result in 1.00D of reduced myopia correction.2 The onset is observable after one night of wear, and the gradual stability is achieved after one to two weeks of wear time.3
The older the individual and the higher the refractive error, the longer the treatment takes to achieve stability. Advanced technology has led to ortho-K lenses that can correct hyperopia and presbyopia, but its most common application is for myopia. The lenses create myopic peripheral defocus that can reduce axial elongation.
1. Do: learn as much as you can. Each ortho-K lens system has its own design and fitting philosophy. There are three ways to approach fitting this modality: empirically, trial-based or custom lens design with topography and software). Each has its own advantages and disadvantages:
- Empirical fitting consists of supplying the lens manufacturer with either keratometry readings or topographic (i.e., eccentricity, HVID) and refractive data to order the lens. Then the OD receives, evaluates and dispenses the lenses if the fit is appropriate. This fitting works great for patients that fall under the parameters.
- Pros: less chair time initially, zero financial investment to start.
- Brands that do this: Contex OK Lens, Vipok, Paragon CRT, iSee, Euclid Emerald.
- Trial fitting involves taking K readings, topographic and refractive information and using a nomogram to choose an initial diagnostic lens to try. The fit of the lens is evaluated using fluorescein, and an over-refraction is performed. The trial lens can be changed based on the fit to reach the best fit prior to ordering a lens. If it’s a new unopened diagnostic lens, you can even dispense it!
- Pros: a higher first fit success rate because the fit is validated in the exam room, sets patient expectation on comfort.
- Cons: chair time at first visit, the practitioner may be limited to available designs.
- Brands: Bausch and Lomb BE Retainer, Paragon CRT.
- Custom topography-based designs allow practitioners to import corneal topographies into a proprietary software, and then a customized lens is designed from the data. This can be a good learning opportunity for intermediate fitters to learn about the interdependence of all the modifiable curves.
- Pros: works well with minimal modifications if data input is accurate, practitioners get more control on design, less chair time.
- Cons: must have accurate topography data, may require a more advanced understanding of lens parameters and practitioner skill.
- Brands: Wave NightLens, Eyespace Forge Ortho-K, OrthoTools, J&J Acuvue Abiliti.
Start off by choosing one or two lens designs to learn in detail and familiarize yourself with the types of modifications that can be made. It may be easier for a novice to start with empirical fittings and move to more advanced design(s) when more comfortable.
2. Do: use the right tools. This is essential to fitting and troubleshooting patients.
The gold standard is topography. The axial map can monitor how much power was changed. The tangential map is useful for patient selection, understanding the type of astigmatism and evaluating treatment centration. Topography is also used for documenting the treatment course and allows for gathering comparative data and troubleshooting on the treatment effect.
Having good-quality topographies is vital for first fit success. Don’t hold back from capturing multiple topographies per eye pre-fit. Also note the consistency of topographic scans with the visual axis vs. the geometric axis.
Aim to capture as much corneal data as possible. If you can match your topography Ks to the autorefractor Ks, you get optimal accuracy.
Other tools worth mentioning include:
- Autorefractor.
- Slit lamp with cobalt blue light.
- Sodium fluorescein strips.
- Wratten filter.
- HVID ruler.
- Slit lamp camera/cell phone holder.
Tools to measure and verify rigid gas permeable (GP) lenses (radiuscope, band magnifier or a V-gauge to measure lens diameter).
3. Do: prepare a protocol. Implementing a new service requires a good workflow to accommodate it. Prepare informed consent forms, instruction sheets on lens care, FAQs and figure out who in your clinic will be reachable if concerns arise. Keep the following in mind:
- Set an appropriate amount of time in your schedule for fittings and follow-ups if you are just getting started. For beginners, this can be 30-to-40-minute slots—long enough to gather relevant data and review expectations.
- Visits should include a thorough history, visual acuity (VA) with/without lenses, refraction with/without lenses, slit lamp evaluation with fluorescein, topography, check of lens condition and decision on whether modifications are needed.
- The suggested follow-up schedule includes dispense visit, one day, one week, one month, three months, six months and one year. Varying between morning and afternoon visits can reveal how well the treatment is maintained throughout the day. If the modified lenses need to be ordered, the schedule may be changed.
4. Do: offer ortho-K to all patients who are candidates. When patients have a history of having active lifestyles, find glasses inconvenient, exhibit myopia progression or are contact lens dropouts, check their ortho-K candidacy and offer it as an alternative if possible.
Many times, parents and patients have not heard of ortho-K lenses and are intrigued to learn more.4 In general, good candidates have low-to-moderate myopia and mild-to-no with-the-rule astigmatism.
In adult patients, I discuss ortho-K with those experiencing mild dry eye and discomfort with conventional soft lenses, if there’s an interest in refractive surgery but they are pre-presbyopic or if they work in occupations or play sports that require good unaided acuity. For instance, a long-distance truck driver once expressed a strong desire to be glasses- and contact lens-free for when he had to load and unload boxes in various weather conditions.
 |
|
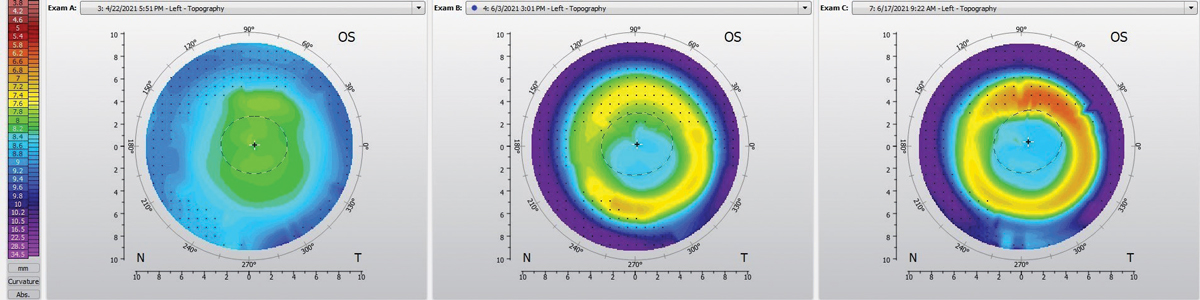
Fig. 2. Pre-ortho-K OS topography (left), post-ortho-K after one week of follow-up (right). Click image to enlarge. |
Hard Lessons
Unfortunately, not all outcomes will turn out as expected. Certain situations can complicate the fitting process and drag you down.
1. Don’t: make changes too early in the fitting process and chase perfection. As mentioned prior, these lenses can take longer to take effect in certain patient populations. The only time new lenses should be ordered at the one-day or one-week follow-up is if there is lens adherence, excessive decentration or corneal staining. Otherwise, give the eye up to two weeks to acclimate.
Patients with low myopia can be functional with their uncorrected myopia. In patients with moderate myopia, dispense daily disposable contact lenses in the first week while the myopia is reduced. Sometimes, the topography might not look perfect—as long as the treatment zone is complete and the patient is 20/happy, we’re happy.
2. Don’t: forget to set expectations and screen out bad candidates. Some patients may want crisp 20/20 uncorrected vision after treatment, and this may be unrealistic due to potential glare or poor treatment response. High residual lenticular astigmatism might influence the outcome. There are limitations with ortho-K, and a goal to set may be improving unaided vision, instead of correcting all refractive changes.
Absolute contraindications include keratoconus, corneal dystrophies and active anterior segment pathology.
Relatively bad candidates include patients who have irregular or limbus-to-limbus astigmatism, which will cause lenses to decenter superiorly or leave patients with more overall astigmatism. Toric ortho-K lenses exist for these more complex patients.
3. Don’t: use bad data. This is especially true if using software-based designs. In existing GP wearers, let corneas normalize before starting ortho-K. If not, the initial maps will be inaccurate, leading to excessive follow-ups and lens reorders. So, invest that time upfront to save time in the long run.
4. Don’t: forget to test binocular vision in candidates. Although uncommon, patients with variable refractive endpoints warrant treatment and management prior to attempting ortho-K. Imagine how frustrating it would be to fit ortho-K in a patient with accommodative spasms!
Now that we’ve gone over the good and the bad, let’s review some ortho-K cases that a clinician might come across.
 |
|
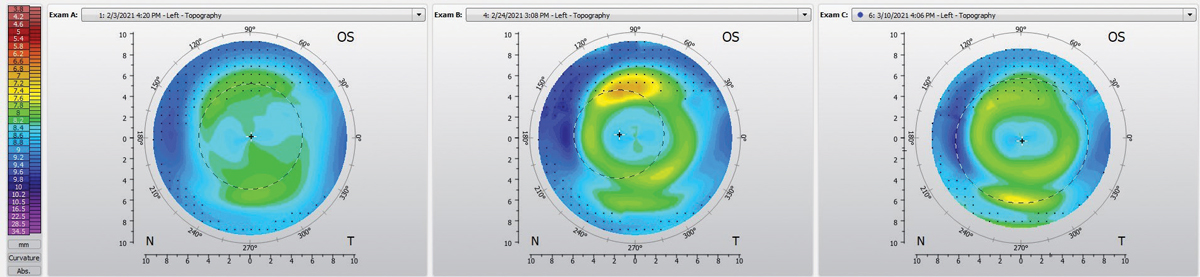
Fig. 3. Pre-ortho-K treatment corneal topography (left), one week after starting ortho-K (center), topography after modifying lens to have a toric landing zone (right). Click image to enlarge. |
Patient with Low Myopia
A 13-year-old Caucasian male presented for a myopia management consultation after having a comprehensive eye exam with another doctor in my practice. The parents were worried that his prescription had progressed 1.00D OU in the last year. The dad being myopic and the mom being emmetropic, they wanted him to be glasses-free while playing sports and to have myopia management at the same time. Their son also frequently took naps during the day and enjoyed swimming.
The refraction was -2.00 DS (20/20) OD and -3.25+0.50x85 (20/20) OS. Binocular vision testing and ocular health examination were unremarkable. Corneal topographic data from the Oculus Keratograph 5M showed the presence of minimal central corneal astigmatism. K values were 41.3/42.2@82 OD and 41.5/42.1@92 OS. The axial length as measured with the A-scan before ortho-K was 24.96mm OD, 25.23mm OS. HVID 11.89mm OD, 12.02mm OS.
Given that he enjoys swimming and taking frequent daytime naps, I advised against soft contact lenses and strongly recommended ortho-K. A set of lenses was empirically ordered from CooperVision Paragon CRT through the company’s lens calculator.
The lenses ordered were:
- OD: CRT dual axis 8.7/11.0, return zone depth (RZD) 1: 525 and RZD 2: 525, Landing zone angle (LZA) 1: 32, LZA 2: 33, optic zone diameter (OZD): 5mm, power: +0.50, material: Menicon Z.
- OS: CRT dual axis 8.9/ 11.0, RZD 1: 525 and RZD 2: 575 LZA 1: 32 and LZA 2: 33, power: +0.50, material: Menicon Z, OZD: 5mm.
At the one-day follow-up, the VA was 20/25 OD and OS. The sodium fluorescein pattern showed good centration, 4mm treatment zone, uniform landing in the landing zone and adequate 0.5mm edge lift. The cornea was clear. Subjective refraction was -0.25 OD and -0.25 OS. The refraction over the lenses was +0.75 OD and +0.50 OS. No new lens was ordered.
At the two-week follow-up, he was extremely happy with his vision and the quality. His uncorrected distance vision was 20/15 OD and 20/20 OS. The over-refraction over the lenses was +0.75DS OD and +0.50DS OS. The slit lamp examination with sodium fluorescein showed an ideal fit.
The corneal health without the lenses was good with no staining present. The topographies showed even treatment OU, with mild decentration temporally OD and slight decentration inferiorly OS (Figures 1 and 2).
Discussion: This was a slam-dunk, easy case for ortho-K. The patient had a low amount of corneal astigmatism and was motivated to be contacts- and glasses-free during the day. Soft contact lenses contraindicated in this patient, as he was a swimmer and took naps throughout the day.
Notice that the treatment ring appears to be decentered relative to the geometric center but is centered with the visual axis to offer the myopia control desired. The patient was 20/happy and additional lens modifications were not necessary.
 |
|
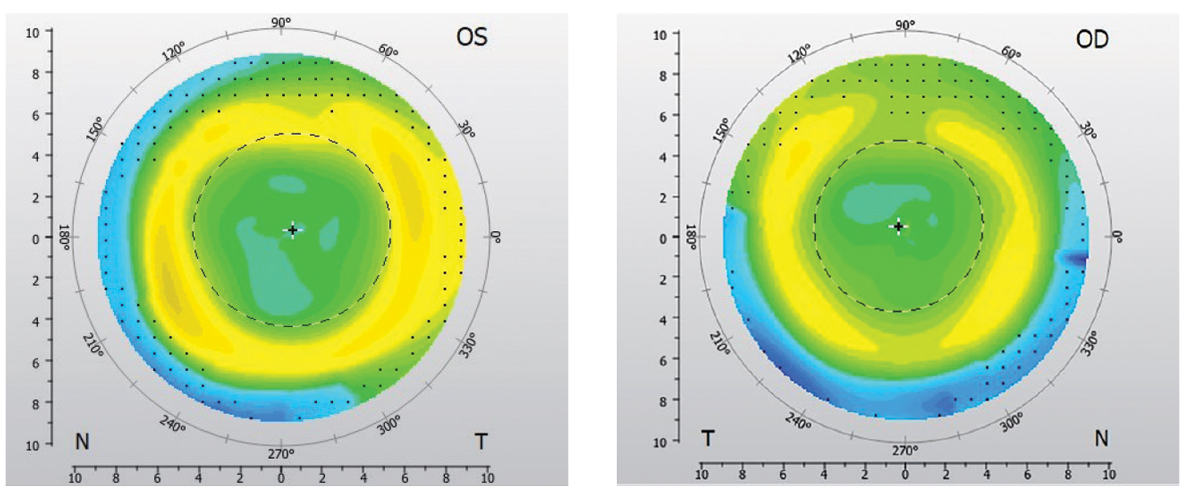
Fig. 4. Pre-ortho-K topographies OS (left) and OD (right) with visible post-LASIK pattern. Click image to enlarge. |
Monocular Ortho-K in Patient with Anisometropia
An 11-year-old Asian male presented for a contact lens fitting in the left eye due to history of anisometropia. The uncorrected VA was 20/20 OD and 20/100 OS. The subjective refraction was plano (20/20) OD and -1.50 (20/20) OS. Ks were 41.25/42.75@75 OD, 40/40.25@100 OS. HVIDs were 11.86mm OD and 11.84mm OS. The binocular vision status and ocular health were unremarkable.
The mother of the patient requested to pursue ortho-K fitting OS despite the possibility of myopia progression OD. The lens ordered empirically was: Paragon CRT: 8.7/10.5, RZD: 500, LZA 32, OZD: 5mm, power: +0.50, material: Paragon HDS. Moving forward, only the OS will be discussed.
At the next follow-up, the entering acuity without the lens was 20/20. The refraction over the lens was -0.50D. The sodium fluorescein pattern with slit lamp revealed a well-centered lens with adequate edge lift 360º but an uneven return zone.
A few modifications were made: the base curve was adjusted to account for the over-refraction. For every 0.10D change in base curve, there is a 0.50D change in power. The lens was reordered with a toric return zone: Paragon CRT 8.8/10.5, RZD 1: 500 and RZD 2: 550, LZA 32, power: +0.50, material: Paragon HDS.
At the follow-up with the new lens, the VA was 20/20. The topography showed a more even treatment zone (Figure 3). The refraction without the lens was plano and the refraction over the lens was +0.50 DS.
Discussion: This case highlighted the application of ortho-K in managing unilateral myopia to slow myopic progression and reduce anisometropic values. Since contact lens wear in anisometropia will reduce aniseikonia too, ortho-K was a great option. Interestingly, there is a subset of research on the topic of ortho-K in managing unilateral myopia with monocular vs. binocular ortho-K, but more prospective studies with longer follow-ups are needed.5
In this case, the ortho-K lens did not have a uniform return zone on the cornea. The Paragon dual axis lens design allows for modifications to be made to improve centration and treatment if there is toricity in the return zone, the landing zone or both.
 |
|
Figs. 5 and 6. Post-ortho-K one-day (left) and two-week (right) follow-up and topography OD. Click image to enlarge. |
Post-LASIK Monovision in Patient with Early Presbyopia
A 45-year-old Asian female presented with blurry vision at a distance in both eyes. Her ocular history was remarkable for myopic LASIK OU 10 years ago. She could not recall her pre-LASIK prescription ranges. She was currently wearing glasses for driving, especially at night. She was interested in more independence from wearing spectacles and contact lenses but was not interested in refractive surgery retreatment. After extensive discussion on options, she was mostly interested in monovision ortho-K.
Her uncorrected VA was 20/40 OD and OS. Ks were 40.75/41@75 OD DS, 40.75/41.00@140 OS. Subjective refraction was -1.00 OD and OS, with +1.00 add. She was OD dominant. HVIDs were 11.30mm OD and 11.37mm OS. Baseline topographies showed a large central zone of corneal flattening consistent with myopic LASIK correction surrounded by relative corneal steeping in the mid-periphery and no signs of ectasia or corneal irregularities (Figure 4).
Ocular health was unremarkable in each eye. Considering a relatively spherical central cornea OU and the need to correct low myopia, we discussed ortho-K as an option. However, since the patient had never tried monovision before, a trial with soft contact lenses was performed first. She was given Johnson and Johnson Acuvue 1-Day Moist -1.00DS for use OD only to trial monovision for two weeks. VA OD was 20/20. If well-tolerated, she could call back to the clinic to continue.
After two weeks, she called back and was ready to proceed with monovision. Since the case is more complicated than a classic case of ortho-K, the lens consultant was given more background information and a new lens was empirically ordered: Paragon CRT 8.7/10.5, RZA: 500, LZA: 32, power: +0.50D, material: Menicon Z.
At the one-day ortho-K follow-up, the uncorrected VA OD and OS was 20/40. Subjective refraction was -1.00DS. Refraction over the lens was plano. Slit lamp examination showed ideal contact lens alignment and no corneal health concerns. No changes were made to the visit. Topography showed an early, incomplete treatment ring (Figure 5).
Since there were difficulties with scheduling a standard one-week follow-up, the patient returned for a two-week follow-up (Figure 6). At this visit, she reported that her vision improved. The uncorrected VA was 20/20 OD and 20/40 OS. Refraction was -0.50 OD and was -1.00DS OS. Refraction over the OD lens was plano. Slit lamp examination showed an ideal fit with the lens on and no corneal health concerns. No changes were made to the visit. Topographies showed a complete and well-centered treatment ring.
Discussion: Post-LASIK myopic regression is infrequently observed and has significant implications on a patient’s quality of life.6,7 Theoretically, LASIK surgery only affects the corneal stromal layer and not the epithelial layer. In ortho-K where the treatment effect occurs in the epithelial layer, the post-LASIK cornea theoretically should be able to respond to the intervention.
Since conventional ortho-K lenses are designed for normal prolate corneas, instead of oblate post-LASIK corneas, the clinician should set the expectation that more lens orders may be necessary to obtain good lens centration and fit.
Monovision ortho-K is one option of managing early presbyopes to keep them glasses- and contact lens-free for as long as possible.
 |
|
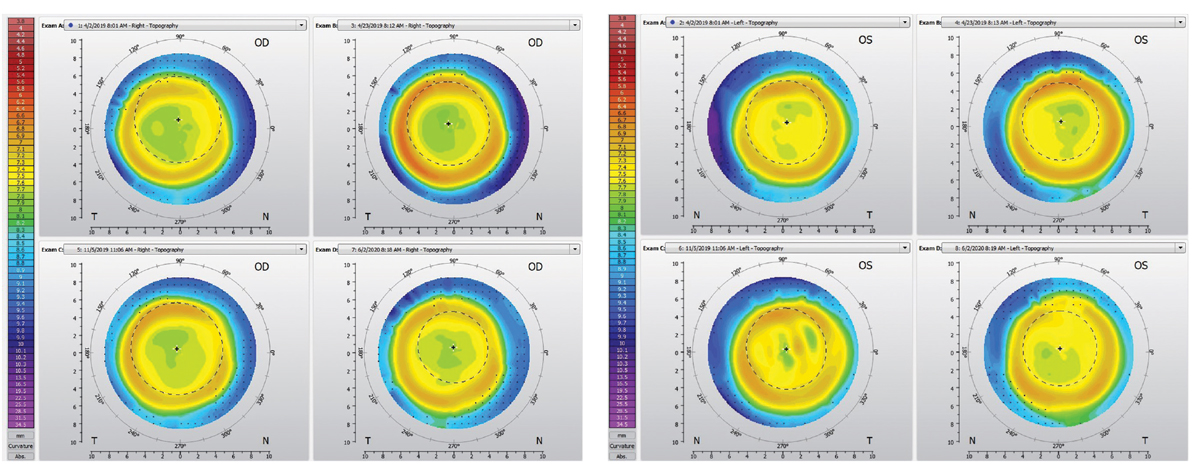
Figs. 7 and 8. Changes in corneal topography over the course of treatment OD (left) and OS (right), that includes one-week follow-up (top left corner of each figure), two-week follow-up (top right), six-month follow-up (bottom left) and one-year follow-up (bottom right). Click image to enlarge. |
Young Adult Patient
A 24-year-old Caucasian female presented to the clinic to inquire about ortho-K. She was motivated to pursue refractive surgery but is concerned about the cost and permanence. She did not any prior experience wearing contact lenses.
Her entering acuity was 20/100 OD and 20/100+ OS. Ks were 45/45.75@86 OD and 45.75 Sph OS. Subjective refraction was -2.00 OD and OS (20/20 in both eyes) and HVIDs were 11.46mm OD, 11.50mm OS.
The binocular vision status and ocular health were unremarkable. Based on her motivation, Ks and refraction, she was a candidate for ortho-K, and initial lenses were ordered empirically.
Parameters ordered were the same for both eyes: Paragon CRT 7.8/10.50, RZA: 550, LZA: 34, OZD: 6mm, power: +0.50D, material: Menicon Z.
At one-week follow-up, uncorrected VA was 20/30 OD/OS. The slit lamp corneal health check was unremarkable. The lens fit on the eye looked ideal. Subjective refraction was -0.50DS. The lenses were reordered with 7.9 base curve OU.
At the two-week follow-up, the uncorrected VA was 20/20+ OD and 20/20 OS. The patient was happy with the improvement in vision quality. Subjective refraction was +0.25 OD and +0.50 OS.
At the six-month and subsequent one-year follow-up, the VA uncorrected, subjective refraction and corneal health remained stable (Figures 7 and 8).
Discussion: Ortho-K is attractive to patients as an alternative to refractive surgery because the treatment is reversible and involves a relatively lower risk. This case highlights the difference in fitting adults vs. kids. In kids, the optic/treatment zone tends to be smaller (5.0mm to 5.5mm) to allow for more relative peripheral myopic defocus for myopia management; however, in adults, larger optic zones are better tolerated, as they reduce aberrations that can cause symptomatic halos/glares.8
Ortho-K is a complex fitting technique that requires time to develop an understanding. Thankfully, clinicians can start with the basics and build their understanding of different lens design approaches. Hard lessons learned ensure that there is quality data collection, patience, realistic expectations, and good patient selection.
Understanding the wide range of ortho-K candidates will open up the potential for more patients to benefit from this unique lens modality.
Dr. Chang is a residency-trained optometrist in California. She is a Fellow of the American Academy of Optometry. She is a speaker for ZenLens and is a clinical sales consultant for Johnson & Johnson.
1. Swarbrick HA. Orthokeratology (corneal refractive therapy): what is it and how does it work? Eye Contact Lens. 2004;30(4):181-5. 2. Sridhar MS. Anatomy of cornea and ocular surface. Indian J Ophthalmol. 2018;66(2):190-4. 3. Duong K, Pucker AD, McGwin G Jr, et al. Established soft contact lens wearers’ awareness of and initial experiences with orthokeratology. Ophthalmic Physiol Opt. 2021;41(4):673-82. 4. Tsai HR, Wang JH, Chiu CJ. Effect of orthokeratology on anisometropia control: a meta-analysis. J Formos Med Assoc. 2021;S0929-6646(21):00239-4. 5. Ren Q, Yang B, Liu L, Cho P. Orthokeratology in adults and factors affecting success: study design and preliminary results. Cont Lens Anterior Eye. 2020;43(6):595-601 6. Yan MK, Chang JS, Chan TC. Refractive regression after laser in situ keratomileusis. Clin Exp Ophthalmol. 2018;46(8):934-44. 7. Ikeda T, Shimizu K, Igarashi A, et al. Twelve-year follow-up of laser in situ keratomileusis for moderate to high myopia. Biomed Res Int. 2017;2017;9391436. 8. Ren Q, Yang B, Liu L, Cho P. Orthokeratology in adults and factors affecting success: study design and preliminary results. Contact Lens Anterior Eye. 2020;43(6):595-601. |


