Scleral contact lens fitting can be an excellent option for patients with both corneal irregularities and ocular surface diseases (OSDs), even when the initial assessment poses challenges. The following cases outline strategies aimed at assisting patients to achieve successful lens wear despite initial obstacles.
The first case describes scleral lens fitting for a child with partial limbal stem cell deficiency and severe dry eye. Special considerations were taken in order to ensure the patient and his family felt at ease, while adjustments to lens design and overall diameter were made as proficiency in lens application and removal was achieved.
The second demonstrates that although visual improvement could be attained with corneal gas permeable (GP) and hybrid lenses in a patient with corneal irregularities and a history of glaucoma surgery, ultimately an impression-based custom scleral provided optimal comfort, with ocular surface support and exceptional visual clarity.
Case One
 |
|
Fig. 1. This scleral lens light and stand allowed the patient to have two free hands to fully retract the upper and lower eyelids during lens application. |
A 10-year-old Asian male was referred due to severe dry eye and light sensitivity in both eyes. His past ocular history included keratoconjunctivitis sicca, corneal neovascularization, limbal stem cell deficiency, high myopia and bilateral amblyopia. His current ocular medications included cyclosporine ophthalmic emulsion 0.05% twice daily, non-preserved artificial tears every two hours and non-preserved lubricating ophthalmic ointment twice daily. He received his first pair of prescription spectacles at age eight and had no prior contact lens use.
His medical history was significant for ichthyosis follicularis, alopecia and photophobia (IFAP) syndrome, an extremely rare X-linked oculocutaneous genetic disorder is caused by a mutation to the MBTPS2 gene.1,2 The patient’s diagnosis was confirmed by a pediatric dermatologist with genetic testing. Worldwide, only around 40 patients have been identified to have IFAP syndrome.2 The patient was adopted internationally at age seven and his family medical history was unknown.
Upon arrival in the United States, he was noted to have visual issues. He was holding things close to see them while also avoiding bright lights and seeking out shade. On physical examination, he had nail dystrophy, no body hair on the head nor extremities and scaly skin on the arms, legs and the bottoms of the feet.
Initial Evaluation
The patient’s entering visual acuities were 20/80 OD and 20/100 OS with spectacle correction of -9.25D sphere OD and -13.00D sphere OS.
Pupils were equal and reactive, and the extraocular muscles had full range of motion. Slit lamp examination was challenging due to severe photophobia. There were no eyebrows or eyelashes. Silicone punctal plugs were present in the lower puncta, which had been placed during an exam under general anesthesia. There was mild diffuse conjunctival injection and diffuse 2-3+ punctate epithelial erosions with peripheral subepithelial opacity and vascularization of both corneas. The anterior chambers were deep and quiet and the lens clear. The dilated fundus exam was normal.
There was a long discussion with the patient and his parents about scleral lenses, their benefits and handling requirements. It is important to answer all questions and discuss the need for daily application and removal, and follow the patient closely prior to initiating lens fitting to manage expectations.
Lens application was attempted with a small-diameter 15mm scleral lens on the right eye. The patient squeezed his eyelids causing eversion and pulled backward repeatedly. Despite additional attempts using an LED light to help maintain downward fixation, as well as filling the lens with a viscous non-preserved artificial tear, attempts at lens application were unsuccessful.
The decision was made with the family to continue close follow-up with the pediatric cornea specialist and return for repeat evaluation in the future. They were also advised to practice holding the eyelids at home to increase familiarity with the lens application process.
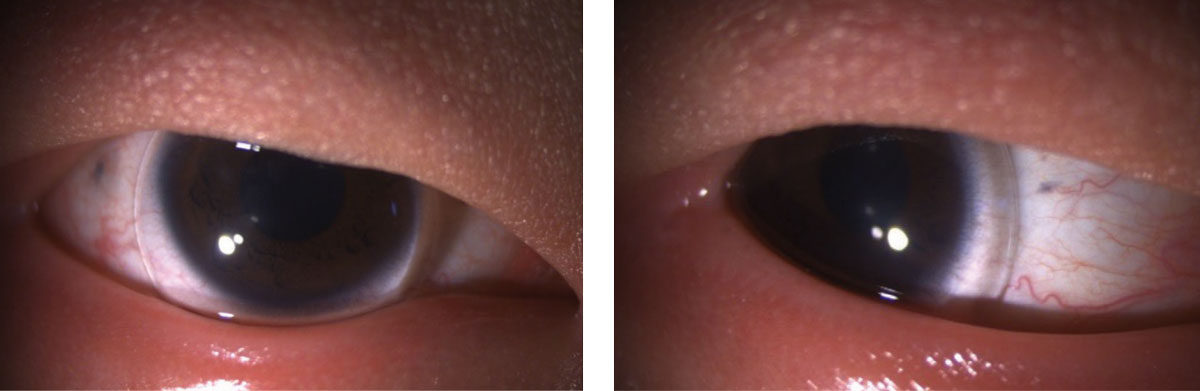 |
| Figs. 2 and 3. The 14mm lens on the right eye had excessive post-lens tear reservoir centrally and complete limbal clearance with a small area of landing zone on the conjunctiva (left). The 14mm lens on the left eye had slightly excessive post-lens tear reservoir and adequate limbal clearance with a small area of scleral landing zone (right). Click image to enlarge. |
Repeat Scleral Lens Evaluation
Three years later, the 13-year-old patient was again referred by their cornea specialist for evaluation for therapeutic scleral lenses. Visual acuity with spectacles was 20/125 pinhole 20/100 OD and 20/100 pinhole 20/70 OS. Slit lamp examination findings remained stable with peripheral corneal pannus and diffuse punctate epithelial erosions OU.
After numerous attempts, a diagnostic scleral lens with a 14.9mm diameter, 7.4mm base curve and -3.50D spherical power was successfully applied to the right eye without application bubbles. The lens demonstrated excessive post-lens tear reservoir with scleral landing zone edge compression and vascular blanching. An over-refraction of -20.00D sphere improved vision acuity to 20/50 in the right eye.
We discussed scleral lenses and daily handling requirements with the patient and his parents. Potential issues with lens wear including fogging or clouding of the vision and lens front surface non-wetting, which may require lens removal, cleaning and reapplication during the day were discussed.
Although the long-term goal was to fit both eyes in order to provide ocular surface protection, the decision was to start with the right eye only due to significant difficulty and stress of applying the right lens in office. The initial right scleral lens was ordered in hyper-GP material tisilfocon A to maximize oxygen transmissibility due to corneal neovascularization. The lens was designed with an unusually small 14mm overall diameter to facilitate easier lens application during the upcoming training visit. A flatter base curve was also selected in order to reduce the refractive power of the lens as well as to ensure complete clearance of the limbus due to the patient’s history of partial limbal stem cell deficiency. Prior treatments included topical steroid and elimination of topical preservatives. Only a right lens was ordered with the plan to use it for fitting of the left eye once in-office lens application was successful.
Pediatric Scleral Lens Application and Removal Training
The patient was scheduled on a day when there was ample time to allow for an extended training session with time for breaks. The exam room lights were dimmed to reduce light sensitivity. A scleral lens stand with LED fixation light was used during scleral lens application training (Figure 1).
A cup of hot water was used to warm the non-preserved viscous artificial tears to body temperature. The warmed solution can reduce some patients’ reflex to pull back. Additionally, a viscous filling solution can help reduce the likelihood of application bubbles. The parents were guided to help coach the patient and observe lens application from the side, which allowed them to let the patient know when to pull back and stop if he was off-center or if his eyelids were bumping the scleral lens.
The first scleral lens with 9.0mm base curve, 14.0mm diameter and -10.75D power with toric scleral landing zone was applied bubble-free to the right eye (Figure 2). Vision in the right eye was 20/50 with -0.50D spherical over-refraction. The lens overall diameter was small for the patient’s cornea.
Next, the lens was removed from the right eye and used as a diagnostic fitting lens for the left eye (Figure 3). Vision was 20/40 with plano sphere over-refraction.
With extensive training, the patient was able to safely apply and remove the 14mm scleral lens on his right and left eyes at this visit. The family was educated that a larger-diameter lens would be needed in the future. A new set of lenses were ordered with plan for repeat lens application and removal training at the next visit. The right scleral lens was ordered with 14.0mm diameter, decreased sagittal height and a power -11.25D. The initial left scleral lens was ordered with tisilfocon A material, 9.0mm base curve, 14.0mm diameter, -10.75D power and decreased central sagittal height with toric scleral landing zone.
Follow-up
One month later, the patient returned for repeat lens application and removal training with the new right and left 14.0mm scleral lenses. He reported good comfort with the lenses and easier lens application with the right eye compared to the left eye initially using a stand with LED light. Vision was 20/50 OD and 20/50 OS. The right lens had 250µm in the post-lens tear reservoir, mild inferior decentration, adequate limbal clearance and mild scleral landing zone edge compression. The left lens had 200µm in the post-lens tear reservoir, mild inferior decentration, adequate limbal clearance and mild scleral landing zone edge compression.
He was provided with clear written instructions describing the lens application, lens removal and disinfection process, which included images of the recommended lens filling and disinfection solutions. He was instructed to limit lens wear to four to six hours until his next visit scheduled one week later.
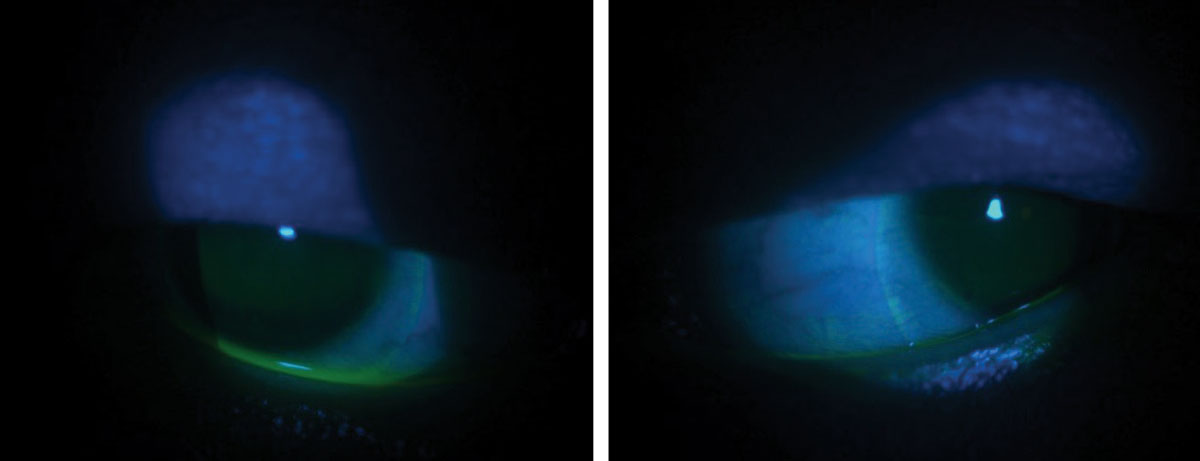 |
Fig. 4. The patient’s eyes after 14mm scleral lenses were removed. There is an impression of the conjunctival tissue as well as staining with fluorescein. Click image to enlarge. |
The patient returned one week later as directed wearing scleral lenses in both eyes. His vision was 20/50 OU. He reported no issues with lens application but did note that at end of the day that the lenses “felt stuck” and were difficult to remove.
The right lens had 200µm in the post-lens tear reservoir, mild inferior decentration and adequate limbal clearance with mild scleral landing zone edge compression. The left lens had 100µm in the post-lens tear reservoir, mild inferior decentration and adequate limbal clearance with mild scleral landing zone edge compression as well.
The lenses were slightly difficult to remove despite wetting the patient’s eyes and removal suction cup with non-preserved saline solution prior to removal and placing the suction cup near the edge of the lens. After removal, his ocular surface was evaluated with fluorescein dye. There were no corneal punctate epithelial erosions; however, there were impression rings on the conjunctival from the scleral lenses on both eyes (Figure 4).
A new set of lenses were ordered; they were redesigned with a larger diameter and flatter scleral landing zone in order to more evenly distribute the weight of the lens on the conjunctival tissue. The patient was instructed to limit his lens wear to four to six continuous hours until the new lenses were received and to return for follow-up one month later.
Follow-upThe patient returned using the newest 16mm-diameter scleral lenses. He reported good comfort and clear vision with the lenses. On the day of the exam, he had worn the lenses for four hours continuously. He noted occasionally fogginess of his vision that would improve with lens removal, cleaning and reapplication. He reported no further difficulties with lens application or removal. Visual acuities were measured as 20/40 OD and 20/30 OS.
Both lenses had 300µm of post-lens tear reservoir, with complete limbal clearance and adequate scleral landing zone alignment. The lenses were removed easily without evidence of corneal or conjunctival impression or stain with fluorescein dye.
Over the past three years, the patient has continued to successfully wear his therapeutic scleral lenses 14 hours per day. His cornea specialist recommended midday removal and reapplication with fresh non-preserved saline solution when possible to reduce the likelihood of inflammatory cytokines building up in the post-lens tear reservoir.
This case demonstrates the value of fitting therapeutic scleral lenses in patients with limbal stem cell deficiency and severe dry eye even when lens application is initially challenging. This patient had improvement in dry eye symptoms while also improving his vision. When working with pediatric patients, it is important to proceed slowly to gain their trust and achieve long-term success. OSD has been reported to the most common indication for pediatric scleral lens fitting.3,4 Scleral lenses can be particularly beneficial for pediatric patients with OSD and irregular astigmatism like this patient. Scleral lens wear has been shown to stabilize the ocular surface, enhance vision and improve ocular comfort while minimizing progression in ocular signs of a patient with limbal stem cell deficiency related to ectrodactyly-ectodermal dysplasia-clefting syndrome over a period of 10 years.5
It is important to closely monitor patients with limbal stem cell disease when initiating therapeutic scleral lens wear. Particular attention should be made to ensure proper lens fitting without negative impact on the ocular surface. Efforts should be made to scheduling follow-up visits in the middle to late afternoon in order to evaluate the lens after settling. The scleral lens should be removed during every office visit to fully evaluate the ocular surface with fluorescein dye and allow for early identification of potential issues.
 |
|
Fig. 5. The patient’s left eye had a glaucoma drainage device superior temporal. |
Case Two
A 59-year-old Caucasian male was referred by his glaucoma specialist for evaluation. His chief complaint was blurry vision in his left eye with a “ghost/overlapping” image. He had no visual complaints with his right eye.
The patient’s past ocular history included moderate open-angle glaucoma status post-endoscopic cyclophotocoagulation OU, Baerveldt glaucoma drainage implant surgery OS, bilateral pseudophakia, pars plana vitrectomy for rhegmatogenous retinal detachment OS, high myopia status post-LASIK refractive surgery, OSD with neurotrophic keratitis, chronic uveitis and cystoid macular edema OS.
He reported past use of corneal GP lenses 25 years ago and soft contact lens use 15 years prior. Ocular medications included dorzolamide 2%/timolol 0.5% twice daily, latanoprost 0.005% daily, non-preserved methylprednisolone three times daily, 50% autologous serum eye drops and cyclosporine ophthalmic emulsion 0.05% twice daily. Past medical history included gastroesophageal reflux disease and benign thyroid nodule.
Initial Evaluation
His baseline uncorrected visual acuities were 20/25 pinhole 20/20 OD and 20/60 pinhole no improvement OS. Corneal tomography revealed irregular corneal astigmatism with simulated Ks of 42.58/40.74@ 108 OD; 42.56/41.42@ 138 OS. Extraocular muscles had full range of motion and there was a left relative afferent pupillary defect. Intraocular pressures were 21mm Hg OD and 14mm Hg OS. Baseline pachymetry readings were 432 OD and 413 OS. Manifest refraction of +0.25D sphere corrected vision to 20/20 OD and -0.25D +1.25Dx116 to 20/60 OS.
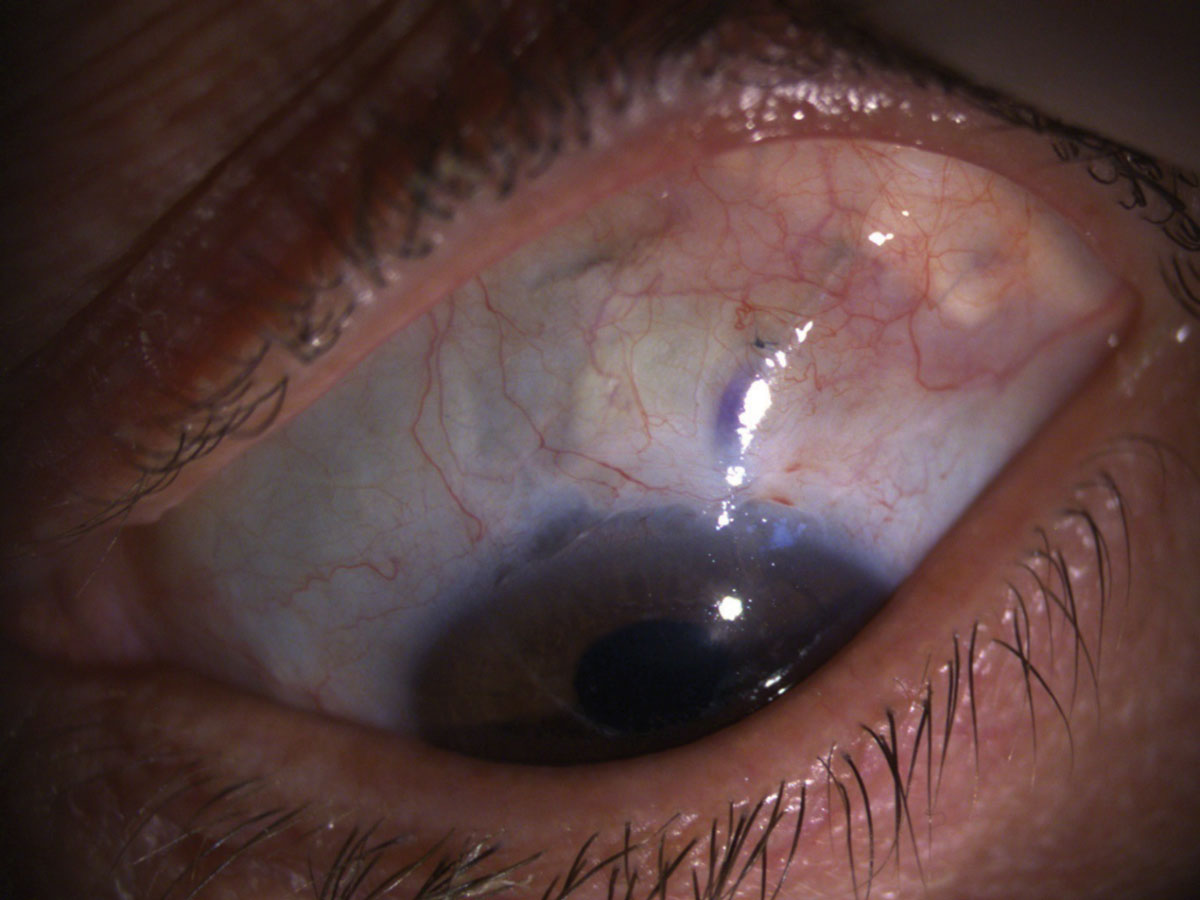
Slit lamp examination revealed 1+ inspissated meibomian glands and mild ptosis OS. His glaucoma drainage device superior temporal left eye was well covered with no evidence of conjunctival erosion (Figure 5).
His corneas had peripheral LASIK scars. The right cornea was clear centrally and the left had 1-2+ central punctate epithelial erosions. The anterior chamber was deep and quiet in the right eye and quiet with well-positioned tube in the left eye, flat iris and posterior chamber intraocular lenses present both eyes.
Contact Lens Evaluation
The patient’s complicated past ocular history as well as chief complaint were taken into consideration when considering the contact lens modality to consider initially. Special considerations were made due to his history of OSD and glaucoma with abnormal conjunctival elevation left eye after glaucoma drainage device implantation.
Initial Evaluation
The decision was made to trial a diagnostic scleral lens on the left eye due to the presence of keratopathy, irregular corneal astigmatism and minimal improvement in visual acuity with manifest refraction. An oblate lens design was selected due to the corneal shape after refractive surgery with a standard spherical landing scleral zone. Despite visual acuity improvement to 20/40, fitting was not immediately pursued further due to poor comfort in office and moderate scleral landing zone compression of the conjunctival tissue covering the glaucoma drainage device superior temporally.
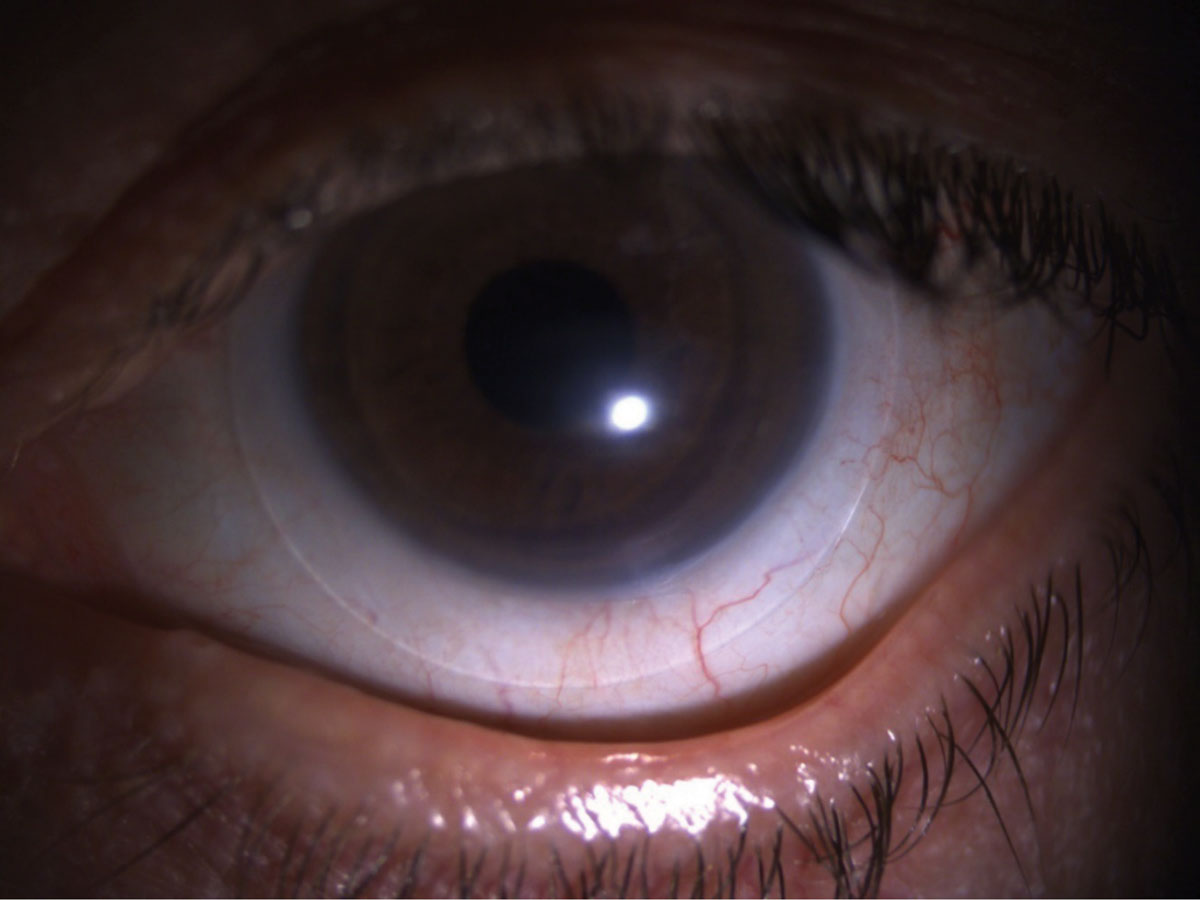 |
Fig. 6. The patient was fit with a hybrid contact lens. Click image to enlarge. |
Next, a corneal GP lens was considered to address the patient’s chief complaint of doubling or overlapping images in his left eye. A diagnostic corneal GP lens was selected with an 11.0mm diameter, 7.85mm base curve, and +1.00D spherical power. The lens fit was evaluated with fluorescein dye revealing mild central pooling with adequate edge lift. Visual acuity improved to 20/40 with a -2.50D sphere over-refraction.
Options were discussed and the plan was to proceed with a trial of a piggyback system of a soft daily disposable contact lens to support the ocular surface with a corneal GP lens over the top to improve visual acuity. A soft daily disposable lens was fit for use as a piggyback lens. The corneal GP lens was ordered in a flatter base curve of 7.94mm, diameter 11.0mm, power -1.00D sphere with standard peripheral curves.
At the next visit, the patient reported discomfort, foreign body sensation and blurry vision with the piggyback lens system. Visual acuity was measured as 20/40 with no improvement with over-refraction in the left eye. He was provided the option to use the soft daily disposable lens alone as a therapeutic soft lens vs. the GP lens over the top to maximize visual clarity.
Repeat Commercial Scleral Lens FittingThe patient returned and complained of continued poor vision in the left eye. He was using the soft therapeutic lens alone and had issues with lens retention with frequent lens loss later in the day. His vision in the left eye was 20/40 improving to 20/30 with pinhole.
During slit lamp examination, he was noted to have 2-3+ punctate epithelial erosions with multiple filaments OU. Intraocular pressures remained stable at 12mm Hg OD and 13mm Hg OS. The right eye was fit with a daily disposable silicone hydrogel lens to support the ocular surface.
A diagnostic scleral lens was placed on the left eye with bi-tangential scleral landing zone and 16mm overall diameter. His vision improved to 20/20 OD and 20/25 OS.
A left scleral lens was ordered with base curve of 8.6mm, decreased overall diameter of 15.5mm, sagittal height of 3300μm, +0.25D power with the flattest scleral landing zone available from the manufacturer.
Despite these modifications to the scleral lens design, the landing zone continued to have moderate compression of the conjunctival tissue superior temporal in the location of the glaucoma drainage device.
One Month Follow-upThe patient returned with frequent complaints of ‘debris’ affecting his vision 15 minutes after lens application despite proper lens handling and disinfection. Vision was 20/20 OD with a soft daily disposable lens and 20/25 OS improving to 20/20 with over-refraction. He also complained of discomfort in the left eye requiring him to remove the scleral lens and take a break for a few days after using it.
On the day of the visit, he reported two hours of continuous lens wear time. The right lens was centered and had full corneal coverage and good movement with blink. The left scleral lens was decentered inferior nasally. The posterior tear film was estimated to be 350µm with complete limbal clearance. The flat scleral landing zone was at 75° with moderate conjunctival compression. Upon lens removal and evaluation with fluorescein dye, there was noted to be impression and staining of the conjunctival tissue superior temporal and inferior nasal.
Left Eye Refitting ConsiderationsThere was a long discussion with the patient regarding borderline fit with the left scleral lens and evidence of compression and stain of the conjunctiva overlying the glaucoma drainage tube. The scleral landing zone toricity had already been adjusted, and we were unable to further flatten the scleral landing zone.
After discussing the risks (including conjunctival erosion over the tube, infection, vision loss and need for additional surgery), the decision was made to discontinue scleral lens wear in the left eye. Alternative options included refitting into a hybrid lens, fitting a scleral lens with a custom notch to avoid the elevated glaucoma drainage device or refitting with a custom impression-based lens design to better align with the ocular surface.
The patient was fit with a hybrid contact lens with a GP center lens surrounded by a silicone hydrogel soft skirt (Figure 6). This lens could potentially improve visual acuity by masking irregular corneal astigmatism with lens mechanical interaction with the elevated conjunctival tissue over the glaucoma drainage device. Ultimately, the desire for added ocular surface protection from the post-tear film reservoir guided the decision to pursue impression-based lens fitting.
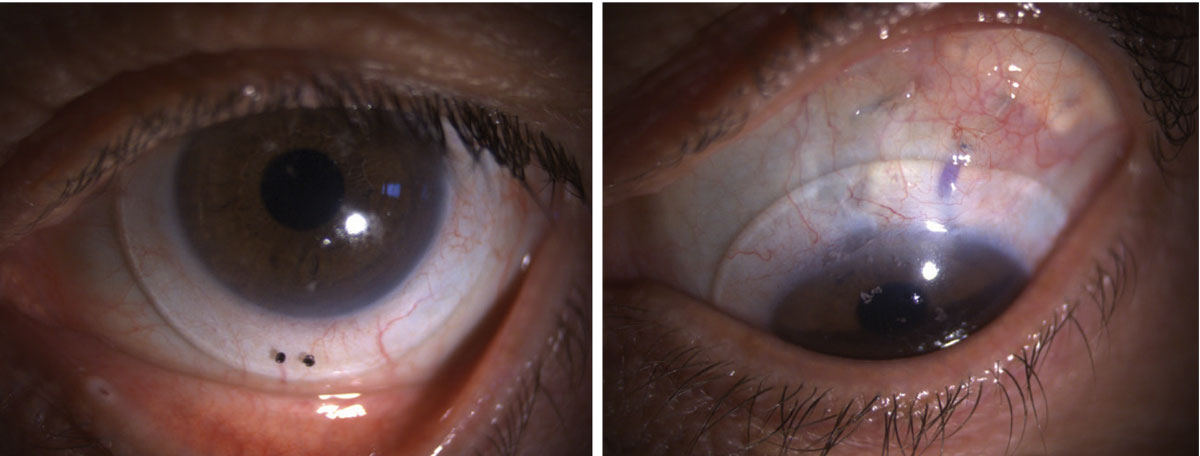 |
Fig. 7. Impression-based custom lens on the left eye. The area of conjunctival elevation over the glaucoma drainage device is well-aligned (right image). |
The patient was instructed to discontinue lens use and to return for impression. At this visit, his vision was 20/80 pinhole no improvement OS. The impression was acquired using an FDA-approved ocular compound and an insertion tray, and the mold was sent to the manufacturer for custom lens design and fabrication. The desired optical parameters were requested based on previous GP lens data.
The initial impression-based custom scleral lens was designed with fluorosilicone acrylate material, Tangible Hydra-PEG lens coating, base curve 8.093mm, diameter 17.5mm power, -0.25D sphere and optic zone of 9.43x7.77mm. Vision was 20/20 OS. The lens oriented properly with two dots down and no rotation. There were 300µm of posterior tear film centrally and adequate limbal clearance 360°. The scleral landing zone was well-aligned to the conjunctival elevations with no vascular blanching (Figure 7).
The lens was easily removed in office. There was no conjunctival impression or stain with fluorescein dye.
This case highlights the use and benefits of a variety of contact lens modalities in a patient with OSD on long-term topical glaucoma therapies. Consideration should be made to switching patients to non-preserved or BAK-free formulations of glaucoma mediations when possible to improve OSD. Soft therapeutic daily disposable lenses are an option to support the ocular surface, improve epithelial healing and reduce pain in patients with mild to moderate OSD. In patients with visual complaints due to irregular corneal astigmatism, corneal GP and hybrid lenses can improve visual function after LASIK such as this patient.6,7 Scleral lenses can be used to both improve visual acuity and support the ocular surface and have been identified as the first option for management of corneal irregularity more frequently than corneal GP lenses, while scleral lenses are typically considered for management of OSD topical medical therapies, meibomian gland expression and punctal occlusion are attempted.8
Patients with complex eye disease who were unable to successfully use standard scleral lenses can achieve visual and therapeutic success with custom, impression-based scleral lens.9,10 In patients with abnormal conjunctival elevations, such as this patient with history of glaucoma drainage device, close monitoring is required with lens removal and evaluation with fluorescein to identify any risk of conjunctival impression or erosion of the conjunctival tissue. These patients benefit from close collaboration between their contact lens and glaucoma specialist to ensure long-term safety. A custom, impression-based lens design can be used to closely align the ocular surface and prevent conjunctival erosion and further serious complications.
Takeaways
Practitioners should allocate extra time and leverage highly trained support staff to assist pediatric patients and their families effectively. Follow-up appointments, ideally scheduled for mid to late afternoon, should include lens removal and a thorough assessment of the ocular surface to identify potential fit issues and guide adjustments to lens design.
1. Oeffner F, Fischer G, Happle R, et al. IFAP syndrome is caused by deficiency in MBTPS2, an intramembrane zinc metalloprotease essential for cholesterol homeostasis and ER stress response. Am J Hum Genet. 2009;84(4):459-67. 2. Mégarbané H, Mégarbané A. Ichthyosis follicularis, alopecia and photophobia (IFAP) syndrome. Orphanet J Rare Dis. 2011;6:29. 3. Gungor I, Schor K, Rosenthal P, Jacobs DS. The Boston Scleral Lens in the treatment of pediatric patients. J AAPOS. 2008;12(3):263-7. 4. Rathi VM, Mandathara PS, Vaddavalli PK, et al. Fluid filled scleral contact lens in pediatric patients: challenges and outcome. Cont Lens Anterior Eye. 2012;35(4):189-92. 5. Labunski A, Carrasquillo KG, Brocks D. Treatment and management of ectrodactyly-ectodermal dysplasia-clefting syndrome with scleral prosthetic devices. Eye Contact Lens. 2023;49(6):262-5. 6. Ward MA. Visual rehabilitation with contact lenses after laser in situ keratomileusis. J Refract Surg. 2001;17(4):433-40. 7. Piñero DP, Pérez-Cambrodí RJ, Ruiz-Fortes P, Blanes-Mompó FJ. New-generation hybrid contact lens for the management of extreme irregularity in a thin cornea after unsuccessful excimer laser refractive surgery. Eye Contact Lens. 2014;40(3):e16-20. 8. Shorter E, Fogt J, Nau C, et al. Prescription habits of scleral lenses for the management of corneal irregularity and ocular surface disease among scleral lens practitioners. Eye Contact Lens. 2023;49(2):46-50. 9. Nau A, Shorter ES, Harthan JS, et al. Multicenter review of impression-based scleral devices. Cont Lens Anterior Eye. 2021;44(5):101380. 10. Silverman JIM, Huffman JM, Zimmerman MB, et al. Indications for wear, visual outcomes and complications of custom imprint 3D scanned scleral contact lens use. Cornea. 2021;40(5):596-602. |


