 |
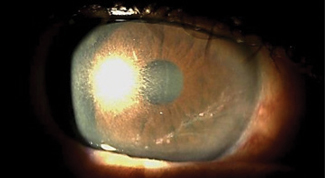
| Heparanase blockers could provide a potential treatment for corneal herpetic dendrites. Photo: Bhawan Minhas, OD |
Enzyme Behind HSV-1 Inflammation Identified
In a recent study, researchers at the University of Illinois at Chicago identified the chief molecule responsible for herpes simplex virus-1 (HSV-1) infection-related corneal inflammation.1 According to the findings, heparanase, a corneal enzyme that degrades heparan sulfate, becomes significantly upregulated during an HSV-1 infection. As a result, the enzyme triggers inflammation, lasting even after the infection has cleared.“I think it’s easy for clinicians to forget that there are long-lasting complications of herpetic eye disease that last after the initial infection has cleared up,” says Bhawan Minhas, OD, assistant professor and director of on-campus residency programs at the Pennsylvania College of Optometry. “Sometimes they deal with the presenting infection successfully through antivirals and steroids but fail to consider the inflammatory cascade initiated by the event that requires more follow-up and management to prevent opacities and neovascularization of the cornea leading to further decrease in vision.”
Heparanase is normally active in the cornea, but only in low levels. In past studies, it was evaluated for its role as a cancer regulator. Here, however, researchers found that high levels of heparanase damaged cell junctions in the cornea and stimulated production of pro-inflammatory molecules, leading to inflammation.
According to Dr. Minhas, this means practitioners may need to consider keeping patients on a topical steroid for an extended period to inhibit sequelae of post-infection inflammation. “Ideally, a drug that specifically targets heparanase could be used as an adjunct well after antivirals and steroids are stopped,” she adds. Results from the study show that use of OGT 2115, a heparanase blocker, causes corneal lesions to heal quickly, while lesions not treated with OGT 2115 did not heal. As researchers believe this could lead to a new treatment option for HSV-1, Dr. Minhas wonders whether any drug companies have taken notice, and what possible side effects could be associated with heparanase blockers.
One important area for future studies to address is the effect of heparanase on other inflammatory ocular conditions. “I would like to see how this can be linked to other conditions that have similar issues with disruption of immune privilege of the cornea that cause scarring and ultimately further deterioration of vision,” says Dr. Minhas.
1. Agelidis AM, Hadigal SR, Jaishankar D, Shukla D. Viral Activation of Heparanase Drives Pathogenesis of Herpes Simplex Virus-1. Cell Reports. 2017;20(2):439-50.
In BriefPatients with persistent epithelial defect after bacterial keratitis who did not have success with topical fortified antibiotics may have a new treatment option with a matrix regenerating agent (RGTA), according to new research. In a case series of 14 patients, investigators found 78.6% achieved complete corneal healing after one drop of RGTA every other day for a month. After three months, 100% of study participants had complete corneal healing. Chappelet MA, Bernheim D, Chiquet C, Aptel F. Effect of a new matrix therapy agent in persistent epithelial defects after bacterial keratitis treated with topical fortified antibiotics. Cornea. 2017;36(9):1061-8. After evaluating 100 consecutive eyes undergoing SMILE refractive surgery at a tertiary care ophthalmic center, researchers found the learning curve of SMILE can be challenging. For the initial 100 eyes, surgeons experienced intraoperative difficulties such as suction loss, black spots, opaque bubble layer, epithelial defect and difficult lenticule extraction. The researchers note lenticule dissection and extraction is the most challenging step, and complications dropped from 16% in the first 50 cases to 2% in the next 50 cases. They found most complications led to delayed visual recovery in the first 50 cases. Titiyal JS, Manpreet Kaur M, Anubha Rathi A, et al. Learning curve of small incision lenticule extraction: challenges and complications. Cornea. August 9, 2017. [Epub]. Inflammation may cause end-of-day discomfort in contact lens wearers, according to a recent study. After evaluating the concentration of certain proteins and inflammatory mediators in the tears of both symptomatic and asymptomatic contact lens wearers, researchers found that leukotriene B4 (LTB4) levels were significantly higher in symptomatic patients. No other compounds showed significant differences between the two groups, leading researchers to conclude that LTB4 may play a role in contact lens discomfort and could be a target for therapy. Masoudi S, Stapleton FJ, Willcox MDP. Differences in tear film biochemistry of symptomatic and asymptomatic lens wearers. Optom Vis Sci. 2017;94. [Epub ahead of print]. |


