 When not managed appropriately, underlying ocular surface disease can erode a contact lens practice relatively quickly. The tear film is a delicate yet sophisticated structure that is composed of a mucin, aqueous and lipid layer. It is the dynamic interaction between these three layers that will either protect the ocular surface or allow it to be compromised, which can lead to clinical sequelae. When contact lenses come into play, this presents an additional obstacle in maintaining a robust tear film.
When not managed appropriately, underlying ocular surface disease can erode a contact lens practice relatively quickly. The tear film is a delicate yet sophisticated structure that is composed of a mucin, aqueous and lipid layer. It is the dynamic interaction between these three layers that will either protect the ocular surface or allow it to be compromised, which can lead to clinical sequelae. When contact lenses come into play, this presents an additional obstacle in maintaining a robust tear film.
Evolution of Dry Eye Treatment
Over the past decade, our knowledge of dry eye disease has improved significantly. Traditionally, we have thought of dry eye disease as either an aqueous deficiency stemming from poor aqueous production or evaporative resulting from a poor lipid layer produced by the meibomian glands. We now know that dry eye patients also have increased osmolarity and inflammation of the ocular surface. These findings have evolved treatment protocols for dry eye patients.1,2
Punctal occlusion is a procedure that helps retain tears on the ocular surface. We know anecdotally that some patients respond favorably after punctal occlusion is performed, reporting that their eye feels “more comfortable,” while others respond with increased dry eye symptoms. We have learned that those patients who respond poorly are likely to have a certain level of inflammation which is retained on the ocular surface. These inflammatory factors will then exacerbate signs and symptoms that escalate with punctal occlusion.
The logical course for treating patients with dry eye is to decrease the inflammatory component and, once the inflammation has been resolved, to implement punctal occlusion—this will retain tears with fewer inflammatory components. This is typically accomplished by initiating therapy with a mild steroid (loteprednol 0.5%) q.i.d. for two to four weeks, followed by b.i.d. dosing for two weeks. The drop is then stopped and replaced with artificial tear therapy or cyclosporine 0.05% b.i.d. O.U. For some patients, we will begin both therapies and then taper off the steroid while maintaining patients on cyclosporine 0.05% b.i.d. for long-term therapy.
Another key factor is eyelid margin inflammation. Altered meibomian gland secretions can cause harm to the tear film by compromising its lipid layer. Eyelid hygiene, along with warm compresses, will often thin meibomian gland secretions. Topical antibiotics or antibiotic/steroid combinations can be used to further decrease eyelid inflammation. Omega 3 fatty acids have been shown to be effective in thinning meibum and promoting healthy meibum production. Additionally, oral doxycycline can supplement eyelid therapy and further reduce inflammation.
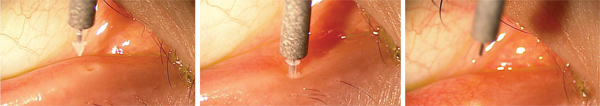
Insertion of a silicone punctal plug in a contact lens wearer with dry eyes.
Once inflammation has been sequestered, punctal occlusion is a logical treatment option to retain a healthier tear film on the ocular surface. One study looked at dry eye treatment effectiveness, comparing three different treatment regimens: using cyclosporine 0.05% b.i.d. O.U., punctal occlusion of the inferior punctum O.U. and a combination of punctal occlusion and cyclosporine. The researchers assessed tear volume, ocular surface staining and artificial tear use at baseline and at one, three and six months. Although all three treatment groups were effective in treating dry eye, combination therapy showed the greatest overall improvement and was superior to either individual treatment.3
In another study, dry eye and non-dry eye patients’ upper and lower puncta were occluded. Tear meniscus volume was analyzed using optical coherence tomography (OCT). Results from the study showed that both the upper and lower tear meniscus volume in dry eye patients increased significantly (when both puncta were occluded). Interestingly, the control group did not show a statistically significant difference in tear meniscus volume—a likely indication that the presence of an autoregulatory mechanism maintains the volume of tears even in the presence of altered tear clearance via punctal occlusion.4
Punctal Occlusion and Contact Lenses
We are fortunate to have a wide array of highly sophisticated designs and materials of lens options in our armamentarium. We are equally appreciative of the modern contact lens care systems and their ability to retain moisture on the surface of a contact lens. But, when contact lens and care systems have been optimized and a patient’s wearing experience continues to be compromised, treating the underlying ocular surface disease may improve lens wear.
Twenty-five patients who complained of decreased contact lens wear were recruited for a study. Researchers placed a silicone plug in the lower punctum of one eye and conducted a “sham procedure” on the other eye by pretending to insert a punctal plug, so that the patient didn’t know which eye had the plug. Three weeks following plug placement, 18 of the 25 subjects reported a 34.6% increase in comfortable contact lens wearing time in the punctal plug eye, three reported no difference and four reported intolerable plug related discomfort.5 This study shows that punctal occlusion has a place in managing contact lens comfort issues.
In another study, patients complaining of dry eye were randomized into two groups: both lower puncta occluded or no punctal occlusion (but the patients went through a sham procedure where the lower puncta were manipulated as if being occluded). At the follow up visit six weeks later, dry eye questionnaires were again administered. Surprisingly, both the treatment and control groups showed an increase in dry eye questionnaire scores, but no significant difference existed between the two groups.6 In this study, dry eye questionnaires were used as the entry criteria but objective findings were not. This illustrates the importance that both subjective (as taken in the study) and objective findings may have in determining whether to perform punctal occlusion.
Punctal occlusion continues to play a significant role in our practices, and when performed in a timely manner, can deliver great relief to both our non-contact lens and contact lens wearing patients.
A Case in Point
“Joan,” a 40-year-old female patient presented complaining of consistent red eyes and discomfort with contact lens wear. She works in a hospital and has had consistent dry eyes in the past. She denied taking any medications and has reported that her symptoms are significantly worse while she is at the hospital. She has tried various contact lenses and has been treated with multiple dry eye therapies, including prescription and non-prescription eye drops, with little to no relief. She has considered LASIK due to her inability to wear contact lenses after these unsuccessful treatment plans. I discussed the possibility of punctal plugs and outlined the process involved with inserting them. After Joan agreed to move forward with this procedure, I inserted the Parasol silicone plugs, Odyssey (refer to picture). When she returned for her follow-up appointment 10 days later, she was content with her ability to wear contact lenses again. Six months later, Joan continues to wear her contact lenses comfortably.
To view the different types of punctal plugs and visit the manufacturer’s website, please visit
www.dryeyeyellowpages.com/products/categories/plugs.html.
1. The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007 Apr;5(2):75-92.
2. Jackson WB. Management of dysfunctional tear syndrome: a Canadian consensus. Can J Ophthalmol. 2009 Aug;44(4):385-94.
3. Roberts CW, Carniglia PE, Brazzo BG. Comparison of topical cyclosporine, punctal occlusion, and a combination for the treatment of dry eye. Cornea. 2007 Aug;26(7):805-9.
4. Chen F, Shen M, Chen W, et al. Tear meniscus volume in dry eye after punctal occlusion. Invest Ophthalmol Vis Sci. 2010 Apr;51(4):1965-9.
5. Giovagnoli D, Graham SJ. Inferior punctal occlusion with removable silicone punctal plugs in the treatment of dry-eye related contact lens discomfort. J Am Optom Assoc. 1992 Jul;63(7):481-5.
6. Geldis JR, Nichols JJ. The impact of punctal occlusion on soft contact lens wearing comfort and the tear film. Eye Contact Lens. 2008 Sep;34(5):261-5.


