Herpes simplex virus (HSV) is an enveloped, linear, double-stranded DNA virus belonging to the Alphaherpesvirinae family, made up of HSV type 1 (HSV-1), HSV type 2 (HSV-2) and varicella zoster virus (VZV); in this article, we will focus on the first two.1 HSV keratitis is thought to be a leading cause of blindness in developed nations.2 Diagnosis can be challenging, as the virus can present with a wide range of signs and symptoms. Here, we aim to educate clinicians on the varying clinical presentations and available treatment options to help our patients achieve ideal outcomes.
HSV Keratitis
Worldwide, 4.58 billion people (67% of the population) are infected with HSV-1, while 836 million people over age 15 are infected with HSV-2.3 The global incidence of HSV-1 in 2016 was 2.1%, and the incidence of HSV keratitis was 24.0 per 100,000 persons.1,4 In the United States, the prevalence of HSV-1 for people between the ages of 14 to 49 is 47.8%, though it has decreased by 11.3% since 2000.2 It is estimated that nearly 500,000 people in the US have a history of ocular HSV.1
Prevalence in the US increases with age, is higher in women and is most common among Mexican-American persons.2 Improved hygiene practices have contributed to the decline in prevalence by reducing or delaying the risk of exposure, though the latter may lead to more severe illness later in life.1
HSV commonly infects the mouth, genitalia and eyes. The virus is spread through direct contact with an infected lesion or secretion as the virus enters the mucous membrane of the host.5 HSV-1 has a greater association with ocular pathology and HSV-2 is more likely to cause genital infection, but both can infect either location.6 Once an individual has been infected, the incubation period ranges from one to 28 days. HSV is infectious during asymptomatic shedding and during the five- to 10-day healing process for skin/mucous membrane lesions if they are present.6 After the primary infection, the virus travels along the sensory nerves via retrograde axonal transport to the trigeminal ganglion where it will remain latent until reactivation.1 Reactivation can be triggered by fever, hormonal changes, ocular trauma, ultraviolet exposure and stress.6,7 Reactivation of ocular HSV can cause blepharitis, conjunctivitis, keratitis, uveitis and acute retinal necrosis.
Typically, ocular HSV is diagnosed clinically on slit lamp examination, but diagnostic testing is available including polymerase chain reaction, enzyme-linked immunosorbent assay, viral cultures, immunofluorescence antibody assay and western blot.8,9 Western blot has high sensitivity and specificity but is not easily accessible.9
HSV keratitis typically presents unilaterally, though bilateral infections can occur in immunocompromised individuals and make up <12% of cases.8 Presenting symptoms are often vague and include redness, photophobia, discharge, watery eyes, irritation, itching, pain and blurry vision. Therefore, to make an accurate diagnosis, we must rely on clinical signs that vary based on the corneal layer affected (epithelium, stroma or endothelium).8,10 Below, we’ll discuss how HSV keratitis manifests in each of these three layers.
Epithelial Keratitis
 |
|
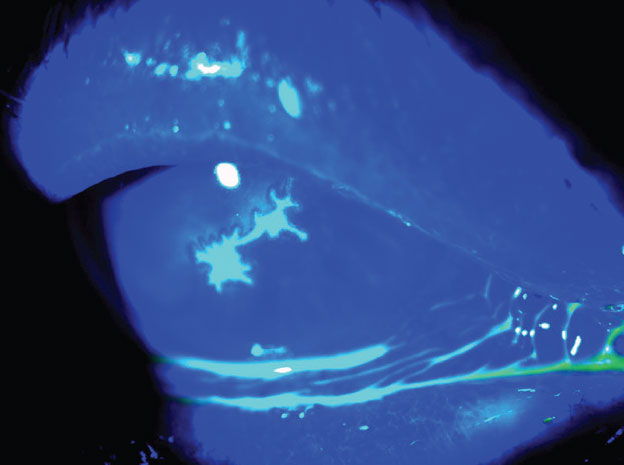
Fig. 1. Typical HSV keratitis epithelial dendrite with terminal bulbs. Click image to enlarge. |
HSV epithelial keratitis is the most common subclassification and first appears as coarse granular epithelial spots that form punctate lesions. The punctate lesions coalesce to form the most common presentation of HSV epithelial keratitis, a dendritic keratitis.8,11 HSV dendrites present as white, linear, branching corneal dendrites with terminal end bulbs (Figure 1).8,10,12 Using vital dyes is necessary to differentiate HSV epithelial keratitis from other corneal epithelial diseases.
HSV dendrites are true corneal ulcers that stain with fluorescein at the base of the ulcer. The swollen, inflamed epithelial cells that surround the base of the ulcer stain with lissamine green or rose bengal.8,10 As HSV dendritic ulcers heal, subepithelial haze or ghost dendrites may remain, which lack fluorescein staining.10 Following resolution of HSV epithelial keratitis, corneal nerve degeneration, decreased corneal sensation, stromal inflammation and/or corneal scarring can persist.10,13
Stromal Keratitis
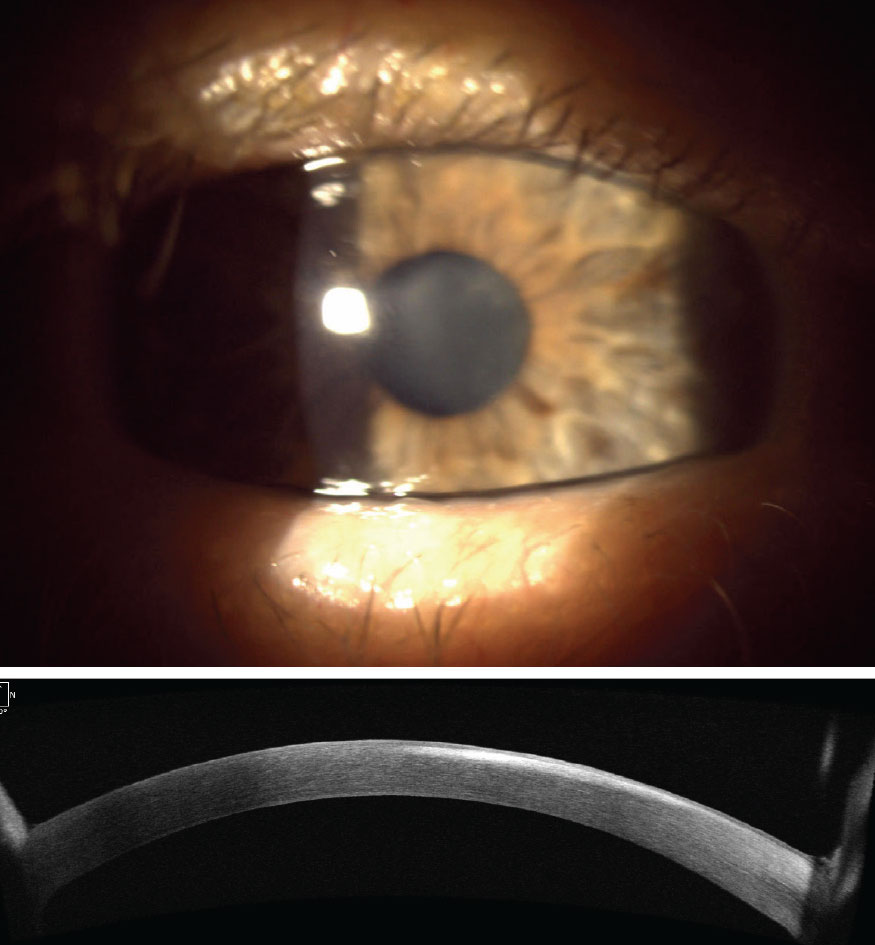
Patients with HSV stromal keratitis or interstitial keratitis often have chronic, recurrent inflammation that worsens with each subsequent episode, resulting from retained corneal viral antigens that trigger an antigen-antibody complement cascade.1,8,10,14 HSV stromal keratitis results from infectious epithelial keratitis or endotheliitis (Figure 2).1,8,10 Clinical manifestations of HSV stromal keratitis include unifocal, multifocal or diffuse stromal infiltrates, stromal edema, an immune ring, corneal thinning and sectoral or diffuse stromal neovascularization.10,15,16 HSV disease may also present as posterior interstitial keratitis as reported in a case series of five patients.15
 |
|
Fig. 2. Same patient from Figure 1 whose epithelial disease resolved with oral antivirals but progressed to stromal keratitis. Top photo shows central stromal haze which corresponds to hyperreflectivity on anterior segment OCT (bottom photo). Click image to enlarge. |
HSV stromal keratitis may be non-necrotizing or necrotizing in clinical presentation. Non-necrotizing HSV stromal keratitis clinically presents with corneal edema and is often self-limiting. Necrotizing HSV stromal keratitis is rapidly progressive with stromal infiltrates, diffuse inflammation, ulceration and is less responsive to therapy, with corneal perforation possible.8,10 Both forms of HSV stromal keratitis can be recalcitrant or resistant, leading to vision loss from corneal neovascularization and scarring.1,10,12,17
Endothelial Keratitis
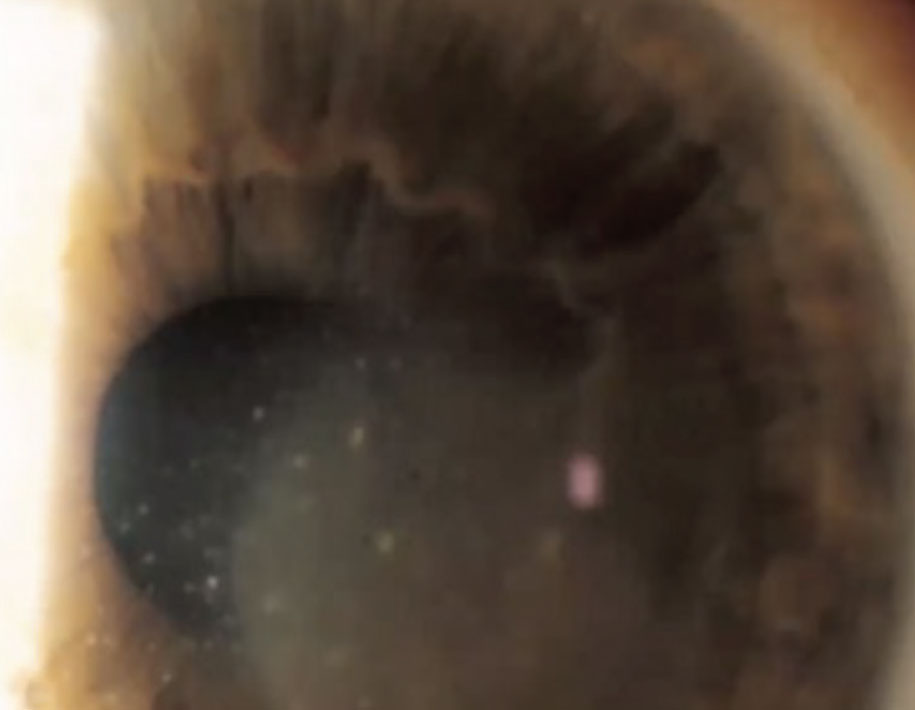
The clinical presentation of HSV endothelial keratitis will reveal keratitis precipitates, iritis and stromal edema without neovascularization in a disciform, diffuse or linear pattern (Figure 3).8,14 HSV endothelial keratitis, or endotheliitis, is thought to be caused by an active virus in the anterior chamber and can represent an infectious or inflammatory HSV process.10
 |
|
Fig. 3. Stromal haze centrally with keratic precipitation indicative of HSV endothelial keratitis. Click image to enlarge. |
Disciform endothelial keratitis will have a central focal circular area of stromal edema with keratic precipitates and anterior uveitis; it’s also the most common presentation.10 Less common is diffuse endothelial keratitis, which presents as keratic precipitates throughout the entire cornea. Linear endotheliitis is usually the most difficult to treat and will clinically show a distinct linear distribution of keratic precipitates progressing from the limbus, demarcating the involved edematous cornea from the noninvolved cornea.10,18,19 Any anterior uveitis with high intraocular pressure should be concerning for possible HSV.
Neurotrophic Keratopathy (NK)
This degenerative corneal disease may result from prior episodes of HSV keratitis due to damage to the ophthalmic branch of the trigeminal nerve.10,20 Diagnosis of NK is based on clinical history, examination and corneal sensitivity testing and can be classified using the Mackie severity scale or the Neurotrophic Keratopathy Study Group Classification.20-23 Using the Mackie grading system, stage 1 (mild NK) includes corneal epithelial changes; stage 2 (moderate NK) is classified by a corneal epithelial defect; and stage 3 (severe NK) is often characterized by corneal ulceration, perforation and melting.22,24 Diagnosis of NK can be delayed due to the reduction in corneal sensitivity and, if left untreated, can result in permanent vision loss.20,25 NK management is targeted to the severity of clinical presentation.21
 |
|
Fig. 4. Mild epithelial defects can be appreciated here in an atypical fashion. Click image to enlarge. |
Treatment and Management
As alluded to earlier, HSV keratitis presentation is unique depending on which corneal layer(s) are affected. Once an accurate diagnosis has been made, clinicians have multiple treatment and management options to consider. Below are some evidence-based recommendations.
HSV epithelial keratitis. Two routes of administration are available for clinicians in their management of HSV epithelial keratitis, topical or oral antiviral medications. Although the thought of combining both oral and topical medications in hopes of achieving faster and better outcomes is enticing, the Herpetic Eye Disease Study (HEDS) showed no benefits in this approach.26,27 Therefore, clinicians should choose one route of administration based on the clinical situation and presentation.
Two topical antivirals (trifluridine solution and ganciclovir gel) and three oral antivirals (acyclovir, famciclovir and valacyclovir) can be used for HSV epithelial keratitis treatment.27,28 While topical trifluridine is available as a generic ophthalmic solution, we have found that it can be difficult for patients to acquire once prescribed.
Trifluridine is administered at one drop in the affected eye(s) nine times. This excessive dosing schedule along with the presence of thimerosal, a known toxic preservative, can lead to potential corneal toxicity that delays the resolution of keratitis.29-31 A more convenient option exists with ganciclovir gel, which is administered five times daily until resolution of the keratitis followed by a taper to three times daily for seven days.32,33 Although both options result in favorable outcomes, ganciclovir may be the preferred choice to trifluridine in certain situations. This applies to patients who cannot instill drops every two hours, those with slow-healing ulcers (trifluridine treatment is restricted to 21 days) and patients under six years old, as trifluridine is only recommended for children older than this age.27
Another approach is oral antivirals, which manage HSV epithelial keratitis relatively safely and effectively.27,34 Dosing depends on the degree of epithelial involvement. HSV epithelial keratitis that is more dendritic in appearance can be managed with a seven- to 10-day course of either acyclovir (400mg five times daily), valacyclovir (500mg three times daily) or famciclovir 250mg (three times daily). If the epithelial keratitis is larger or more geographic, dosing can be extended to 14 to 21 days with the following increase in antiviral strength: acyclovir (800mg five times daily) valacyclovir (1g three times daily) or famciclovir (500mg three times daily).27,35,36
While all three agents are safe in most patients, clinicians should remain cautious when prescribing to patients with known kidney disease or those older than 65, as all three have the potential to cause nephrotoxicity, hallucinations, confusion and agitation.37 Famciclovir is preferred over acyclovir and valacyclovir in elderly patients with or without reduced renal function.27,38 Consultation with the patient’s PCP or nephrologist is strongly suggested before prescribing in such situations. Dosages can also be adjusted based on a patient’s renal clearance.
Oral antivirals are often favored over topical antivirals due to their more manageable dosing schedule and lower cost. They are also advantageous for patients who are unable to administer drops or gels, do not respond to topical treatments or have preexisting ocular surface disease.27,39
HSV stromal keratitis without epithelial ulceration. Due to a large inflammatory response caused by the HSV virus in the stroma, the HEDS Group advised the use of topical steroid therapy in combination with oral antivirals as the mainstay of treatment.40 A tapered course of topical steroids for more than 10 weeks is suggested, as discontinuation at an earlier stage results in a higher chance of treatment failure.26 At all times of steroid treatment, the patient should be taking concurrent prophylactic oral antiviral treatment with either acyclovir (400mg two times daily), valacyclovir (500mg daily) or famciclovir (250mg two times daily, or higher doses if indicated). Recommended dosing of topical steroids is prednisolone 1% six to eight times daily, tapered over a time greater than 10 weeks.27 The ultimate time of the taper period will be determined by the patient’s clinical response and appearance of the cornea.27
Topical antiviral agents have no role in the treatment of HSV stromal keratitis. Both agents do not adequately penetrate to the corneal stroma when compared to oral antivirals. In addition, they are not indicated for an extended period of treatment time, nor do they address the underlying inflammation.41,42
HSV stromal keratitis with epithelial ulceration. As it is rarely encountered, no set treatment protocol has been determined due to the lack of evidence-based clinical studies.26,40 The American Academy of Ophthalmology Treatment Guidelines suggests a limited dose of prednisolone 1% (twice daily) plus a therapeutic dose of an oral antiviral for seven to 10 days (one of the following, dosed three to five times daily: acyclovir 800mg, valacyclovir 1g or famciclovir 500mg).27 The oral antiviral can then be reduced to the previously mentioned prophylactic doses with slow taper of the topical prednisolone. Unfortunately, there are no recommendations for the length of treatment.
HSV endothelial keratitis. An uncommon form of HSV keratitis, endothelial keratitis usually presents independent of other forms of HSV keratitis.27,43 As the inflammation in these cases is further posterior in the cornea, topical trifluridine and ganciclovir again have no role in treatment as they cannot achieve adequate corneal penetration. An oral antiviral agent is therefore needed for corneal penetration.44. Due to the degree of inflammation seen, anti-inflammatory therapy is indicated. The literature has shown the effectiveness of a combination of a topical steroid in conjunction with an oral antiviral.36,44 This combination approach leads to healing times between 21 to 25 days.45,46 Recommended treatment consists of prednisolone acetate 1% every hour or every other hour plus a therapeutic dose of one of the three antivirals. The steroid can be tapered based on the clinical response, while the oral antiviral can be reduced to a prophylactic dose. The length of treatment will again vary between patients.27
Clinicians should also be cognizant of prescribing additional treatments including cycloplegic agents to stabilize the blood-aqueous barrier and to immobilize the iris for pain management.47 With any steroid treatment, intraocular pressure should be monitored for any potential spikes and be managed appropriately with intraocular pressure drops including beta blockers and alpha agonists.48 Classic teaching states that prostaglandin analogs should be avoided due to their potential links to HSV activation.27,49 However, this is based on anecdotal case reports or papers based on rabbit models. A larger study found the prevalence of ocular herpes in those using latanoprost (0.11%) to be similar to the general population (0.15%).50
Reoccurrences: Don’t Call it a Comeback
Even with prompt and effective treatment, the possibility of recurrence exists in patients with HSV keratitis. As the condition can lead to significant corneal scarring and vision loss, especially in cases of HSV stromal keratitis, clinicians should consider prophylactic or maintenance doses of oral antivirals for their patients.27
The HEDS Group examined patients who had an ocular HSV episode in the previous year. Specifically, they looked at the effects of oral acyclovir (400mg twice daily) vs. placebo in preventing ocular HSV recurrences in patients with a history of ocular HSV.51 The findings indicated that during the 12-month treatment period, the incidence of HSV keratitis recurrences was reduced by half in patients receiving oral acyclovir compared to the placebo group. Additionally, the researchers observed that the protective effect of acyclovir ceased once the medication was discontinued.51,52
Importantly, patients who benefited most from prophylactic treatment in HEDS included those with a history of HSV stromal keratitis and those who have experienced multiple episodes of other types of HSV keratitis (epithelial or endothelial).51,52 Additionally, clinicians might consider using valacyclovir 500mg daily for prophylaxis, as it has proven to be as effective as acyclovir in preventing recurrences.53 Another alternative could be famciclovir 250mg taken twice daily, which can be used instead of acyclovir or valacyclovir.54
Remember that before beginning any prophylaxis treatment, appropriate communication with a patient’s primary physician and other medical specialists is recommended. Renal function should be checked regularly (every six months) with prolonged use of any oral antiviral.
Takeaways
HSV is one of the most ubiquitous infections clinicians will encounter, capable of affecting any or all layers of the cornea. Through a comprehensive corneal examination, clinicians can determine what type of HSV keratitis they are dealing with and initiate prompt and appropriate treatment to achieve ideal visual outcomes.
Dr. Bhakhri is an associate professor at Illinois College of Optometry (ICO) where he coordinates the ocular pharmacology and advanced retina courses. He is a fellow of the American Academy of Optometry (AAO) and the Optometric Retina Society and is on the advisory board for Regeneron Pharmaceuticals.
Dr. Harthan is a professor at ICO and chief of the Cornea and Contact Lens Center for Clinical Excellence at the Illinois Eye Institute. She is a fellow of the AAO, a diplomate of the Section on Cornea, Contact Lenses and Refractive Technologies, a fellow of the Scleral Lens Education Society and serves on the advisory board for GP Lens Institute and International Keratoconus Academy. She is also a founding member of the SCOPE (Scleral Lenses in Current Ophthalmic Practice Evaluation) research team.
Dr. Skoog is an assistant professor at ICO in the cornea and contact lens department, where he previously completed a residency. He lectures on anterior segment disease and contact lenses.
1. Farooq AV, Shukla D. Herpes simplex epithelial and stromal keratitis: an epidemiologic update. Surv Ophthalmol. 2012;57(5):448-62. 2. McQuillan G, Kruszon-Moran D, Flagg EW, Paulose-Ram R. Prevalence of herpes simplex virus type 1 and type 2 in persons aged 14-49: United States, 2015-2016. NCHS Data Brief. 2018;(304):1-8. 3. James C, Harfouche M, Welton NJ, et al. Herpes simplex virus: global infection prevalence and incidence estimates, 2016. Bull World Health Organ. 2020;98(5):315-29. 4. McCormick I, James C, Welton NJ, et al. Incidence of herpes simplex virus keratitis and other ocular disease: global review and estimates. Ophthalmic Epidemiol. 2022;29(4):353-62. 5. Akhtar J, Tiwari V, Oh MJ, et al. HVEM and nectin-1 are the major mediators of herpes simplex virus 1 (HSV-1) entry into human conjunctival epithelium. Invest Ophthalmol Vis Sci. 2008;49(9):4026-35. 6. Liesegang TJ. Herpes simplex virus epidemiology and ocular importance. Cornea. 2001;20(1):1-13. 7. Suzich JB, Cliffe AR. Strength in diversity: understanding the pathways to herpes simplex virus reactivation. Virology. 2018;522:81-91. 8. Azher TN, Yin XT, Tajfirouz D, Huang AJ, Stuart PM. Herpes simplex keratitis: challenges in diagnosis and clinical management. Clin Ophthalmol. 2017;11:185-91. 9. Crawford Katharine HD, Selke S, Pepper G, et al. Performance characteristics of highly automated HSV-1 and HSV-2 IgG testing. J Clin Microbiol. 2024;62(6):e00263-24. 10. Valerio GS, Lin CC. Ocular manifestations of herpes simplex virus. Curr Opin Ophthalmol. 2019;30(6):525-31. 11. Green LK, Pavan-Langston D. Herpes simplex ocular inflammatory disease. Int Ophthalmol Clin. 2006;46(2):27-37. 12. Sibley D, Larkin DFP. Update on herpes simplex keratitis management. Eye (Lond). 2020;34(12):2219-26. 13. Gallar J, Tervo TM, Neira W, et al. Selective changes in human corneal sensation associated with herpes simplex virus keratitis. Invest Ophthalmol Vis Sci. 2010;51(9):4516-22. 14. Kaye S, Choudhary A. Herpes simplex keratitis. Prog Retin Eye Res. 2006;25(4):355-80. 15. Farooq AV, Paley GL, Lubniewski AJ, Gonzales JA, Margolis TP. Unilateral posterior interstitial keratitis as a clinical presentation of herpes simplex virus disease. Cornea. 2018;37(3):375-8. 16. Holland EJ, Schwartz GS. Classification of herpes simplex virus keratitis. Cornea. 1999;18(2):144-54. 17. Mott KR, Bresee CJ, Allen SJ, BenMohamed L, Wechsler SL, Ghiasi H. Level of herpes simplex virus type 1 latency correlates with severity of corneal scarring and exhaustion of CD8+ T cells in trigeminal ganglia of latently infected mice. J Virol. 2009;83(5):2246-54. 18. Shen YC, Wang CY, Chen YC, Lee YF. Progressive herpetic linear endotheliitis. Cornea. 2007;26(3):365-7. 19. Shin J, Ra H, Rho CR. Herpes simplex virus linear endotheliitis in a post-keratoplasty patient: a case report. Medicine (Baltimore). 2019;98(3):e14191. 20. Dana R, Farid M, Gupta PK, et al. Expert consensus on the identification, diagnosis, and treatment of neurotrophic keratopathy. BMC Ophthalmol. 2021;21(1):327. 21. Dua HS, Said DG, Messmer EM, et al. Neurotrophic keratopathy. Prog Retin Eye Res. 2018;66:107-31. 22. Mackie IA. Neuroparalytic keratitis. In: Fraunfelder FRF, Meyer SM, eds. Current ocular therapy. Philadelphia, PA, USA: WB Saunders; 1995. 23. Cheung AY, Holland EJ, Lee WB, et al. Neurotrophic keratopathy: an updated understanding. The Ocular Surface. 2023;30:129-38. 24. Mastropasqua L, Nubile M, Lanzini M, Calienno R, Dua HS. In vivo microscopic and optical coherence tomography classification of neurotrophic keratopathy. J Cell Physiol. 2019;234(5):6108-15. 25. Versura P, Giannaccare G, Pellegrini M, Sebastiani S, Campos EC. Neurotrophic keratitis: current challenges and future prospects. Eye Brain. 2018;10:37-45. 26. Barron BA, Gee L, Hauck WW, et al. Herpetic eye disease study. A controlled trial of oral acyclovir for herpes simplex stromal keratitis. Ophthalmology. 1994;101(12):1871-82. 27. White ML CJ. Herpes simplex virus keratitis: a treatment guideline - 2014. American Academy of Ophthalmology. Updated June 27, 2014. 28. A controlled trial of oral acyclovir for iridocyclitis caused by herpes simplex virus. The Herpetic Eye Disease Study Group. Arch Ophthalmol. 1996;114(9):1065-72. 29. Høvding G. A comparison between acyclovir and trifluorothymidine ophthalmic ointment in the treatment of epithelial dendritic keratitis. A double blind, randomized parallel group trial. Acta Ophthalmol (Copenh). 1989;67(1):51-4. 30. la Lau C, Oosterhuis JA, Versteeg J, et al. Acyclovir and trifluorothymidine in herpetic keratitis: a multicentre trial. Br J Ophthalmol. 1982;66(8):506-8. 31. Wellings PC, Awdry PN, Bors FH, Jones BR, Brown DC, Kaufman HE. Clinical evaluation of trifluorothymidine in the treatment of herpes simplex corneal ulcers. Am J Ophthalmol. 1972;73(6):932-42. 32. Chou TY, Hong BY. Ganciclovir ophthalmic gel 0.15% for the treatment of acute herpetic keratitis: background, effectiveness, tolerability, safety, and future applications. Ther Clin Risk Manag. 2014;10:665-81. 33. Sahin A, Hamrah P. Acute herpetic keratitis: what is the role for ganciclovir ophthalmic gel? Ophthalmol Eye Dis. 2012;4:23-34. 34. Chen F, Xu H, Liu J, et al. Efficacy and safety of nucleoside antiviral drugs for treatment of recurrent herpes labialis: a systematic review and meta-analysis. J Oral Pathol Med. 2017;46(8):561-8. 35. Collum LM, McGettrick P, Akhtar J, Lavin J, Rees PJ. Oral acyclovir (Zovirax) in herpes simplex dendritic corneal ulceration. Br J Ophthalmol. 1986;70(6):435-8. 36. Ahmad B, Gurnani B, Patel BC. Herpes simplex keratitis. StatPearls. StatPearls Publishing LLC.; 2024. 37. Murakami T, Akimoto T, Okada M, et al. Valacyclovir neurotoxicity and nephrotoxicity in an elderly patient complicated by hyponatremia. Drug Target Insights. 2018. 38. Brandariz-Nuñez D, Correas-Sanahuja M, Maya-Gallego S, Martín Herranz I. Neurotoxicity associated with acyclovir and valacyclovir: a systematic review of cases. J Clin Pharm Ther. 2021;46(4):918-26. 39. Cernik C, Gallina K, Brodell RT. The treatment of herpes simplex infections: an evidence-based review. Arch Intern Med. 2008;168(11):1137-44. 40. Wilhelmus KR, Gee L, Hauck WW, et al. Herpetic eye disease study. A controlled trial of topical corticosteroids for herpes simplex stromal keratitis. Ophthalmology. 1994;101(12):1883-95; discussion 1895-6. 41. Castela N, Vermerie N, Chast F, et al. Ganciclovir ophthalmic gel in herpes simplex virus rabbit keratitis: intraocular penetration and efficacy. J Ocul Pharmacol. 1994;10(2):439-51. 42. Poirier RH, Kingham JD, de Miranda P, Annel M. Intraocular antiviral penetration. Arch Ophthalmol. 1982;100(12):1964-7. 43. Inoue Y. Review of clinical and basic approaches to corneal endotheliitis. Cornea. 2014;33 Suppl 11:S3-8. 44. Porter SM, Patterson A, Kho P. A comparison of local and systemic acyclovir in the management of herpetic disciform keratitis. Br J Ophthalmol. 1990;74(5):283-5. 45. Collum LM, Logan P, Ravenscroft T. Acyclovir (Zovirax) in herpetic disciform keratitis. Br J Ophthalmol. 1983;67(2):115-8. 46. Collum LM, Grant DM. A double-blind comparative trial of acyclovir and adenine arabinoside in combination with dilute betamethasone in the management of herpetic disciform keratitis. Curr Eye Res. 1987;6(1):221-4. 47. Agrawal RV, Murthy S, Sangwan V, Biswas J. Current approach in diagnosis and management of anterior uveitis. Indian J Ophthalmol. 2010;58(1):11-9. 48. Phulke S, Kaushik S, Kaur S, Pandav SS. Steroid-induced glaucoma: an avoidable irreversible blindness. J Curr Glaucoma Pract. 2017;11(2):67-72. 49. Dvivedi A, Murthy SI, Garudadri C, Sheba E, Sharma S. Bilateral severe herpes simplex endotheliitis with a possible association with latanoprost. Ocul Immunol Inflamm. 2023;31(5):1073-5. 50. Bean G, Reardon G, Zimmerman TJ. Association between ocular herpes simplex virus and topical ocular hypotensive therapy. J Glaucoma. 2004;13(5):361-4. 51. Herpetic Eye Disease Study G. Oral acyclovir for herpes simplex virus eye disease: effect on prevention of epithelial keratitis and stromal keratitis. Arch Ophthalmol. 2000;118(8):1030-6. 52. Acyclovir for the prevention of recurrent herpes simplex virus eye disease. Herpetic Eye Disease Study Group. N Engl J Med. 1998;339(5):300-6. 53. Miserocchi E, Modorati G, Galli L, Rama P. Efficacy of valacyclovir vs acyclovir for the prevention of recurrent herpes simplex virus eye disease: a pilot study. Am J Ophthalmol. 2007;144(4):547-51.e1. 54. Chong DY, Johnson MW, Huynh TH, Hall EF, Comer GM, Fish DN. Vitreous penetration of orally administered famciclovir. Am J Ophthalmol. 2009;148(1):38-42.e1. |