 |
Demodex is a common yet often overlooked condition among our patients. Even though signs and symptoms may not be obvious under a slit lamp, they are sure to cause discomfort. This makes it even more imperative that we catch and treat these tiny mites as early as possible. The following case example will give you a good idea of how to go about this.
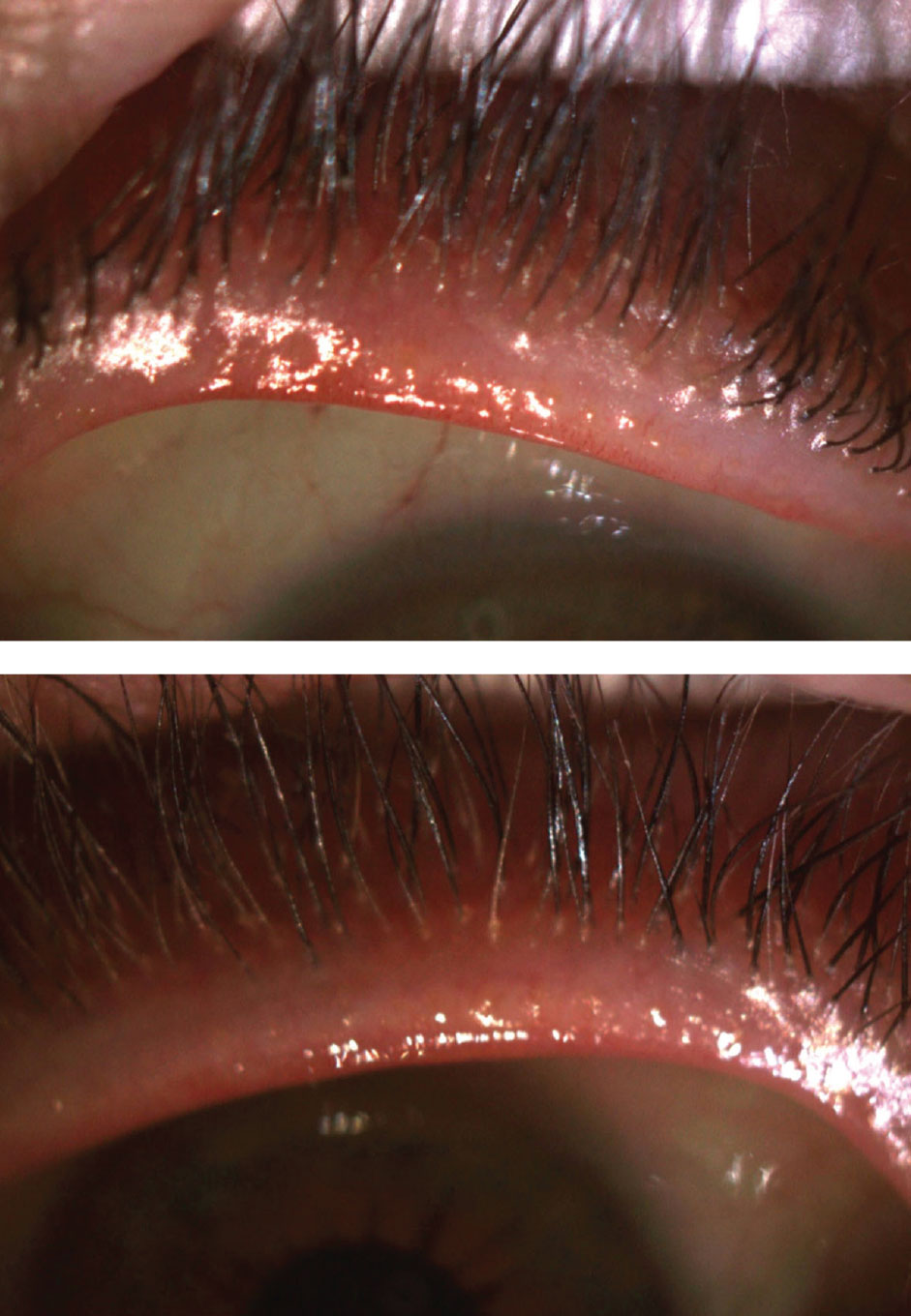 |
| Fig. 1. Lid margin examination revealed lashes that pouted at the base (OD on the top). Click image to enlarge. |
The Case
A 23-year-old female patient presented with complaints of contact lens intolerance for the past two years. The itching and discomfort she experiences worsen when she wears contact lenses, despite only using them for sport. She has tried many different contact lens brands and modalities but has found no success. Further exacerbating her symptoms is eye makeup, which she has stopped wearing altogether to avoid ocular irritation. She was diagnosed with dry eye, but warm compresses and artificial tears have not improved her signs and symptoms. She was also told she is not a good candidate for LASIK surgery due to her reduced corneal thickness and unique lens prescription.
The patient’s presenting visual acuity was 20/20 OU with her spectacles, which had a prescription of -8.00D OD and -9.00D OS. She wore Acuvue Oasys 1-Day HydraLuxe lenses with a base curve of 8.50mm and a prescription of -7.00D OD and -8.00D OS. She was receiving topical treatment for facial rosacea, which was mild and under control. Her ocular history was not significant, but she did report that she had taken oral doxycycline in the past.
Her pupils were reactive to light, with no relative afferent pupillary defects in either eye, and extraocular movements were full OU. Slit lamp examination revealed clear corneas OU, a clear palpebral conjunctiva with no papillae OU and a deep and quiet anterior chamber OU.
Examination of the lid margin revealed telangiectasia OU and cylindrical collarettes with lashes that pouted at the base (Figure 1). The patient’s meibomian glands expressed clear oil. Her non-contact tear breakup time was five seconds OD and four seconds OS, keratometry readings were 45.00/46.00@045 OD and 44.00/44.50@150 OS and intraocular pressures were 10mm Hg OD and 11mm Hg OS. Undilated posterior segment evaluation revealed a normal fundus OU.
The Verdict
The patient’s soft contact lenses fit well and centered with good movement. While the lid margin initially appeared relatively clear and clean, the lashes pouted at the base. That, along with the fact that the patient had a history of facial rosacea, made me suspicious of possible Demodex burrowed in her lash follicles.
I temporarily suspended contact lens wear and put the patient on a regimen that would treat her ocular rosacea and Demodex—twice daily Oust Demodex cleanser (OcuSoft) and Avenova spray (NovaBay). I asked her to avoid common triggers of rosacea, including sun, dairy, alcohol and caffeine, and to continue application of warm compresses daily for 10 minutes with a plug-in eye mask. I advised her to discontinue makeup use indefinitely. If she made the decision to wear it, I recommended she purchase products with clean ingredients and no irritants and ensure complete removal after each use.
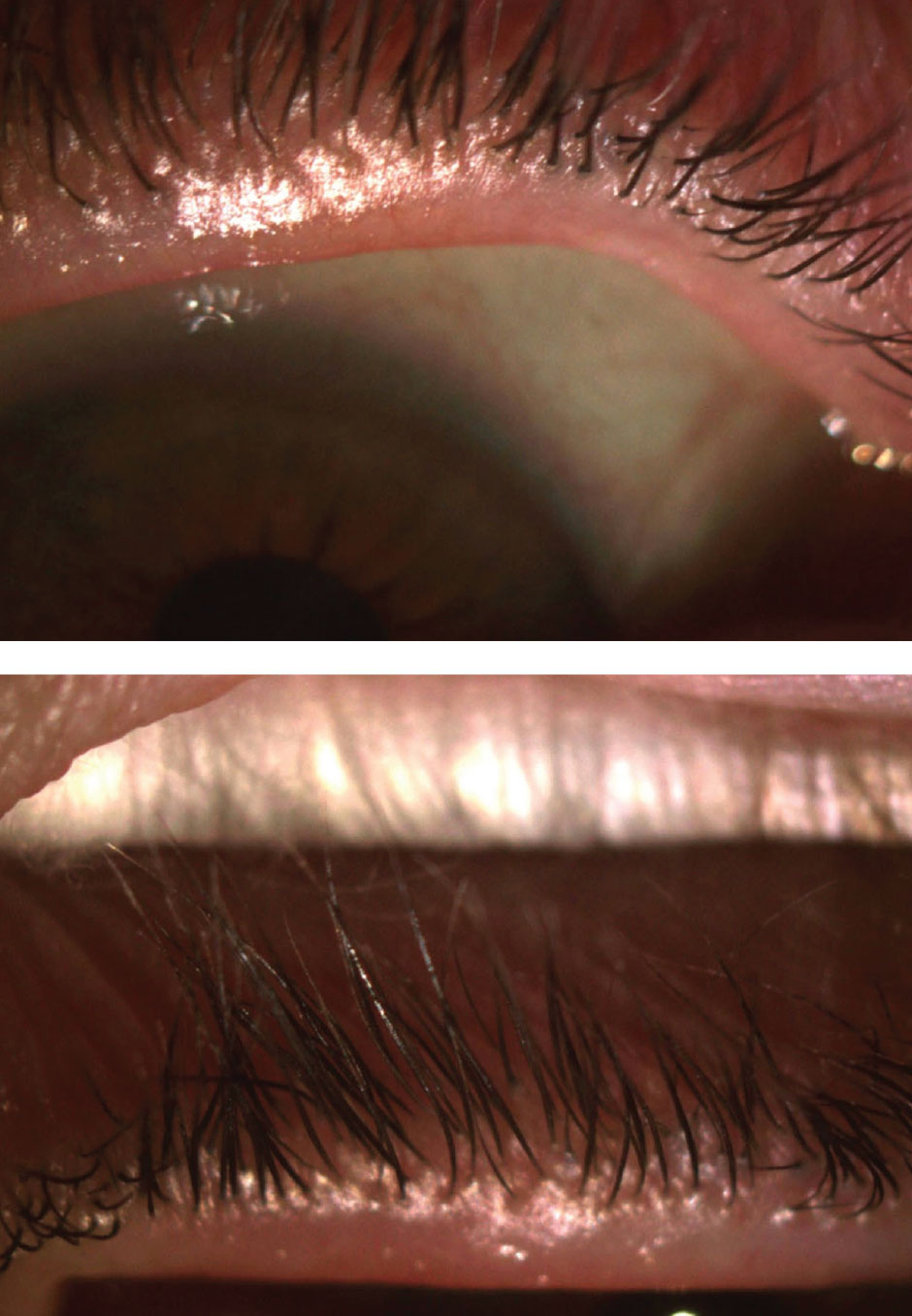 |
| Fig. 2. After discontinuing contact lens wear for a week, the patient’s lashes were still pouted (OD on the top). Click image to enlarge. |
Follow-ups
The patient came back one week later stating her itching had slightly improved but was still present. Upon examining the anterior segment, I found clear and clean lashes, but the lash base was still pouted (Figure 2). I performed in-office BlephEx on both eyelids with tea tree oil and asked the patient to continue lid cleansing with the same regimen.
She returned after another week had passed with improved symptoms. Slit lamp examination revealed clear lids and lashes. I gave her permission to resume contact lens wear and asked her to follow up in a week.
The patient was now able to wear her lenses for eight hours at a time, which was a significant improvement from her previous experience. I suggested she increase lubrication with preservative-free artificial tears, and we discussed scleral lenses and more aggressive treatment of her rosacea, such as oral antibiotics or intense pulsed light therapy, if her condition worsened. The patient was happy with her current situation, and the fit was finalized.
Discussion
Demodex is a common condition in patients who also have rosacea.1 The skin inflammation associated with rosacea makes these patients more prone to blepharitis, the bacteria of which Demodex like to feed on. Even when the blepharitis seems to be under control, the mites can embed in the lash follicle and cause discomfort.
Rosacea is more common in women and light-skinned patients but can be underdiagnosed in those who have darker skin. Patients with rosacea are typically more sensitive to facial products since the blood vessels lay close to the top layer of skin.2 They should avoid food triggers and use hypoallergenic products and sunscreen to protect them from ultraviolet light.3
Tea tree oil lid washes are a form of preventative therapy for patients with rosacea. Inform patients that long-term treatment is usually required to control the effects of rosacea—a chronic condition that requires daily maintenance to manage its symptoms.
| 1. Gonzalez-Hinojosa D, Jaime-Villalonga A, Aguilar-Montest G, et al. Demodex and rosacea: is there a relationship? Indian J Ophthalmol. 2018;66(1):36-8. 2. Knox C. Rosacea: a review of a common disorder. The Internet Journal of Academic Physician Assistants. 2006;4(2). 3. National Rosacea Society. www.rosacea.org. Accessed April 10, 2020. |


