Widespread change is happening at a breakneck pace in the ophthalmic field, though new research and concepts for future studies remain cornerstones for all advancements. This year’s Association for Research in Vision and Ophthalmology’s (ARVO) meeting in Seattle, Wa. offered practitioners a peek at some of the newest discoveries and advances designed to aid in clinical practice. Areas of study included dry eye and associated comfort issues, keratoconus and its treatments and bacterial infections related to contact lens wear.
Infection and Inflammation
Data collected on antibiotic resistant-bacteria highlights changing trends, report researchers who evaluated the frequency of methicillin-resistant Staphylococcus (MRS) keratitis as it appeared in a referral ophthalmology center in Mexico City, Mexico from February 2014 to February 2015.1 The bacteria identified via diagnosis of infectious keratitis and positive culture predominantly included Staphylococcus, with those organisms that were drug resistant noted as being non-responsive to oxacillin and/or cefoxitin disk diffusion. These results are concerning because resistance to multiple antibiotics means treatment options are limited.
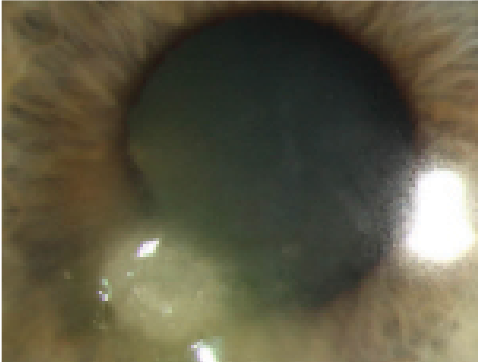 | |
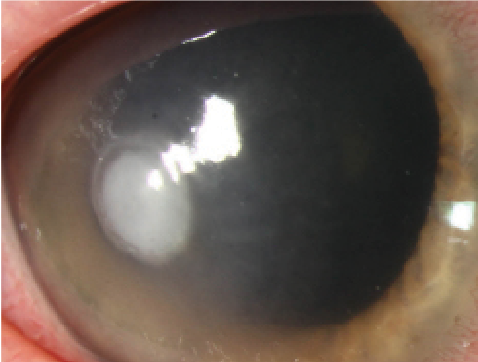 | |
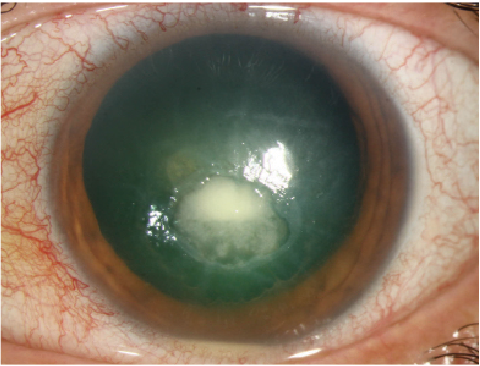 | |
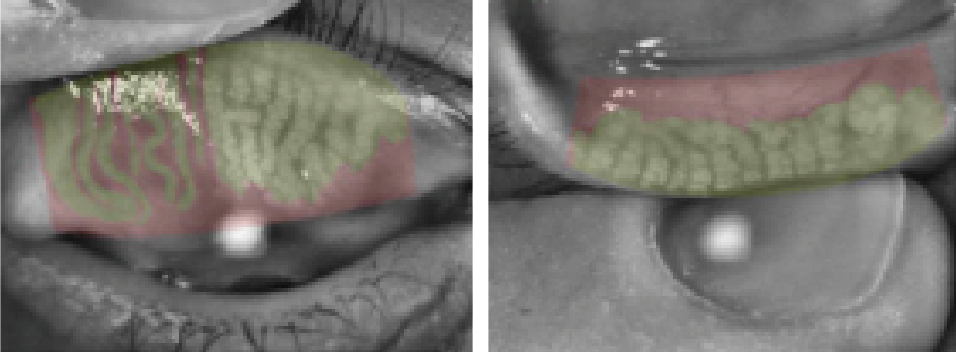
| From left to right: Moraxella nonliquefaciens ulcer, Pseudomonas ulcer and HZO neurotrophic cornea with bacterial superinfection. Research from this year’s ARVO conference could lend insight into treating these issues. Photos: Christine W. Sindt, OD |
Antibiotic resistance trends should be kept in mind when selecting therapy preoperatively, researchers from New York suggest.2 Use of topical antibiotics is key to help with minimizing intraocular infections prior to and following surgery, as bacterial resistance continues to be a prevalent issue and can inhibit an otherwise positive therapeutic effect. In this study, the investigators examined the resistance profiles of common bacterial pathogens to the antibiotics that are routinely used by ophthalmologists. One hundred and seventy-two aqueous and vitreous humor isolates of note were collected from the ARMOR surveillance study, including 11 with Haemophilus influenzae, 10 with Pseudomonas aeruginosa, 21 with Streptococcus pneumoniae, 30 with Staphylococcus aureus, and 100 with coagulase-negative staphylococci (CoNS). Minimum inhibitory concentrations (MICs) were determined by broth microdilution and the isolates were categorized as susceptible, intermediate or resistant according to systemic breakpoints. Results from the study indicated antibiotic resistance was most prevalent among staphylococci, particularly CoNS, with higher rates of opposition observed to azithromycin, ciprofloxacin and oxacillin/methicillin. At least 70% of the methicillin-resistant staphylococci samples collected demonstrated multidrug resistance; furthermore, among S. pneumoniae isolates, resistance was highest to azithromycin, chloramphenicol and oral penicillin.
Another study evaluated povidone iodine (PI) as a potential disinfecting solution for contact lenses, focusing on its antimicrobial efficacy against ocular bacterial strains in planktonic form and following biofilm formation in the contact lens case.3 Researchers in New South Wales, Australia found that the PI solution performed exceptionally well against the planktonic forms of all bacteria strains tested; in fact, no viable organisms were recovered following the minimum recommended disinfection time. The PI solution was also effective to varying degrees at removing the bacterial biofilm; air-drying or wiping the lens case with a tissue and then air-drying was deemed most effective (71% of the biofilm was removed), while recapping the lens case wet was less so (55% removed). As such, results demonstrate not only that ocular strains of bacteria are susceptible to povidone iodine in planktonic and biofilm form, but also reiterates the importance of air-drying in maintaining lens case hygiene.
Directed energy at certain wavelengths may be capable of eliminating the presence of Acanthamoeba from contact lenses and lens cases, report researchers in Pennsylvania, who hypothesized that certain levels of ultraviolet energy administered with and without riboflavin will eradicate Acanthamoeba while maintaining the clarity of the contact lens.4 To test this theory, the team administered multiple modes of energy in microjoules/cm² x 100 in a dose-dependent manner. Three groups were prepared: Acanthamoeba castellanii (106 cysts in saline) exposed to just UVE; Acanthamoeba castellanii (106 cysts in saline) plus soft contact lens exposed to just UVE; and Acanthamoeba castellanii (106 cysts) plus soft contact lens exposed to UVE in a saline solution or 0.01% riboflavin. The soft contact lenses were evaluated for clarity following exposure via spectrophotometry. Results indicated a total UVE amount of 89,991 microjoules/cm² x 100 for a time length of 180 minutes is required to eliminate the presence of Acanthamoeba castellanii in all three groups.
Though the rate of complications associated with scleral lens wear remains low, certain issues continue to be prevalent and should be further monitored, according to researchers from Minnesota, Illinois, Ohio and Massachusetts, who collected data from a 19-question survey regarding scleral lens wear and management practices administered to eye care practitioners between January 12, 2015 and March 31, 2015 by the Mayo Clinic Survey Research Center.5 Nine hundred and eighty nine individuals responded to the survey, 723 of whom reported fitting five or more patients with scleral lenses for a total of 84,735 scleral lens patients represented. Reported issues included edema, neovascularization, infiltrates, toxic keratopathy, bullae and microbial keratitis as well as limbal stem cell compromise, elevated intraocular pressure, uveitis and retinal detachment. Handling error was reported as the primary cause of these problems in 448 patients.
 | |
| Anterior segment OCT measurements could help practitioners assess ocular surface dryness in patients with conjunctovochalasis. Photo: Christine W. Sindt, OD |
Dry Eye
Keratoconjunctivitis sicca (KCS) pathology may be improved via topical antioxidant therapy, report researchers from the United States, Finland and Lithuania.6 In this study, six-week-old mice were exposed to a desiccating environmental chamber with airflow and humidity levels set at 15 L/min and 5%, respectively, for 10 days. Each mouse received transdermal scopolamine in their left eyes twice daily with superoxide dismutase (SOD) mimetic Manganese (III)-5,10,15,20-tetrakis (N-methylpyridinium-2-yl) porphyrin Pentachloride (MnTM-2-PyP, EMD Millipore) diluted in physiological saline at 0.05%. Their right eyes served as controls and were treated with saline. Study results indicated the topical administration of the MnTM-2-PyP significantly improved lacrimal gland pathology compared with the effects of the saline control, suggesting topical antioxidant therapy may be feasible as a treatment for KCS.
A study from investigators at Cornell Medical College, University of Illinois College of Medicine and Indiana University of Medicine suggested exposure of the corneal surface to hyperosmotic tears may cause considerable damage to corneal subbasal nerve fibers.7 The researchers studied the relationship between tear hyperosmolarity and corneal nerve abnormalities for the recorded first time ever in an effort to explain the common signs and symptoms associated with dry eye disease. Results indicated the responses of the corneal neurons to the drying of the cornea were depressed or completely abolished by hyperosmolar tears in a timely and dose-dependent manner. The researchers observed that the disappearance of action potentials occurred as quickly as two minutes, but generally within three hours following application of the tear solutions and suggested these findings are consistent with the abnormal activities of trigeminal ganglion neurons demonstrated by electrophysiological recordings and may account for the signs (i.e., morphological abnormalities) and symptoms (i.e., abnormal sensations) reported in dry eye patients.
 | |
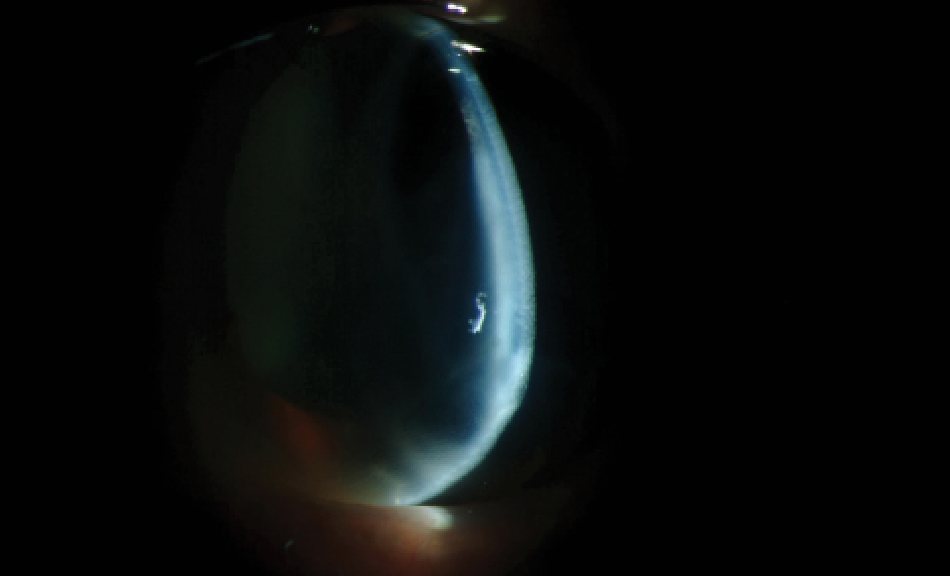
| Meibomography images demonstrating the effects of electronic device use on ocular dryness. Photos: Jennifer Hartman, OD |
Dry eye disease may also play a role in inhibition of corneal graft survival, says a team of scientists from Schepens Eye Research Institute, Harvard Medical School and the Juntendo University School of Medicine in Japan.8 These researchers evaluated the effect of the condition on allosensitization and graft rejection by transplanting healthy corneas with dry eye disease from donor mice onto recipient mice. Graft survival rates and opacity scores were evaluated with slit lamp biomicroscopy. Corneas and draining lymph nodes were harvested at day 14 post-transplant and findings demonstrated that the transplant recipients with the DED donor corneas demonstrated significantly reduced graft survival (i.e., 10%) as compared with control mice (50% survival).
Other research from Germany on omega-3 fatty acids (O3F) indicates they could be used as potential topical adjunct therapy for dry eye.9 Oral and topical treatments that use omega-3 fatty acids have previously demonstrated positive effects on the severity of dry eye. In the current study, experimental dry eye (EDE) was induced in mice and topical therapy was administered. Therapeutic treatment of mice with omega-3-fatty acids using a semi-fluorinated alkane (F6H8) as a preservative-free lipophilic carrier demonstrated a significantly earlier decrease of epithelial damage following EDE as compared with untreated controls or another treatment. The amount of tear fluid also increased following 03F/F6H8 treatment as compared with levels of the same in untreated controls or those treated with F6H8 alone or with artificial tears, as did the number of goblet cells.
Additionally, anterior segment optical coherence tomography (AS-OCT) may be appropriate for clinicians to use in assessing the level of ocular dryness in patients with conjunctivochalasis, report researchers from the University of Jukui in Japan, who compared tear meniscus area and height in patients with the disease and those with normal eyes.10 Potential relationships between TMA or TMH and fluorescein film tear-breakup time, fluorescein staining score and the extent of conjunctivochalasis were also evaluated in the conjunctivochalasis group. Results indicated that conjunctivochalasis eyes exhibited a reduced TMA and increased TMH as compared with the normal eyes. Note, a more severe dry eye condition in conjunctivochalasis is commonly associated with a reduction in TMA, despite a high level of TMH due to the conjunctival fold. As such, AS-OCT technology may be appropriate for use in this type of patient scenario.
 | |
| Pseudophakia and severe dry eye from graft-versus-host disease. Researchers presenting at this year’s ARVO conference found that dry eye may inhibit survival of corneal grafts. Photo: Christine W. Sindt, OD |
Japanese researchers in the field also suggest that addressing the presence of patient sleep disorders may help alleviate cases of dry eye.11 A cross-sectional case control study involving 715 outpatients diagnosed with DED, chronic conjunctivitis or allergic conjunctivitis incorporated the Pittsburgh Sleep Quality Index (PSQI) and Hospital Anxiety and Depression Scale (HADS) as a means to evaluate their well-being. Regression analysis of patients with DED revealed correlations between higher PSQI and HADS and the presence of DED, rather than other forms of ocular surface disease. There was also a connection to the condition’s level of severity, further raising quality-of-life concerns and supporting the theory that providing psychiatric help to address a patient’s sleep issue may have a direct effect on the improvement of their ocular health.
Patients who use digital devices throughout the day, regardless of their age, may experience adverse impacts on their work performance, productivity and quality of vision, suggests a team of researchers from Illinois, Pennsylvania, California and Tennessee.12 Overall, eye care practitioners have noted an increase in dry eye symptoms as the use of digital devices—including handheld tablets, smartphones, laptops and computers—increases. Data collected from questionnaires related to digital device use as well as additional answers regarding vision fluctuation concerns and contact lens wear were used to generate results for the study. Six hundred and eighty-six subjects were evaluated, with the average number of hours spent on devices per day noted at 6.35 hours for the <40 age group and 4.83 hours for the >40 age group. Average ocular comfort was recorded on a scale of one to 10 as one at the beginning of the day and seven at the end of the day following gratuitous digital device use, further demonstrating a positive correlation.
A second study organized by researchers in Indiana and California in cooperation with CooperVision found that frequent and severe eye fatigue is prevalent among soft contact lens wearers who use digital devices.13 Previous reports have found that eyestrain or eye fatigue occurs in roughly 60% of student and working populations that use digital devices and typically results in a notable decrease in quality of life. This study attempted to quantify the symptoms most frequently associated with eye fatigue while using digital devices in soft contact lens wearers, who were asked to complete a survey with questions pertaining to the condition. Eighty-eight percent reported experiencing eye fatigue once per month, while 74% reported experiencing eye fatigue at least once per week. Reported symptoms included dryness, eye irritation, eyestrain and tired eyes. Strain, soreness, tiredness and headache comprised primary sensation factors, while burning, irritation and dryness comprised the secondary sensation factors in the study. Additionally, blurring, doubling and moving/floating were noted as visual sensation factors. The researchers concluded that frequent and severe eye fatigue is highly prevalent among the population of soft contact lens wearers that use digital devices, and that the recorded symptoms can be used to better identify members of this population.
According to German investigators in Cologne who examined the onset of DED pain symptoms like burning, stabbing or photophobia that presented without accompanying clinical signs including normal visual acuity, intraocular pressure, Schirmer test and corneal fluorescein staining in combination with pathological Ocular Surface Disease Index score, there is a correlation between patients with a discrepancy of signs and symptoms in dry eye that are resistant to therapy and the presence of psychosomatic diseases and/or previous eye surgery.14 Typically, in these cases of symptoms without signs, corneal neuralgia is postulated; however, the results from this study that indicate the co-morbidities of psychosomatic disease or prior eye surgery suggest there may be different sensitization pathways for the proposed development of corneal neuralgia than previously believed. Furthermore, incomplete analgesia following topical corneal anesthesia supports the assumption of a central sensitization that would explain the resistance to topical therapy, the researchers concluded.
A cross-sectional study open to all participants of the American Academy of Optometry’s 2015 annual meeting suggested that the Standard Patient Evaluation of Eye Dryness (SPEED) questionnaire may not be as successful at detecting dry eye in contact lens wearers as it is in those who do not wear lenses.15 One-hundred and fifty contact lens wearers and 134 non-lens wearers elected to participate in the study by answering the questions listed as part of the SPEED questionnaire and undergoing tear meniscus height photographic assessment and tear volume testing. Unfortunately, while the questionnaire was accurately able to predict the dry eye status in non-contact lens wearers, it was unable to predict the same in those wearing lenses. The researchers concluded additional work should be conducted to further assess the study’s usefulness in contact lens wearers.
Furthermore, artificial tears may be less beneficial than initially believed for patients with ocular surface disease, according to investigators from Virginia who incorporated a modified version of the Schirmer test into their research.16 Study participants were divided into three groups: a control group not treated with artificial tears, a group with ocular surface symptoms that responded to artificial tear treatment, and a group with similar ocular surface symptoms that did not respond to the tears. No significant difference in standard Schirmer test scores, modified Schirmer test scores, punctate epithelial erosion presentation (PEE), meibomian gland dysfunction (MGD), blepharitis tear break-up time (TBUT) or Ocular Surface Disease Index (OSDI) scores was noted in any group. The researchers concluded that current clinical tests are not able to adequately identify the subset of patients who might most benefit from artificial tear use. Given the low cost and morbidity of artificial tear treatment, they suggest a trial treatment of the prescribed drops be performed in patients with chronic ocular surface symptoms and add that future studies should take into account the type of artificial tears used as well as frequency of use.
Keratoconus and Its Potential Remedies
In Australia, investigators examined changes in corneal sensitivity and their association with other clinical parameters in keratoconus patients.17 Ocular symptoms using validated questionnaires, corneal topography, tear osmolarity, tear meniscus height measurement, tear volume, ocular surface staining with fluorescein and lissamine green dye, corneal sensitivity using Cochet-Bonnet aesthesiometer and corneal nerve mapping using HRT II confocal microscopy were recorded, and correlations were made using either Spearman’s or Pearson’s coefficient. Subjects were graded as having either mild or severe keratoconus, and partial correlation was performed to control the effect of confounding factors. Only data from each patient’s most severe eye was included in the study. Results found central corneal sensitivity to be lower in the severe keratoconus group, while in bivariate correlations, decreased corneal sensitivity in keratoconus was associated with condition severity, lower central nerve fiber density, contact lens wear, contact lens tolerance, patient age and duration of disease. Researchers further observed a distinctive trend in which age and duration of keratoconus was also associated with decreased corneal sensitivity, and that contact lens wear-intolerants exhibited higher corneal sensitivity compared with tolerant wearers. They concluded that decreased corneal sensitivity was associated with age and duration of disease, and that reduced tolerance of keratoconic patients to contact lens wear was associated with increased corneal sensitivity.
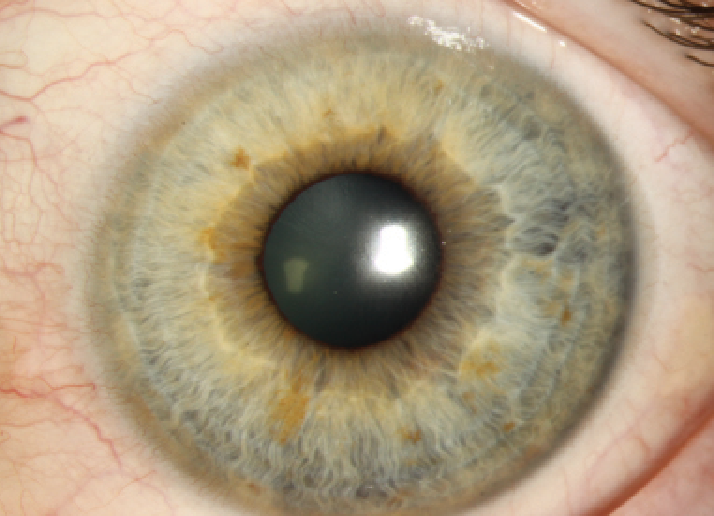
 | |
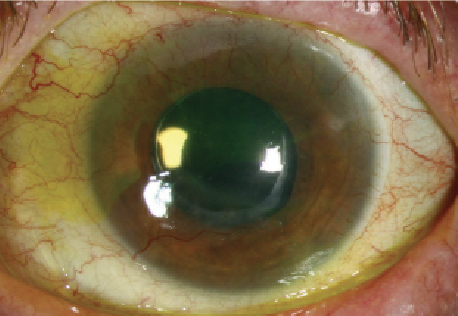
| A slit lamp view of a keratoconic patient with hydrops. Research is increasingly looking at the implications of this irregular corneal condition and potential methods for its management. Photo: Christine W. Sindt, OD |
Hair cortisol concentration as a biochemical correlate of chronic psychological stress may be an observable risk factor for keratoconus, report German scientists who analyzed strands of hair taken from both healthy and keratoconic patients.18 As hair segments of 3cm in length represent the prior three-month stress profile of an individual, the researchers used sections of hair this length located most proximal to the scalp. Cortisol levels were determined using the hair by the Institute of Biopsychology of the TU Dresden; a standardized questionnaire for chronic stress was also administered to all subjects. Results indicated hair cortisol was higher in patients with progressive keratoconus compared with those with a stabilized form of the disease or those who were healthy. Furthermore, the study suggested increased hair cortisol concentration could be a risk factor for the progression of keratoconus.
Other research from Germany supports the concept that axis alignment could be used in an algorithm to support the diagnosis and staging of keratoconus.19 Scientists compared the power and axis orientation of anterior and posterior astigmatism in 861 eyes with keratoconus and 500 healthy eyes as part of a retrospective study, finding posterior axis alignment of corneal astigmatism is in line with the alignment of the anterior surface in the majority of cases of keratoconus. In contrast, the majority of the healthy eye group demonstrated a vertical posterior axis alignment independent of the anterior surface. These results indicate that with progression of the disease and a decrease in pachymetry, corneal resistance to vertical forces—most likely the eyelids—decreases and axis orientation becomes increasingly vertical.
Corneal crosslinking may effectively relieve the intensity and frequency of pain associated with bullous keratopathy for at least one year following treatment, report researchers in Tokyo, Japan, who conducted a retrospective observational case study to monitor post-operational results of 11 patients who had undergone surgery for the condition.20 Patient best-corrected visual acuity (BCVA), intraocular pressure and corneal thickness were examined prior to treatment, as well as at one-week, and three-, six- and 12-month intervals following treatment. Intensity and frequency of pain were scaled from zero to 10, while after 12 months of treatment, corneal stromal depths of 100μm and 200μm were observed using confocal microscopy. Density of the patients’ keratocytes and nerve fibers was also calculated. Results indicated that BCVA did not significantly improve following treatment, but pain—which was initially scored at an average of 6.27—decreased. Furthermore, the mean pain frequency score of 5.45 also decreased following treatment to 1.27 at 12 months post-operation, while keratocytes and nerve fibers were rarely observed at 12 months following the procedure. Persistence of pain relief was ultimately attributed to the inadequate regeneration of nerve fibers in the corneal stroma.
Other abstracts from ARVO 2016 highlight alternative treatment options, surgical techniques and potential concerns on the horizon to be aware of. As always, practitioners are encouraged to review the full list of available abstracts, not just those chosen for this report. So, go take a look!
Dr. Shovlin is the senior optometrist at Northeastern Eye Institute and a member of the adjunct faculty at the Pennsylvania College of Optometry. He is also the clinical editor for Review of Cornea & Contact Lenses, associate clinical editor for Review of Optometry and president-elect for the American Academy of Optometry.
1. Avila-Lule I, Teran-Tejada T, Betancourt NR, et al. Methicillin-resistant staphylococcus keratitis in a referral ophthalmology center. Program 2354. Association for Research in Vision and Ophthalmology Meeting 2016.
2. Asbell PA, DeCory H, Sahm D, Sanfilippo CM. In vitro antibiotic susceptibility of ocular pathogens collected from the aqueous and vitreous humor during the ARMOR surveillance study. Program 2348. Association for Research in Vision and Ophthalmology Meeting 2016.
3. Vijay AK, Liu L, Nguyen TC, et al. Efficacy a novel povidone iodine based contact lens disinfection system against bacterial biofilm. Program 1454. Association for Research in Vision and Ophthalmology Meeting 2016.
4. Ross AGG, Kowalski RP, Dhaliwal D, KArenchak LM. The threshold of light energy to eliminate acanthamoeba. Program 1456. Association for Research in Vision and Ophthalmology Meeting 2016.
5. Schornack M, Harthan J, Barr et al. Complications of scleral lens wear. Program 1467. Association for Research in Vision and Ophthalmology Meeting 2016.
6. Kaja S, Kourlen P, Puranen J, Symantas R. A topically delivered synthetic metalloporphyrin SOD mimetic improves hallmarks of dry eye disease pathology. Program 396. Association for Research in Vision and Ophthalmology Meeting 2016
7. Mizerska KK, Hirata H, Dallacasagrande V, et al. Short exposure to hyperosmolar tears produces profound anatomical and physiological changes in rodent corneal nerves: implications for dry eye disease. Program 403. Association for Research in Vision and Ophthalmology Meeting 2016.
8. Inomata T, Hua J, Shiang T, et al. Is dry eye disease in donors a risk factor for corneal graft rejection? Program 1438. Association for Research in Vision and Ophthalmology Meeting 2016.
9. Gehlsen U, Braun T, Steven P. Omega-3 fatty acids using a F6H8-carrier as topical therapy in experimental dry eye disease. Program 417. Association for Research in Vision and Ophthalmology Meeting 2016.
10. Kimura K, Takamura Y, Gozawa M, et al. Difference in tear meniscus between conjunctivochalasis eyes and normal eyes using anterior segment optical coherence tomography. Program 2836. Association for Research in Vision and Ophthalmology Meeting 2016.
11. Ayaki A, Kawashima M, Negishi K, et al. Sleep disorders in dry eye disease and allied irritating ocular diseases. Program 2840. Association for Research in Vision and Ophthalmology Meeting 2016.
12. Harthan J, O’Dell L, Kwan JT, et al. Dry eye symptoms and visual function with digital device use. Program 2843. Association for Research in Vision and Ophthalmology Meeting 2016.
13. Kollbaum PS, Meyer D, Huenick S, et al. Digital Device user survey of eye fatigue. Program 1492. Association for Research in Vision and Ophthalmology Meeting 2016.
14. Steven P, Schneider T, Ramesh I, et al. Pain in dry-eye patients without corresponding clinical signs – a retrospective analysis. Program 2848. Association for Research in Vision and Ophthalmology Meeting 2016.
15. Pucker AD, Jones-Jordan L, Kwan JT, et al. A comparison of SPEED scores in contact lens and non-contact lens wearers. Program 2855. Association for Research in Vision and Ophthalmology Meeting 2016.
16. Young M, Zhong H, Peterson E, et al. Clinical evaluation of Schirmer test variations on the predictability of benefit from artificial tears. Program 2882. Association for Research in Vision and Ophthalmology Meeting 2016.
17. Mandathara PS, Stapleton F, Kokkinakis J, Willcox MD. A pilot study of corneal sensitivity and its associations in keratoconus. Program 2896. Association for Research in Vision and Ophthalmology Meeting 2016.
18. Lenk J, Spoerl E, Pillunat LE, Raiskup F. Hair cortisol analysis in progressive and stable keratoconus patients. Program 2906. Association for Research in Vision and Ophthalmology Meeting 2016.
19. Schmack I, Shajari G, PourSadeghian M, et al. Characteristics of corneal astigmatism of anterior and posterior surface in healthy individuals and keratoconus patients. Program 2913. Association for Research in Vision and Ophthalmology Meeting 2016.
20. Ono T, Terada Y, Mori Y, et al. The persistence of pain relief after corneal crosslinking in mild bullous keratopathy eyes. Program 2919. Association for Research in Vision and Ophthalmology Meeting 2016.


