Practitioners who follow the oft-quoted estimate that keratoconus (KC) affects one out of every 2,000 individuals are apt to miss quite a lot of cases in clinical practice. This rule of thumb is based on a 1986 publication that used diagnostic criteria that today would be considered outmoded and insensitive. Thanks to more advanced diagnostic technologies, we now know the prevalence of keratoconus is five- to tenfold higher than previously thought.
Early diagnosis of keratoconus is key to halting its progression. To do so, one of three criteria must be met: abnormal posterior corneal ectasia, abnormal corneal thickness distribution (rate of change of corneal thickness across the corneal tissue) and/or clinically non-inflammatory corneal thinning.
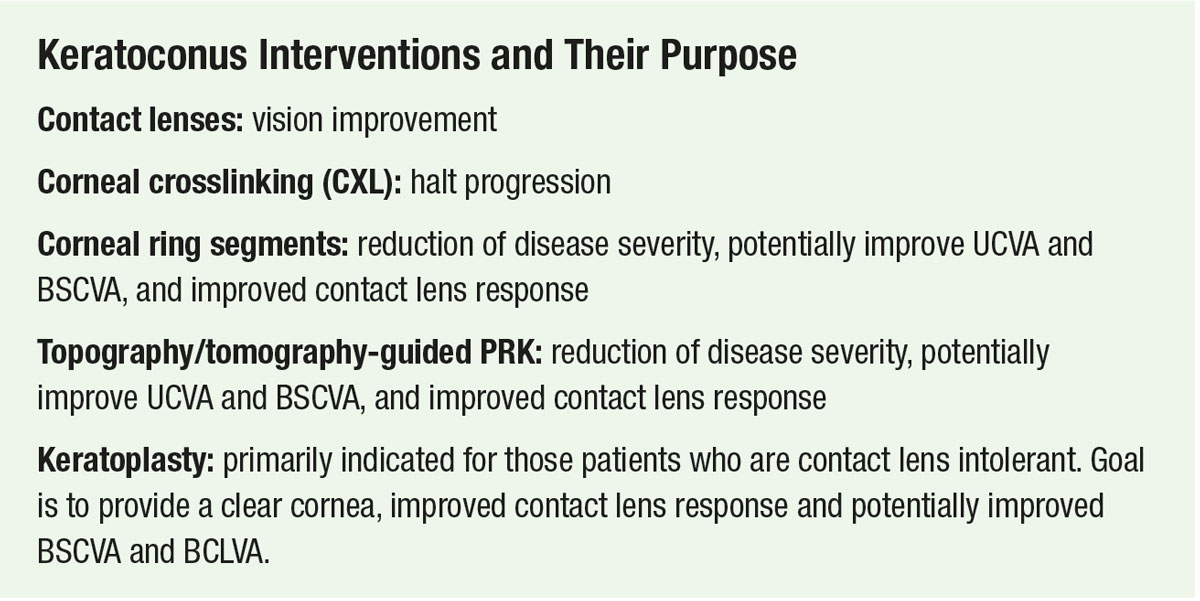
Along with early diagnosis, appropriate medical management to preserve vision has become critically important in light of the introduction of corneal collagen crosslinking (CXL). However, it remains of utmost importance to provide visual rehabilitation for those who have already suffered vision loss from the disease. The mainstay of such an effort is the application of contact lenses, and there are a plethora of options to help optimize vision that aren’t just scleral or corneal gas permeable (GP) lenses. In this two-part article, we describe all the contact lenses available today and which ones can help your patients achieve the most effective results at each stage of keratoconus, including after undergoing a corneal procedure.
Part 1 (below) discusses contact lens use as a primary visual rehab modality for keratoconic patients. Part 2 (coming in the next issue) will address surgical interventions and post-procedure contact lens fitting. Taken together, these two articles should outline a comprehensive plan for success.
 |
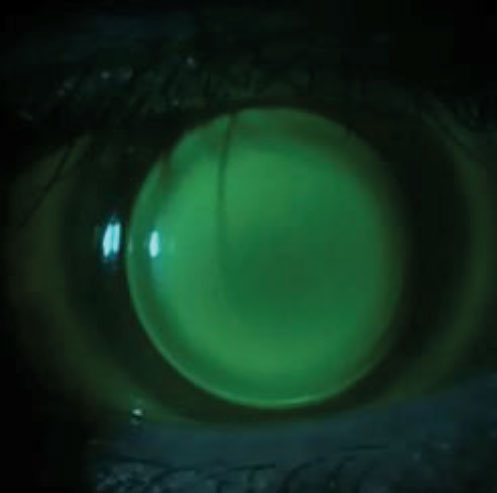
The often-extreme corneal shape change seen in keratoconus need not be intimidating to clinicians. The abundance of contact lens options all but assures we can improve vision. Photo credit: Melissa Barnett, OD. Click image to enlarge. |
Soft Contact Lenses
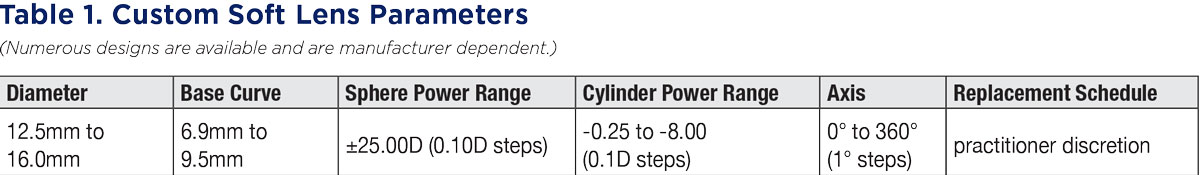
Those with early or mild KC may do well in commercially available soft contact lenses since toric and extended-range parameters are readily manufactured. If decreased acuity, reduced comfort or lens decentration is noted, numerous laboratories offer custom soft lenses with vast power ranges and parameter availability. These made-to-order lenses may provide improved vision, a better fit and greater comfort as they are tailored specifically for each patient (Table 1). In advanced KC, soft lenses have limited use since they tend to contour to and assume the shape of the irregular keratoconic cornea.
 |
| Click image to enlarge. |
Specialty Soft Lenses
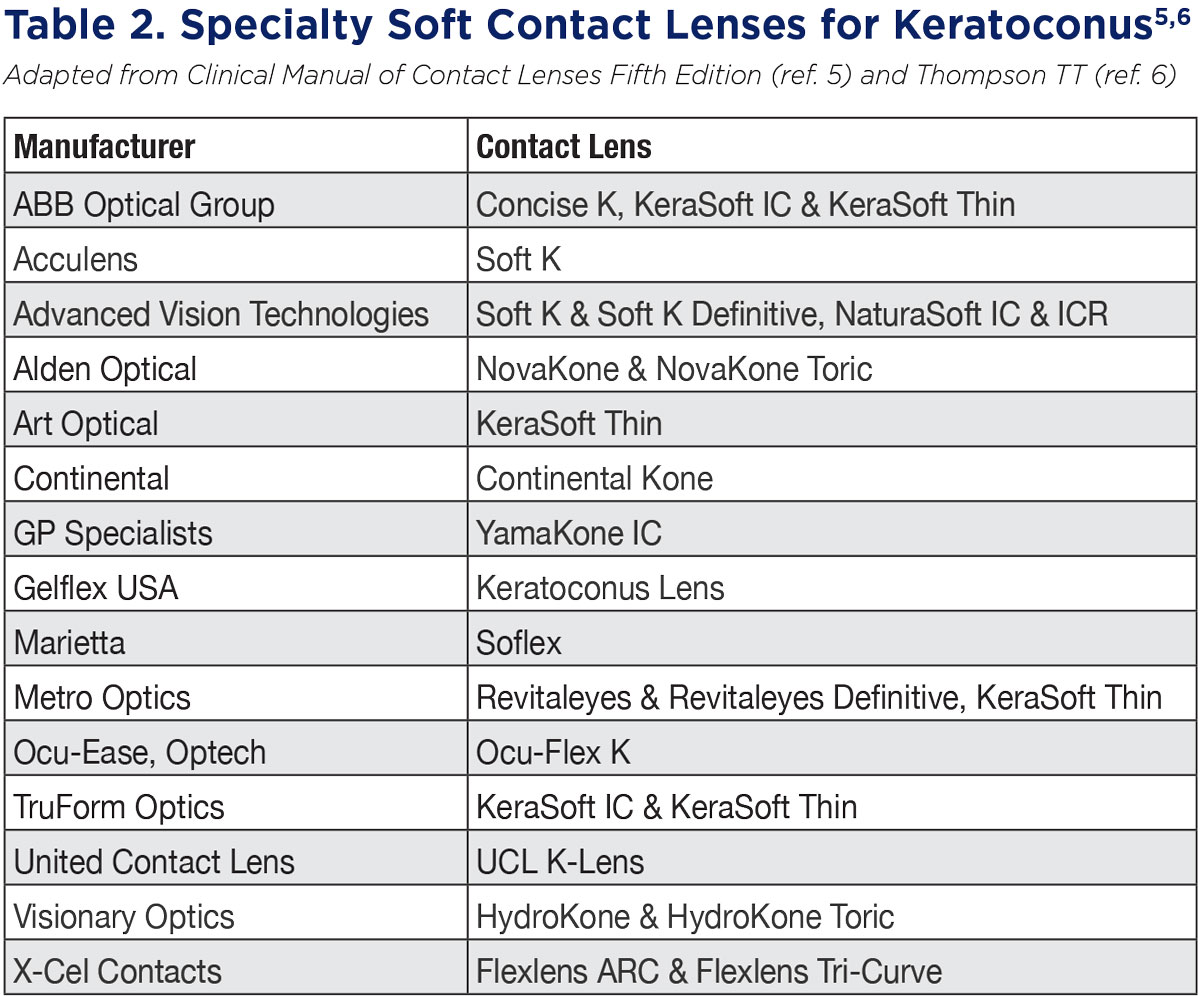
Masking front surface corneal irregularity requires a neutralizing tear lens under a smooth refractive plane, typically achieved with a GP lens.1 Specialty KC-specific soft lenses exhibit characteristics similar to a GP and mask low amounts of corneal irregularity as they are lathed in higher-modulus materials or are designed with greater lens center thicknesses. Many are available in silicone hydrogel materials or use fenestrations to prevent corneal hypoxia. Diagnostic fitting and following each manufacturer’s fit guide is recommended as numerous designs are available and vary greatly in fitting philosophy (Table 2).
 |
| Click image to enlarge. |
Corneal Lenses
Previously known as corneal GPs, these lenses play a critical role in KC management and continue to be practitioners’ initial lens of choice when fitting the irregular cornea.2 Fitting goals for a corneal lens is to vault minimally over the corneal apex to prevent epithelial disruption, and provide mid-peripheral alignment and moderate peripheral clearance. In early KC, an ideal fit is easier to obtain. In moderate to advanced KC, due to corneal irregularities and increased frequency of decentration of the cone apex, it becomes more challenging to obtain a stable and optimal fit.
KC corneas with paracentral “nipple” cones often do well in smaller-diameter corneal lenses, while corneas with larger “oval” cones or decentered cones fare better in medium or large diameter corneal lenses. A known risk factor for corneal scarring is flat-fitting lenses with associated corneal staining.3 Patients in flat-fitting lenses also experienced increased lens discomfort and a greater propensity for corneal transplantation.4
In general, KC corneal lenses are comprised of a small diameter, steep base curve radius and spherical or aspheric peripheral curves. A type of conventional lens design is the CLEK design. More recent designs include Rose K2, ComfortKone, TruKone, Dyna Z Cone, V Cone, C Cone and E Cone. Intra-limbal designs include Dyna Intra-Limbal, Rose K2 IC and the GBL.
It is imperative to avoid a harsh apical bearing relationship when fitting KC eyes, regardless of the corneal lens diameter. Two common fitting philosophies aim for either a very light apical bearing (three-point touch) or mild apical clearance (first definite apical clearance lens) fluorescein pattern.5 Adequate peripheral edge lift and movement on blink is also necessary to facilitate tear exchange and debris removal. Lens design software in some corneal topographers may simplify the fitting process by relaying information directly to GP labs. Advanced lathing technologies can fabricate asymmetric peripheral curves, creating a more uniform edge during corneal lens wear.
 |
| Click image to enlarge. |
Piggyback Lenses
Those with early or mild KC may do well in commercially available soft contact lenses since toric and extended-range parameters are readily manufactured. If decreased acuity, reduced comfort or lens decentration is noted, numerous laboratories offer custom soft lenses with vast power ranges and parameter availability. These made-to-order lenses may provide improved vision, a better fit and greater comfort as they are tailored specifically for each patient (Table 1). In advanced KC, soft lenses have limited use since they tend to contour to and assume the shape of the irregular keratoconic cornea.
 |
A piggyback approach—as in this patient, wearing a corneal lens fit on top of a silicone hydrogel—combines the crisp optics of the rigid material with the comfort profile of a soft lens. Click image to enlarge. |
Hybrid Lenses
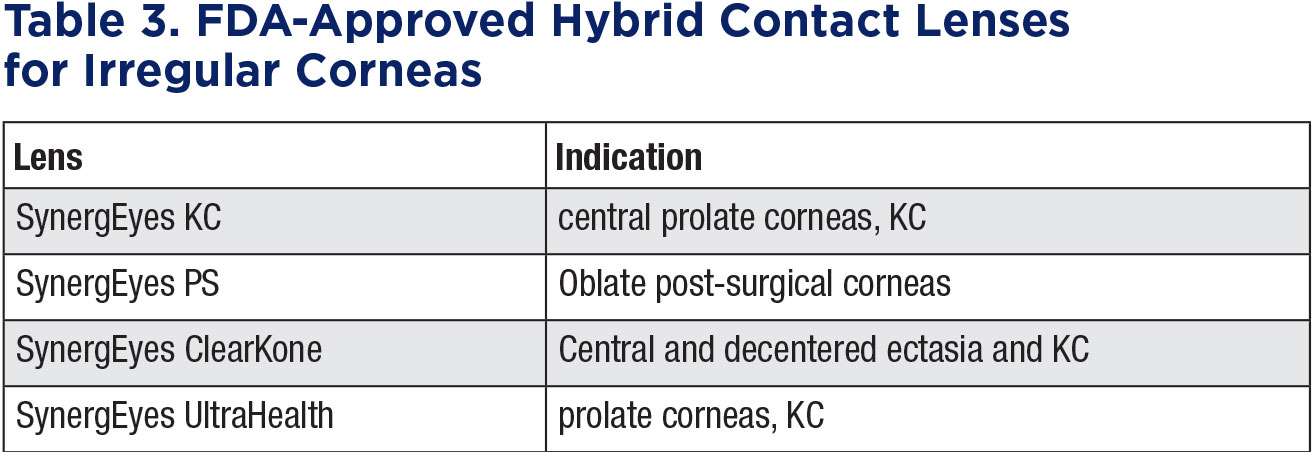
These are a natural progression from piggyback fitting. For those who have failed with corneal lenses due to poor centration, discomfort or dislodgment, hybrids resolve these issues and eliminate the cumbersome nature of tandem fitting since they are one unit. This design consists of a corneal GP bonded with a peripheral soft hydrogel or silicone skirt. The central GP lens provides crisp optics while the soft skirt enhances comfort, stability and centration.
A number of studies have detailed the benefits of fitting hybrid lenses for an irregular cornea, including increased comfort and tolerability over GPs and improvements in visual acuity, contrast sensitivity and subjective comfort vs. other contact lens options.7
SynergEyes, currently the only manufacturer of hybrid lenses in the United States, has a wide variety of designs available (Table 3), including a KC-specific lens with steep base-curve options and multiple skirts to lift the GP and allow total clearance of the ectasia. This first-generation lens is still widely used for very prolate, centrally located cones.
SynergEyes UltraHealth,the latest generation for hybrid lenses for irregular corneas,provides a reverse geometry system so that the GP center vaults over the cornea, yet with flatter base curves to eliminate high powers and aberrations. The GP core has a Dk of 130 and the skirt is made of silicone with a DK of 84 and a lower modulus to aid comfort. The weight of the lens is primarily on the soft landing portion, which also aids in centration. The SynergEyes UltraHealth FC is an extension of this lens design and is intended for more oblate corneas.
 |
| Click image to enlarge. |
Hybrid lenses have certainly evolved over the years. Some early obstacles have been overcome with the use of higher oxygen permeable materials, stronger material junctions, vaulting with reverse geometry curves and the ability for these lenses to be designed empirically. While scleral lens designs are popular to best treat the advanced stage of the disease, hybrid lenses are a better approach for patients in the form fruste, mild and moderate stages.
Central clearance of approximately 75µm to 100µm over the apex and 1mm of movement is desired. Diagnostic fitting is still an option; however, with the ability to provide either the raw topographical data or specific values such as axial Ks and eccentricity, these lenses can be designed empirically in hopes of getting a better first lens fit.
Patient selection is important. In the past, many doctors used this modality as a problem solver after other designs failed or as last resort on very challenging patients—thus, success rate was limited. Although hybrids do resolve many issues related to unstable optics of soft torics or discomfort from GPs, many reach for them successfully as first-line treatment.
 |
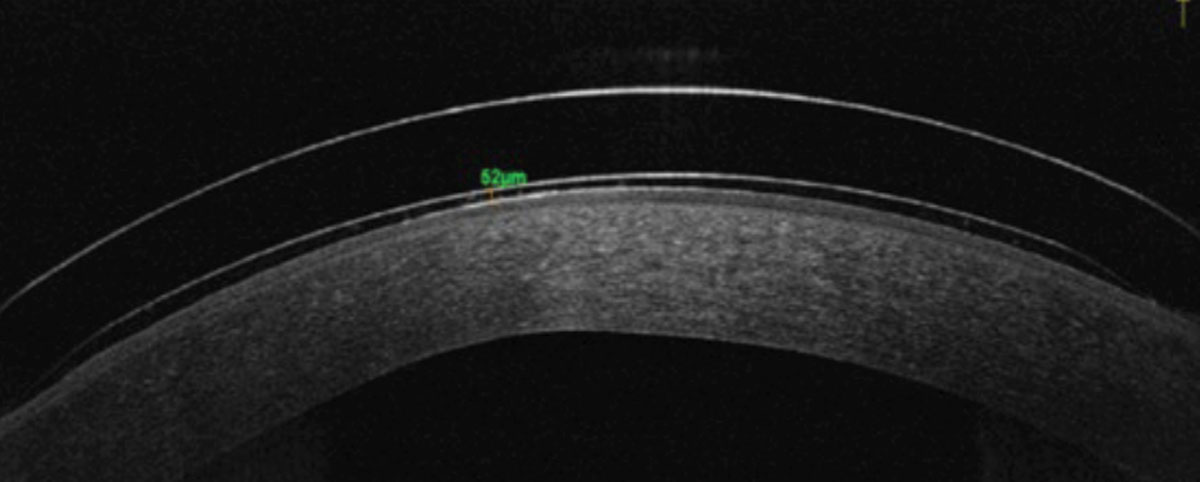 |
Slit lamp photo and OCT of an ideally fit hybrid lens on a keratoconic eye. Photo: Tiffany Andrzejewski, OD. Click images to enlarge. |
Scleral Lenses
Keratoconus is the single most common indication for scleral lenses.8-11 They neutralize irregularities of the corneal surface and offer have improved centration and stability compared to corneal lenses. Since the lens does not touch the cornea, there is improved comfort due to less lens awareness. A recent study compared the comfort and visual performance of rigid corneal lenses and sclerals in patients with corneal ectasia who successfully wore habitual corneal GP lenses. Significantly improved comfort was reported for sclerals.12
Sclerals are less likely than GPs to mechanically reshape the cornea and cause warpage. They may delay or even avoid surgical intervention, with a study showing the majority of participants who would have otherwise undergone corneal transplant surgery were successfully treated with long-term scleral lens wear.1 A similar study that evaluated the association of scleral use with the risk for keratoplasty in KC patients showed that contact lens wear significantly lowered the risk of undergoing keratoplasty.13
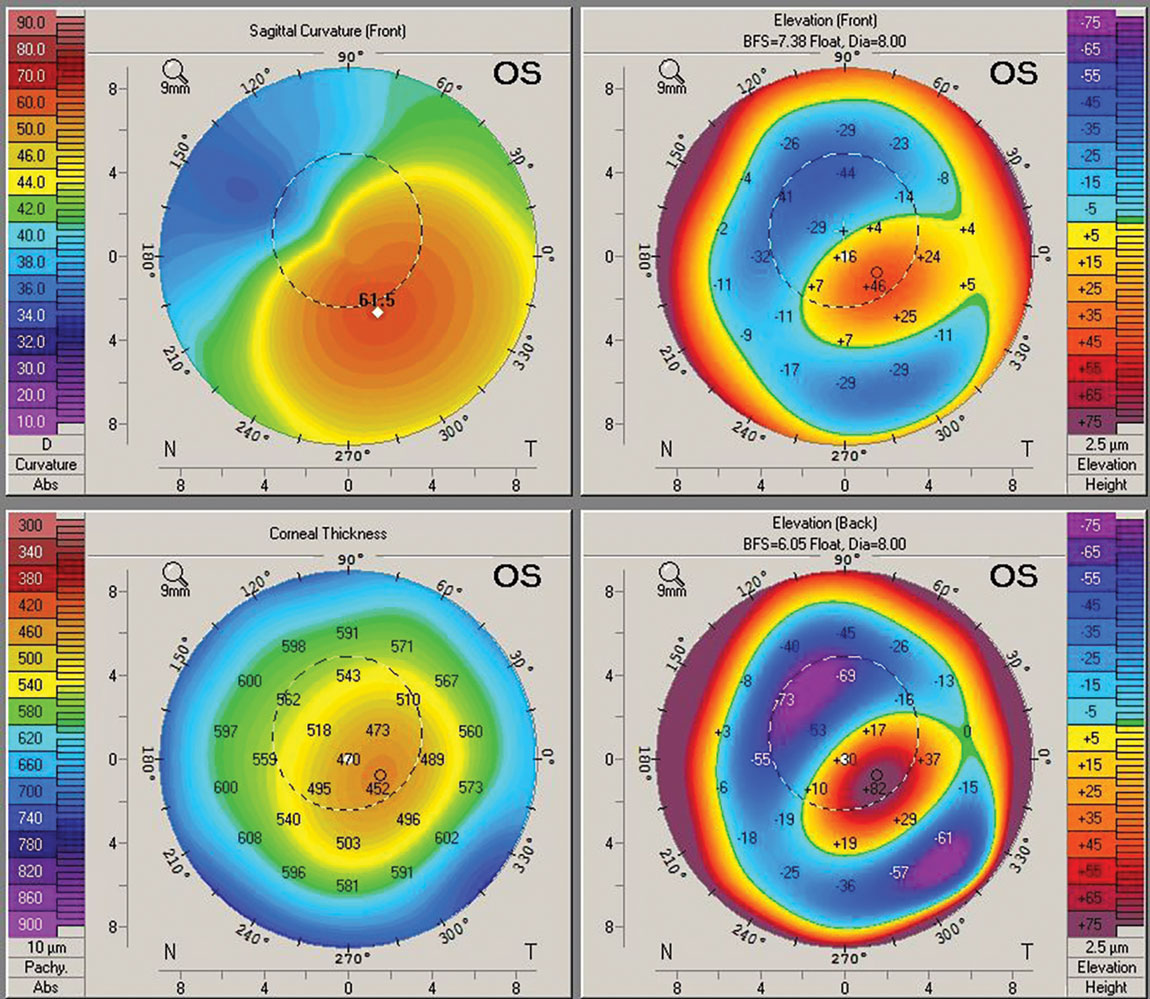 |
Having access to corneal topography and tomography is essential for achieving the best fit with custom-designed lenses for keratoconic eyes. Click image to enlarge. |
Factors to consider when selecting a scleral lens include corneal diameter, presence of ocular surface disease, palpebral aperture, ethnicity and disease severity. Corneal and scleral topography and/or tomography are also beneficial tools when determining the type of KC and areas of elevation.
With mild KC, a smaller-diameter scleral lens may be used. For those with advanced KC or keratoglobus, a larger diameter may be preferred. For progressive keratoconus, a scleral may be fit with additional sagittal depth to allow room for progression. In cases of extreme ectasia, a specialized design such as a quadrant-specific or impression-based lens may be preferred.
A recent publication described how a quadrant-specific scleral lens (BostonSight Scleral) resulted in visual improvement, a reduced need for mid-day removal and an average of two lenses needed to complete the fitting process.14
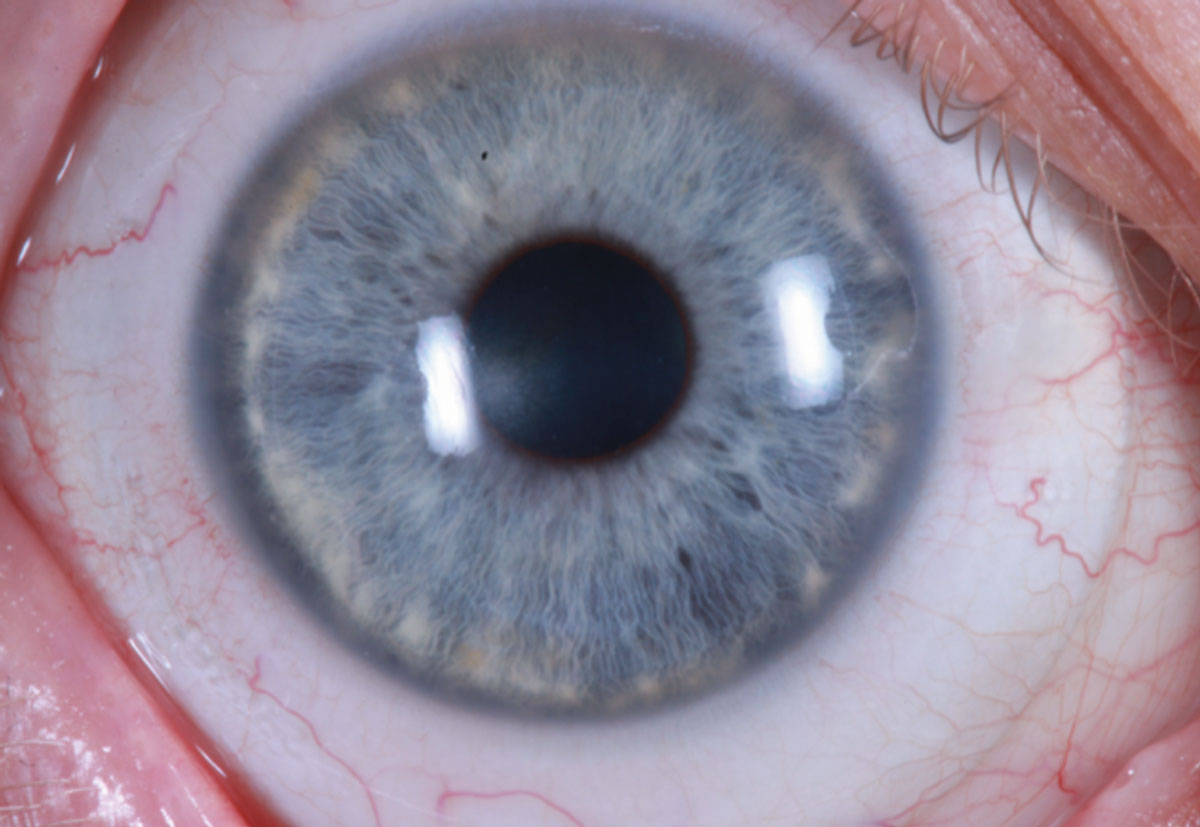 |
Scleral lenses offer several advantages when fitting a KC patient, including improved centration, stability and comfort. Photo: Tm Arnold, OD. Click image to enlarge. |
Another unique approach is an impression-based scleral lens design. In one study, patients fit with an EyePrintPro lens saw an improvement in the quality of vision, comfort of lenses, dry eyes, eye redness and pain symptoms.15
Scleral lenses are often used to minimize visual distortion after a CXL procedure for KC. They have also been used to improve vision and reduce higher-order aberrations after intracorneal ring segment implantation in keratoconic eyes. These applications of scleral lens fitting, and the various surgical procedures themselves, will be explored in detail in Part 2 of this article in the January/February issue. Stay tuned!
 |
A 19mm scleral lens with sodium fluorescein fit on an eye with a 25-year-old proud graft fit. Photo: Tom Arnold, OD. Click image to enlarge. |
Takeaways
Keratoconus has significant implications on our patients’ visual function and quality of life. Although its prevalence is fairly high, we have technologies that can halt progression and, as such, preserve visual function. Contact lenses remain the primary method of improved visual function in keratoconus.
 |
| Click image to enlarge. |
Dr. Barnett is a principal optometrist at the Univ. of California, Davis Eye Center. She is chair of the AOA’s Contact Lens and Cornea Section, a fellow of the American Academy of Optometry, a diplomate of the American Board of Certification in Medical Optometry, a fellow and global ambassador of the BCLA and a board member of the GPLI and the International Society of Contact Lens Specialists. Dr. Barnett has consulting and/or lecturing relationships with ABB, Acculens, Bausch + Lomb, Contamac, CooperVision, EveryDay Contacts, Johnson & Johnson Vision Care, SynergEyes and Tangible Science.
Dr. Eiden is president and medical director of North Suburban Vision Consultants, president and founder of the International Keratoconus Academy of Eye Care Professionals and co-founder and president of EyeVis Eye and Vision Research Institute. He is a fellow of the American Academy of Optometry and the Scleral Lens Education Society. Dr. Eiden has consulting, lecturing and/or financial interests with the following companies: Alcon, Avellino, Bausch + Lomb, CooperVision, Oculus, Special Eyes, SynergEyes and VTI.
Dr. Sclafani is vice president of professional affairs for SynergEyes and sees patients at SoLo Eyecare in Chicago and the Illinois College of Optometry. She is a fellow of the Scleral Lens Society and associate member of the International Society of Contact Lens Specialists. Dr. Sclafani is vice president of professional affairs at SynergEyes.
1. Koppen C, Kreps EO, Anthonissen L, et al. Scleral lenses reduce the need for corneal transplants in severe keratococonus. Am J Ophthalmol. 2018;185:43-8. 2. Shorter E, Harthan J, Nau CB, et al. Scleral lenses in the management of corneal irregularity and ocular surface disease. Eye Contact Lens. 2018;44(6):372–8. 3. Barr JT, Zadnik K, Wilson BS, et al. Factors associated with corneal scarring in the collaborative longitudinal evaluation of keratoconus (CLEK) study. Cornea. 2000;19(4):501–7. 4. Zadnik K, Barr JT, Steger-May K, et al. Comparison of flat and steep rigid contact lens fitting methods in keratoconus. Optom Vis Sci. 2005;82(12):1014–21. 5. Edrington TB, Barr JT, Zadnik K, et al. Standardized rigid contact lens fitting protocol for keratoconus. Optom Vis Sci. 1996;73(6):369–75. 6. Michaud L, Brazeau D, Corbeil ME, et al. Contribution of soft lenses of various powers to the optics of a piggy-back system on regular corneas. Contact Lens Anterior Eye. 2013;36(6):318-23. 7. Carracedo, G, Gonzalez-Meijome, JM, Lopes-Ferreira, D, et al. Clinical performance of a new hybrid contact lens for keratoconus. Eye Contact Lens. 2014;40(1):2-6. 8. Tan DT, Pullum KW, Buckley RJ. Medical applications of scleral contact lenses: 1. A retrospective analysis of 343 cases. Cornea. 1995;14(2):121-9. 9. Rosenthal P, Croteau A. Fluid-ventilated, gas-permeable scleral contact lens is an effective option for managing severe ocular surface disease and many corneal disorders that would otherwise require penetrating keratoplasty. Eye Contact Lens 2005;31(3):130-4. 10. Pullum KW, Whiting MA, Buckley RJ. Scleral contact lenses: the expanding role. Cornea 2005;24(3):269-77. 11. Visser ES, Visser R, van Lier HJ, Otten HM. Modern scleral lenses part I: clinical features. Eye Contact Lens. 2007;33(1):13-20. 12. Levit A, Benwell M, Evans BJW. Randomised controlled trial of corneal vs. scleral rigid gas permeable contact lenses for keratoconus and other ectatic corneal disorders. Cont Lens Anterior Eye. 2020;43(6):543-52. 13. Ling JJ, Mian SI, Stein JD, et al. Impact of scleral contact lens use on the rate of corneal transplantation for keratoconus. Cornea. 2021;40(1):39-42. 14. Barnett M, Carrasquillo KG, Schornack MM. Clinical outcomes of scleral lens fitting with a data-driven, quadrant-specific design: multicenter review. Optom Vis Sci. 2020;97(9):761-5. 15. Nguyen MTB, Thakrar V, Chan CC. EyePrintPRO therapeutic scleral contact lens: indications and outcomes. Can J Ophthalmol. 2018;53(1):66-70. |


