Lens materials are often taken for granted when fitting and prescribing scleral contact lenses. Fortunately, eye care providers have the insight of in-house fitting consultants to rely on when choosing lens materials and designs. I regularly lean on their expertise and have found it increasingly useful to better understand the unique properties of specific lens materials as I expand my scleral lens practice. Becoming more knowledgeable about the materials that make up the lenses we prescribe leads to more accurate fits earlier in the process and, ultimately, happier patients with optimal vision.
Scleral Background
Scleral lenses have undergone vast improvements since their genesis. Today, they are used with great success and can improve vision in patients with compromised corneas and dry eyes and offer more stable options for patients with multifocal or high astigmatism requirements. Patients with keratoconus, corneal trauma or irregularity, post-refractive surgery complaints, corneal degeneration and Sjögren’s syndrome are increasingly being fit with scleral lenses for improved vision and enhanced comfort.
Since the first scleral lenses were invented in the 1880s, material advances have increased oxygen permeability, improved structural integrity and customized the fit for patients with many different conditions and eye shapes.1 Having a variety of materials has led to greater success in improving and correcting vision while promoting patient comfort.
Identifying the right material is an intricate process that involves many interlocking factors and considerations. It takes a comprehensive patient history, unimpeded patient-doctor communication and sometimes trial and error to find a lens that balances vision correction with eye health and patient comfort.
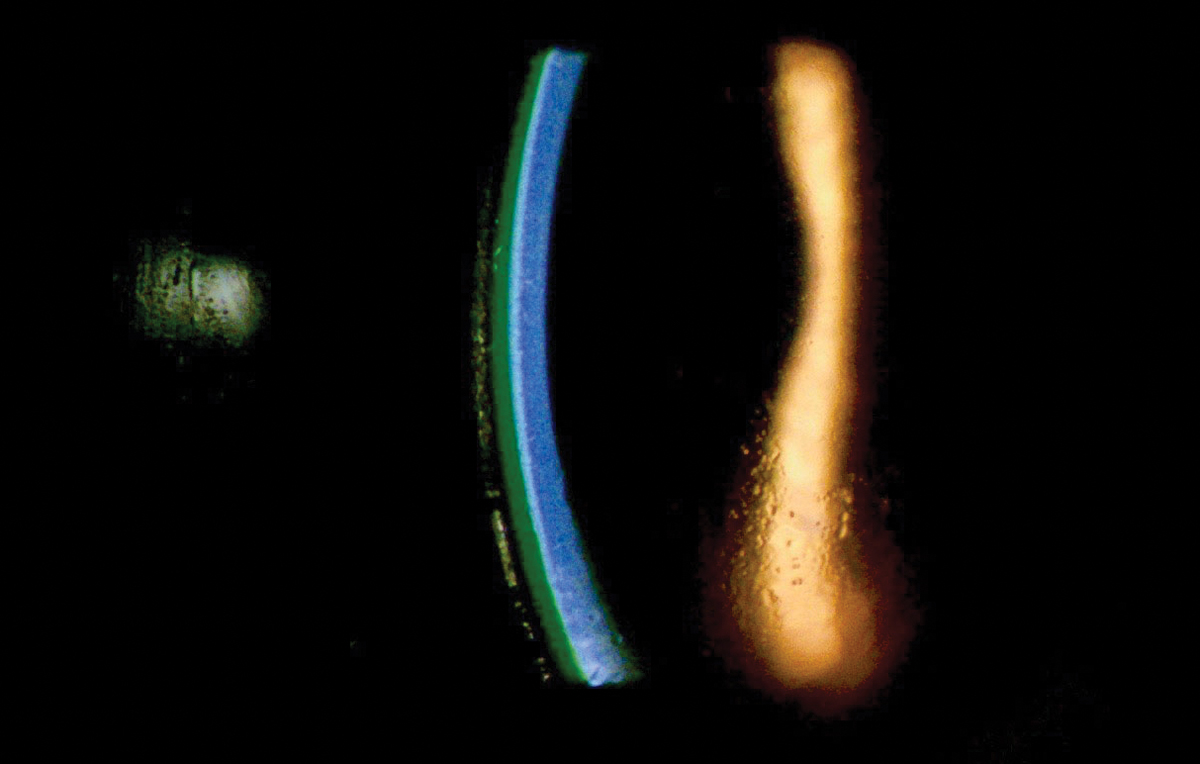 |
This slit lamp cross-section shows a posterior tear reservoir of approximately 250μm. Click image to enlarge. |
Physiological Considerations
Scleral lenses create a semi-seal surrounding their interface with the conjunctiva and sclera, resulting in limited tear exchange behind the lens. This is important, as the cornea obtains most of its oxygen from the atmosphere. A scleral lens is in effect a barrier between the cornea and its primary source of oxygen. This has been shown to cause corneal hypoxia, resulting in corneal swelling and edema.
The extent of corneal swelling is highly debated and is a main consideration when discussing the long-term health of scleral lens wear. A number of studies have observed varying amounts of corneal edema with scleral lenses, while others have found that corneal edema secondary to scleral lens wear is not as significant as originally thought.2,3
Lens Dk measures the oxygen permeability of a material; therefore, the easiest way to improve oxygen permeability is to choose a material with a high Dk. There are a number of suggested ideal Dk values for scleral lenses, with some studies recommending a Dk of 150 or higher.2 Although there are materials that boast Dk values of up to 200, there are other factors we must consider when selecting lens material,
Though difficult to measure, the wetting angle is an important consideration, especially as higher Dk materials often have a larger wetting angle. This may result in poor surface wetting, leading to dry eye and discomfort.4
A material’s wetting angle may decrease with the addition of Hydra-PEG coating (Tangible Science), which can be considered as a material enhancer, since it is part of the lens manufacturing process. This biocompatible polymer covalently bonds to the surface of the lens material to create a more consistent and durable coating.5 Originally introduced in 2017, it has been shown to improve lens comfort and dry eye symptoms and decrease lens fogging.6 It is now available with most gas permeable lens materials and may improve the experience for patients who are chronic depositors, suffer from dry eye or require a higher Dk lens.
Higher Dk materials typically have higher silicone content, increasing the likelihood of surface deposits, and a lower modulus, increasing the risk of lens flexure and resulting in irregular power changes and difficulty quantifying on-eye fitting relationships.
A higher Dk material may also have the opposite effect and result in lower oxygen transmissibility if we fail to take the refractive index into account and risk ending up with a thicker lens.
The relatively small range of refractive index options available for scleral lens materials (1.3 to 1.5) makes this factor less important when determining lens center thickness, unless you are dealing with a very high plus or high minus prescription.7 It has been argued that the ideal center thickness to prevent corneal edema falls between 250µm and 400µm.2 Keep in mind that designing a lens as thin as possible may actually result in unwanted lens flexure or warpage.
The recommended tear reservoir depth is another topic that is debated in the literature, and there are a number of suggestions ranging from 100µm to 200µm to minimize the risk of corneal edema.8 On the other hand, another study found no significant correlation between the post-lens tear reservoir and corneal edema.9 Despite these mixed recommendations, I typically strive for a post-lens tear reservoir of around 200µm six to eight hours post-insertion and consider this when selecting the ideal lens material.
Clinical ExamplesCase #1. A 66-year-old Caucasian female presented to our clinic inquiring about multifocal lens wear options. She expressed frustration about the lack of choices available for her visual needs. Her history included soft multifocal dropout, mild to moderate dry eye and a prescription consisting of +2.25-1.00x167 OD and +2.25-1.00x150 OS with an add power of +2.50. Due to the patient’s relatively small prescription, we opted to go with Optimum Extreme in an EasyFit multifocal lens design from Acculens and use Hydra-PEG coating to help address her dry eye. Unfortunately, she started to notice anterior surface deposits after the first three to four hours of wear. We switched to Optimum Extra with the same parameters. This lens performed much better, resulting in 10 to 12 hours of comfortable lens wear and stable vision. If the issue still had not resolved, we likely would have tried the same design but switched to Tyro-97 or Onsi-56 if Tyro-97 had also resulted in deposits. Case #2. A 29-year-old Caucasian female presented to our clinic asking about contact lens options to treat recurrent corneal erosion secondary to corneal epithelial dystrophy. Her history included chronic bandage contact lens use over the past three years and phototherapeutic keratectomy in the past nine months. Her main goals were to increase her vision, decrease the incidence of corneal erosions and improve her overall comfort. We chose to move forward with Optimum Infinite manufactured with Hydra-PEG coating in a Maxim scleral lens design from Acculens. We chose a higher Dk material to decrease hypoxic stress on the patient’s already damaged corneal surface. The initial few weeks of wear went well for the patient, and we continue to monitor how her cornea responds to chronic scleral lens wear while using this hyper Dk material. |
Material Options
Menicon Z, Optimum Infinite. Until recently, Menicon Z (tisilfocon A, Menicon) carried the highest Dk label at 163, leading to it earning FDA clearance for 30-day continuous wear. As it is made from a hyper Dk material, this lens has a slightly larger wetting angle, which could lead to decreased wettability.
Optimum Infinite (tisilfocon A, Contamac) is one of the newer lenses to hit the market. With a Dk of 180, structural stability and quality surface wettability, this lens has many of the characteristics we look for in a scleral lens.10 It may become a go-to lens option for many newer scleral patients regardless of their condition, especially those with multiple anterior surface comorbidities.
In addition to being offered in gas permeable lenses, tisilfocon A is a popular option for orthokeratology due to its FDA approval for use while sleeping. One study found no corneal endothelial morphology changes after a year of almost continuous wear.11
Optimum Extra and Extreme. These lenses work well for simpler designs and patients who have not demonstrated other corneal surface disease. Optimum Extra (roflufocon D and E, Contamac) offers a Dk of around 100 and an extremely low wetting angle of 3°, while Optimum Extreme (roflufocon D and E, Contamac) has a Dk of around 125 and a wetting angle of around 6°.10 Based off these characteristics and its proven machinability and strong modulus, Optimum Extra seems to be the material of choice between the two for many seasoned clinicians.
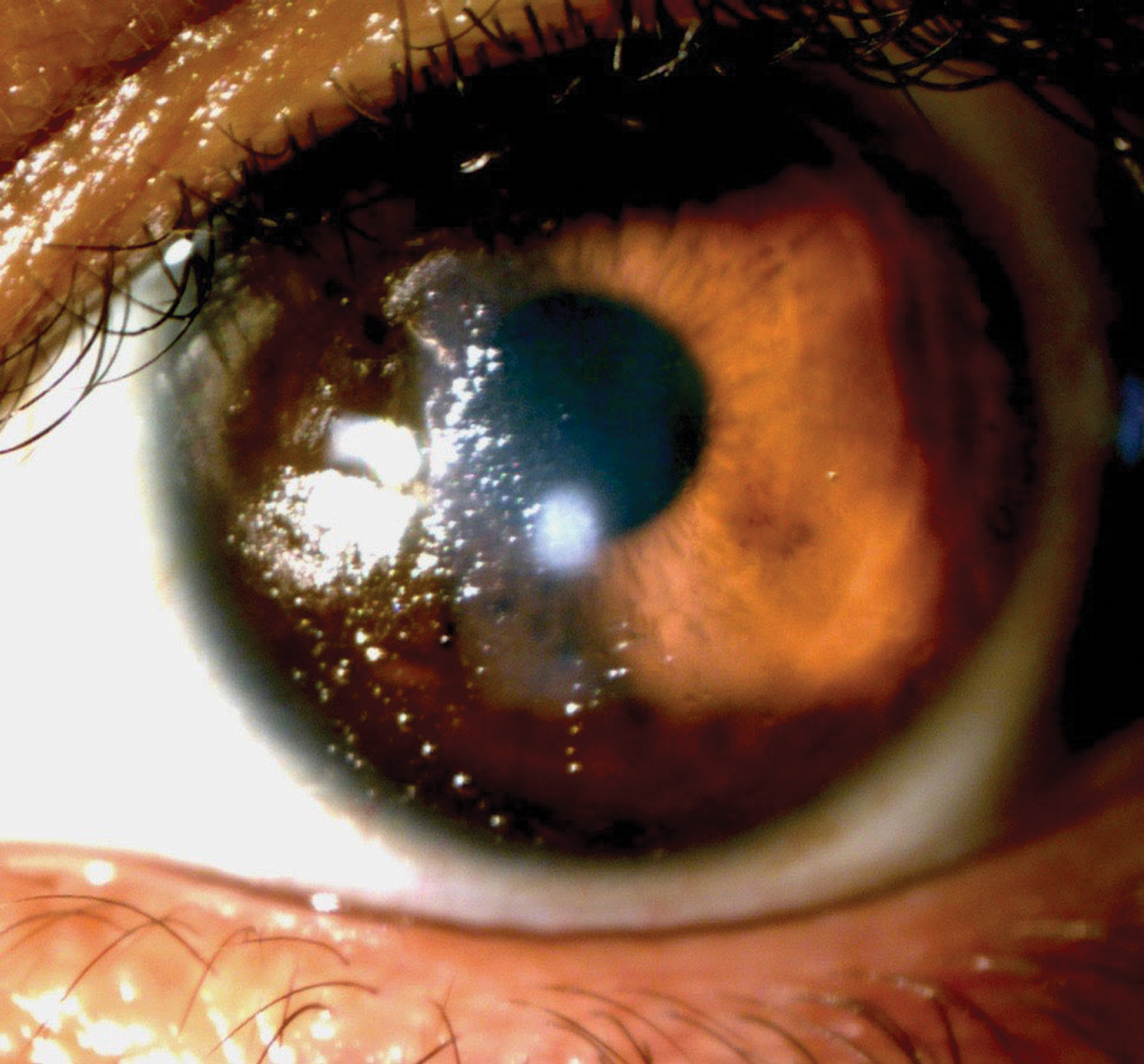 |
| Poor wetting is seen nasally with this scleral lens. Click image to enlarge. |
Acuity 200. This lens offers a hyper Dk of 200 and is currently only available outside of the United States, though it is working its way through the FDA approval process. Acuity 200 (fluoroxyfocon A, Acuity Polymers) has been commended “for its ability to solve challenging specialty lens cases, particularly in the areas of irregular cornea and diseased eyes.”12
Acuity 100, Boston XO. Both lenses offer a high Dk of 111, making them viable options for most scleral lens users. However, Acuity 100 (hexafocon A, Acuity Polymers) and Boston XO (hexafocon A, Bausch + Lomb) may not perform as well for dry eye patients, due to their material’s higher wetting angle of around 49°.13
Boston XO2. This lens offers a hyper Dk of 141, which is ideal for oxygen permeability, but it has a higher wetting angle of 38° and a lower modulus of 1,160MPa.14 This means Boston XO2 (hexafocon B, Bausch + Lomb) may perform well for patients who require a higher Dk but not as well for those who are depositors, have dry eye or have prescription requirements that may promote lens flexure. Hydra-PEG coating may improve the dryness and depositing issues previously seen with hexafocon B.
Tyro-97. This is a good entry-level scleral lens with its relatively high Dk of 97. Tyro-97 (hofocon A, Lagado) is marketed for its higher Dk, high strength factor and hydrophilic properties that create a wetter surface for improved tear film interaction.15
Onsi-56. This lens’ lower Dk of 56 makes it a less-than-ideal solution for scleral lens fitting. Monitor corneal endothelial cell counts and pachymetry closely if prescribing this lens. That being said, Onsi-56 (onsifocon A, Lagado) could work wonders for patients who have a history of deposits and dry eye when fit with higher Dk materials.15
As scleral lenses become more popular, it is becoming increasingly important to understand the fitting characteristics associated with each lens material, especially if you are looking to expand your specialty lens practice. These patients often have higher expectations and shorter patience due to a lifetime of managing a debilitating visual condition. Choosing the right material at the beginning of the process can make a world of difference for them.Dr. Persson is a partner in a multi-location optometric practice in Denver, CO, where he founded the Scleral Contact Lens Institute. He is a 2013 graduate of the Ohio State University College of Optometry.
1. Romero-Rangel T, Stavrou P, Cotter J, et al. Gas-permeable scleral contact lens therapy in ocular surface disease. Am J Ophthalmol. 2000;130(1):25-32. 2. Michaud L, van der Worp E, Brazeau D, et al. Predicting estimates of oxygen transmissibility for scleral lenses. Cont Lens Anterior Eye. 2012;5(6):266-71. 3. Vincent SJ, Alonso-Caneiro D, Collins MJ, et al. Hypoxic corneal changes following eight hours of scleral contact lens wear. Optom Vis Sci. 2016:93(3):293-9. 4. Bennett ES, Henry VA. Clinical Manual of Contact Lenses, 4th ed. Philadelphia: Lippincott Williams and Wilkins; 2014:94. 5. Tangible Science. Eye care professional resources. tangiblescience.com/tangible-hydra-peg-toolkit/. Accessed August 12, 2020. 6. ClinicalTrials.gov. Tangible Hydra-PEG: a promising solution for scleral lens wearers with dry eye. clinicaltrials.gov/ct2/show/NCT03417505. Accessed August 12, 2020. 7. Coronis T. 20/20 Magazine. Winning the high-index numbers game. Published July 2009. www.2020mag.com/article/winning-the-high-index-numbers-game. Accessed August 12, 2020. 8. Jaynes JM, Edrington TB, Weissman BA. Predicting scleral GP lens entrapped tear layer oxygen tensions. Cont Lens Anterior Eye. 2015;38(1):44-7. 9. Tan B, Zhou Y, Yuen TL, et al. Effects of scleral-lens tear clearance on corneal edema and post-lens tear dynamics: a pilot study. Optom Vis Sci. 2018;95(6):481-90. 10. Contamac. Optimum Infinite. www.contamac.com/product/optimum-infinite. Accessed August 12, 2020. 11. Barr JT, Pall B, Szczotka LB, et al. Corneal endothelial morphology results in the Menicon Z 30-day continuous-wear contact lens trial. Eye Contact Lens. 2003;29(1):14-6. 12. Acuity Polymers. GP materials. www.acuitypolymers.com/gp-materials/acuity-materials. Accessed August 12, 2020. 13. Bausch + Lomb. Boston materials. www.fit-boston.eu/downloads/other/B-L_Boston_Materials_Presentation.pdf. Accessed August 12, 2020. 14. Bausch + Lomb. Boston XO2. bauschgp.com/lens-material/boston-xo2.html. Accessed August 12, 2020. 15. Lagado Corp. Premium GP materials. www.lagadocorp.co/products/premium-gp-materials. Accessed August 12, 2020. |


