 |  |
Oftentimes, your most loyal patients are those who believe that you would go above and beyond to meet their visual needs appropriately while still allowing them to wear contact lenses. In turn, they’re more than willing to refer others to you without a second thought or any type of incentive.
We can take patient satisfaction a step further when handling particularly challenging cases that require specialty care and advanced knowledge. Here, we discuss several examples of oddball ocular surface issues among contact lens wearers and how to appropriately address them to optimize the patient experience.
Post-refractive Surgery
These corneas typically have a lower sagittal depth than normal because the central cornea is thinned and flattened during the refractive procedure, whether it be photorefractive keratectomy, laser-assisted in situ keratomileusis or laser-assisted epithelial keratomileusis. Although radial keratotomy doesn’t thin the cornea, it does alter its architecture. As such, if suboptimal refractive results occur with any refractive procedure, resulting in an irregular corneal surface, it becomes very difficult to fit these patients with standard soft contact lenses. These lenses often vault over the surgically altered cornea, leading to vision that is clear shortly after blinking but becomes blurrier as the eye remains open.
Post–refractive surgery patients require contact lenses with a lower sagittal depth to mitigate the vaulting. This is difficult to achieve with standard soft contact lenses, but other options are available for these types of corneas. Reverse-geometry gas permeable (GP) lenses provide a flat central curve that transitions to a steeper peripheral curve joined by a reverse curve. Hybrid and scleral lenses can also optimize vision for these surgically altered corneas. When fitting scleral lenses, be cognizant of the need to establish appropriate clearances over post-refractive corneas, as these patients tend to have excessive central corneal clearance.
Progressive Keratoconus
This clinical condition can range in severity. Early on, mild corneal thinning causes a protrusion of the cornea in the area of thinning. As the condition progresses, further thinning and steepening of the cornea occur, increasing the sagittal depth of the cornea and creating irregular astigmatism. Keratoconic eyes have a hard time succeeding with standard soft contact lenses.
Earlier on in the condition, the irregular astigmatism may be correctable with a standard soft toric contact lens. However, as the condition progresses, you can prescribe specialty soft contact lenses, such as KeraSoft (UltraVision) and Novakone (Bausch + Lomb). GP and standard hybrid lenses are also options. As corneal steepening begins to take place, it’s likely that you’ll need to turn to specialty hybrid lenses, including UltraHealth (SynergEyes), and scleral lenses to correct for the irregular cornea. Discuss corneal crosslinking with progressive keratoconus patients when necessary.
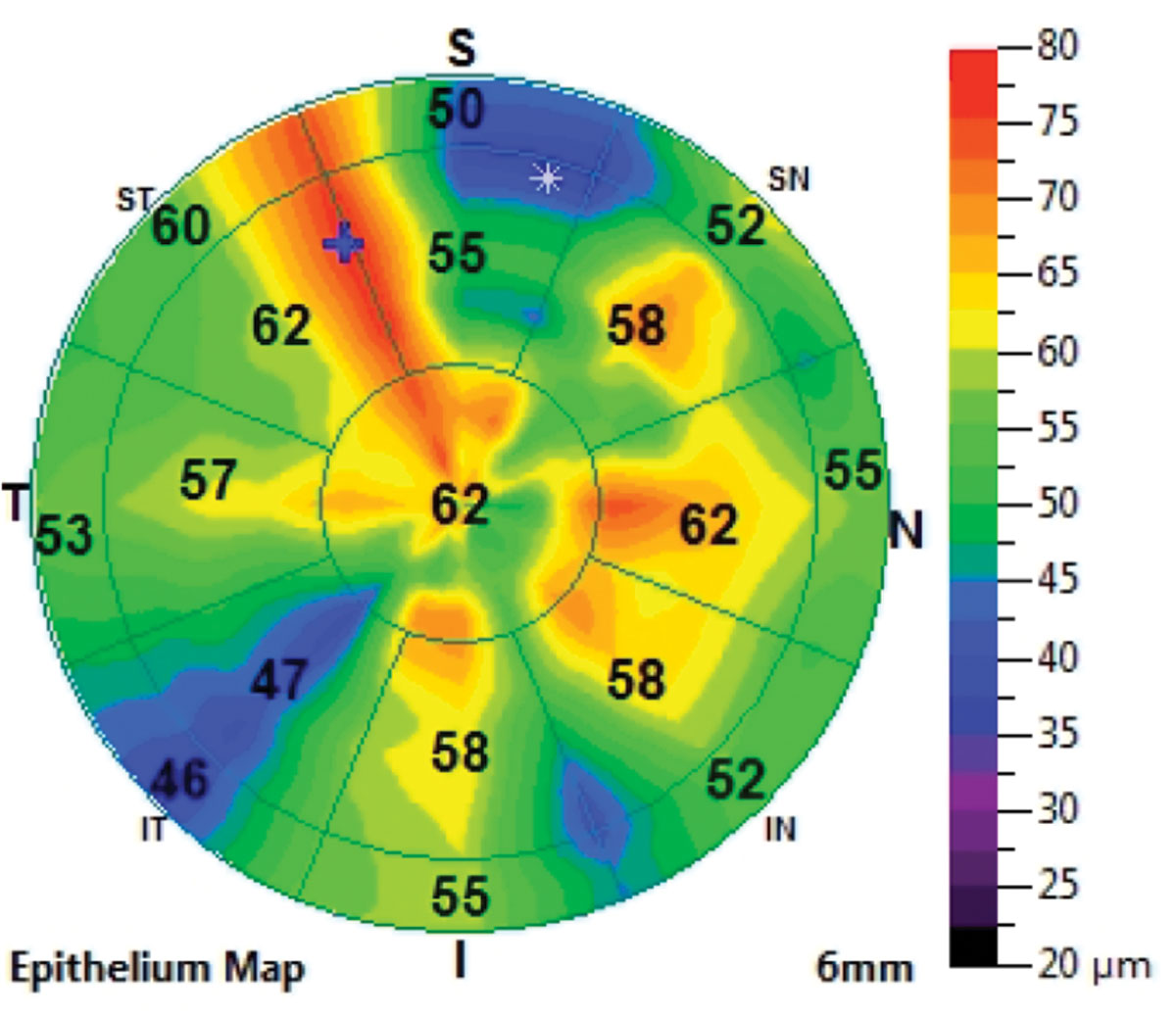 |
| Irregular thickness secondary to a corneal injury can cause an irregular surface. Click image to enlarge. |
Irregular or Scarred Cornea
Injuries and infections can cause permanent architectural changes to the cornea that may affect the cornea’s shape and clarity. They can also permanently alter the corneal epithelial thickness, creating additional abnormalities to the ocular surface. Depending on the level of irregularity present, a high-modulus silicone hydrogel lens may mask these abnormalities. GP, hybrid and scleral lenses are also all options.
High Astigmatism
Moderate corneal astigmatism can be adequately corrected with soft toric lenses. The technology, contemporary design and wide range of disposable options provide a reliable, predictable fit. As corneal astigmatism increases and becomes the main refractive error causing visual disturbance, however, it becomes increasingly difficult to correct with soft toric lenses. Smaller rotations of soft toric lenses create greater changes with higher amounts of astigmatism, oftentimes compromising it. This is where GP designs come into play and provide superior vision.
A tear lens is created between the posterior surface of a GP lens and the cornea to correct the corneal astigmatism. If the astigmatism is centrally located, high amounts may be correctable with a standard spherical lens. If the corneal astigmatism extends closer to the limbus, the lens is at greater risk of flexure, which ultimately compromises the patient’s vision by correcting less of the corneal astigmatism. By fitting the cornea with a back-toric GP lens, the lens toricity is designed to match the corneal toricity, mitigating lens flexure and optimizing vision.
Of course, don’t forget about the option of scleral contact lenses, which are typically made at a thickness of between 300μm to 400μm centrally to provide a surface that resists flexure. This creates a predictable tear lens for patients with regular astigmatism. Those patients whose corneal astigmatism is similar to their refractive astigmatism tend to see very well with scleral lenses. Keep in mind that regular astigmatism can extend onto the sclera as well, so make sure to appropriately align the landing zone of the lens with the scleral shape by designing the lens with the appropriate toricity.
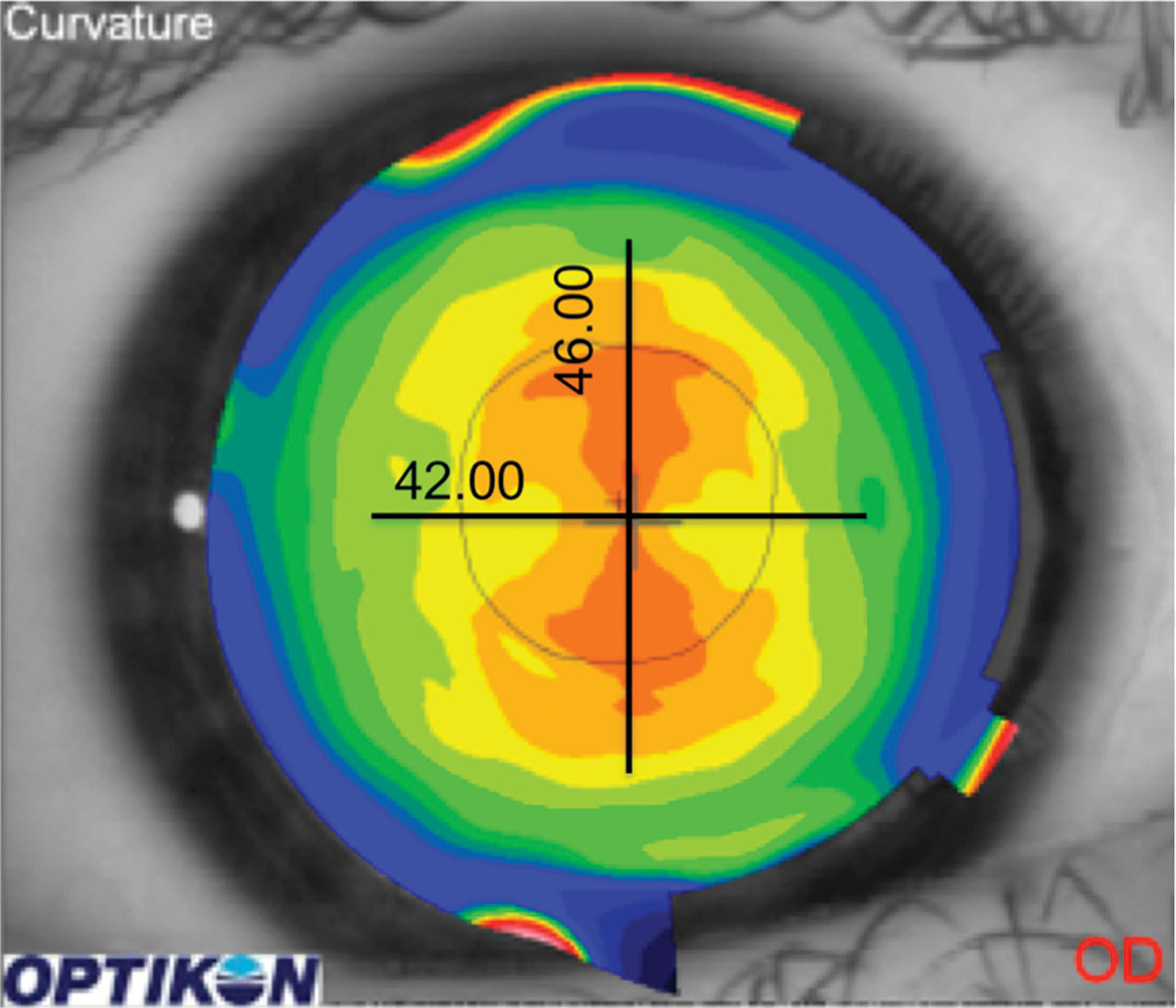 |
| Centrally located astigmatism can often be fit with a spherical GP lens. Click image to enlarge. |
Irregular Scleral Shape
A decade ago, discussion about the importance of the shape of the sclera was just starting to emerge. We used to be limited to scleral lenses with a spherical landing zone that caused unintended consequences, such as discomfort, more lens awareness in certain regions where the lens lifted away from the sclera, impingement in areas where the landing zone was steeper than the scleral profile and post-lens tear clouding throughout the day.
It is critical to understand the relationship between the landing zone of the lens and the often irregular scleral shape. There are technologies that guide clinicians in measuring the scleral profile and producing the appropriate landing zone on the lens. Many scleral lens diagnostic sets now come with a standard toric landing zone. This provides the practitioner with the added advantage of an adequate starting point that may require only minor modifications to optimize the landing zone.
Oddball ocular surfaces present unique challenges to clinicians as they work to restore appropriate vision. Keep these examples and fitting strategies in mind when managing tricky cases. Your patients and your practice are sure to benefit.


