For those patients who have suffered vision loss from keratoconus, contact lenses usually provide optimal visual rehabilitation and remain our first-line therapy given their versatility and low risk, as discussed in Part 1 of this two-part article (published in the Nov/Dec 2021 issue). Many of the lens modalities discussed in Part 1—scleral, corneal, soft contact, specialty soft, piggyback and hybrid—are also viable options after keratoconus surgical procedures, as the cornea will likely still have some irregularities that impact vision and are not amenable to spectacle correction. Some of these surgical procedures, such as corneal collagen crosslinking (CXL) and intrastromal corneal ring segments (ICRS), are intended to halt progression and reduce some of the ectasia, thereby making contact lens fitting easier.
When a keratoconus patient has become intolerant of contact lenses, has visually compromising scars or corneal perforation, a full or partial keratoplasty is recommended. In 2016, the Eye Bank Association of America reported that keratoconus was the most common indication for penetrating keratoplasty (PKP) in the United States and 6,195 transplants are performed each year.1 Fortunately, advancements in contact lens technology and the introduction of CXL have reduced the incidence of PKP over the years.
When to initiate contact lens therapy after a procedure depends on the type of procedure and the eyes’ response to healing. When fitting, monitor the state of the corneal tissue. As these are more “fragile” corneas, it is important to use high oxygen permeable materials, schedule more frequent observation and emphasize compliance to reduce complications.
In Part 2 of this two-part article, we’ll discuss in detail these surgical interventions and post-procedure contact lens fitting, including the application of scleral lens fitting.
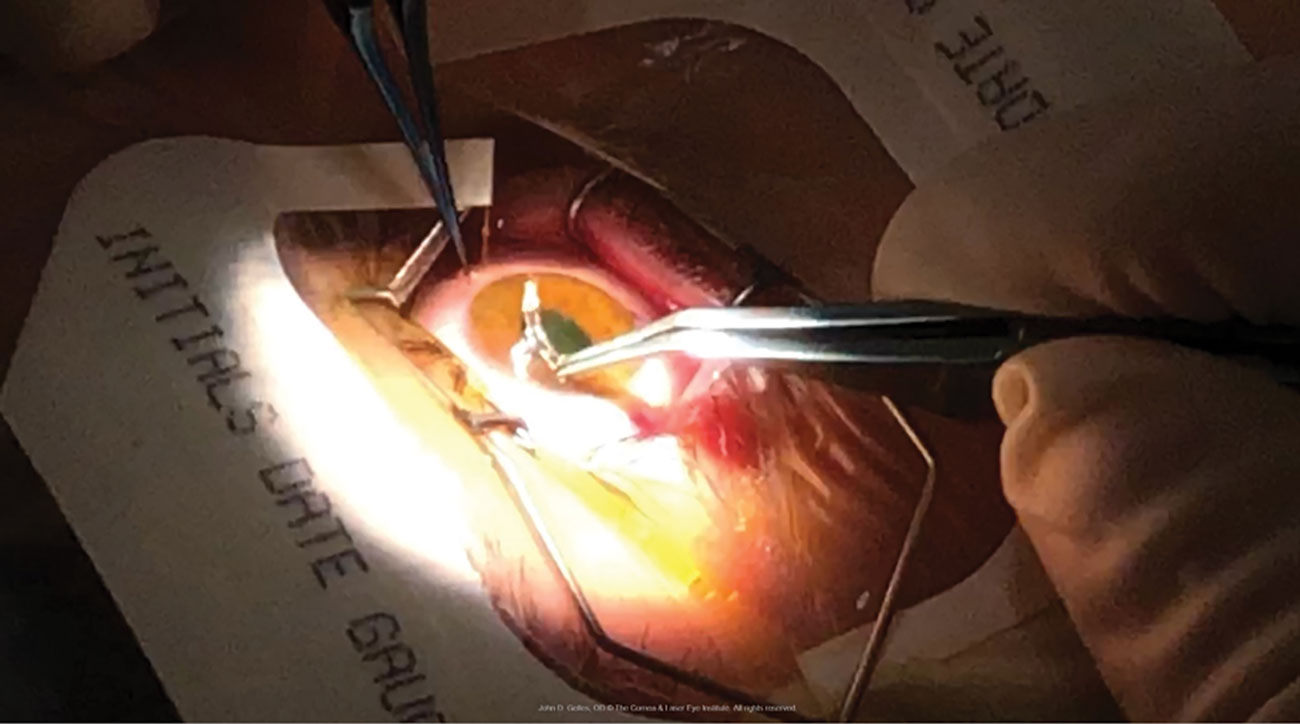 |
An ICRS is placed into an intrastromal channel immediately after undergoing CXL. Note the riboflavin-induced yellow hue of the cornea. Photo credit: John Gelles, OD. Click image to enlarge. |
Corneal Collagen Crosslinking
Improved technology and early diagnosis have led way for earlier surgical intervention so that patients do not have to succumb to corneal transplantation. In 2016, the FDA approved the Avedro KXL System and Photrexa for CXL. The procedure is intended to both strengthen and stabilize an ectatic cornea by applying riboflavin (vitamin B12) and controlled UV light. It is indicated for corneas over 400µm thick that have shown progression of keratoconus or post-surgical ectasia. The eye must be free of scars, herpetic infection, autoimmune disease and wound healing issues.
Some interesting studies came out of the recent pause in elective procedures due to the COVID-19 pandemic. A paper by Shah et al. in the UK demonstrated that in their study, all 46 subjects with progressive keratoconus worsened during the wait time to receive treatment.2 Goh et al. showed a similar finding in New Zealand with 39.6% of 96 eyes further worsened.3
Early intervention with CXL is critical to achieve maximum benefit from the procedure, but the postoperative management is crucial. In the US, the ‘epi-off’ technique, which requires epithelial debridement prior to riboflavin application, is the only approved procedure. It also requires the use of a soft therapeutic bandage lens for seven to 10 days following surgery while the surface heals. However, the epithelium continues to strengthen and the stroma remodels for several months; therefore, this tissue must be respected.
The epithelium remains fragile for several months to a year with increased apoptosis and changes in thickness and density, which may alter visual acuity likely due to induced higher-order aberrations. The corneal nerve plexus is also altered, reducing sensitivity for up to a year, making it critical for the clinician to monitor carefully for ocular surface damage, even though the patient may be asymptomatic. Finally, stiffening and remodeling of the stroma leads to curvature changes for several months, so be aware that modifications may be needed to provide optimal vision and the healthiest outcome.4-7 This may necessitate the use of pre-procedure spectacle wear for five to six weeks to avoid any damage and allow for full recovery.
Many patients achieve better spectacle visual acuity after CXL, but most will still require a specialty contact lens design. Because diagnostic tools allow earlier diagnosis and the opportunity to halt progression with CXL, patients can benefit from more options for optical corrections, especially spectacles, soft lens designs and hybrid lenses, as their disease status may stay in the mild to moderate phase. Patients may be anxious to be fit or refit into contact lenses, but it’s important to stress that rehabilitation may take time to get the safest and optimal fit and the fitting process may begin around one to two months following the procedure.
Higher Dk soft lenses may be fit, but careful observation for signs of hypoxia is important; also, lens stability is often challenging. Rigid corneal lenses are an option, but the fit may be delayed or require multiple modifications to avoid landing on the cornea during the postoperative months while it is in transition. It may be safer and require fewer re-fits if the prescriber monitors the topography until stability is achieved.
Hybrid lenses can be considered, as they should vault the corneal tissue approximately 100µm, which will maintain corneal integrity, and the newer designs emphasize landing on the sclera rather than GP portion; however, timing is still crucial. Many of these patients may present as scleral lens wearers, and their habitual design can be re-established much sooner—likely within a month, since the surface does not come into contact with the lens. During the first few months following the procedure, the cornea undergoes a series of changes that may necessitate modifying the scleral lens fit and power; therefore, proper patient education is essential.
As discussed, much of our attention should be directed to the ocular surface and lens designs that touch the cornea should be avoided until the epithelium is healed. Some of these patients will be novice lens wearers and inadvertently self-inflict mild trauma to the surface; take heed of their need for additional training.
Between improvements in CXL as the technology matures and potentially better outcomes from ‘epi-on’ procedures (where the cornea remains intact) with supplemental oxygen, there is hope that contact lens management can be initiated sooner for this population, as the procedure will become more accepted and available.
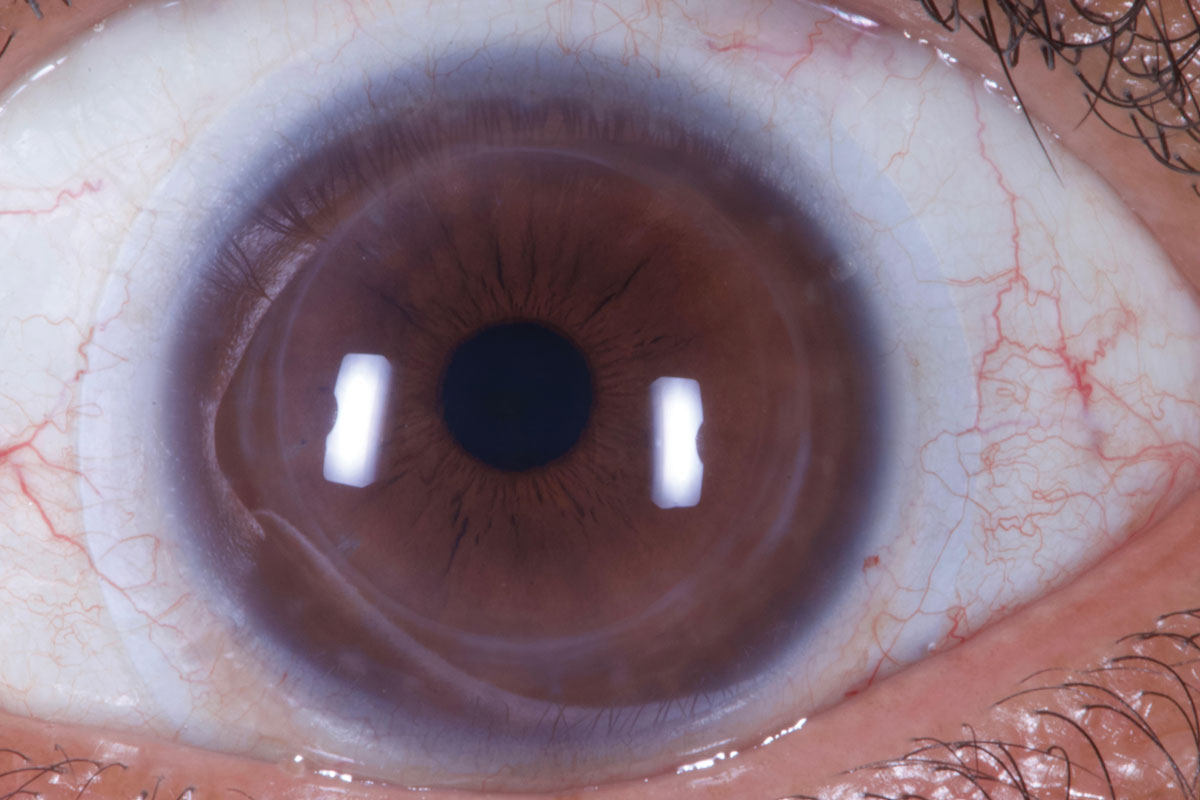 |
A scleral lens over an eye post-ICRS. Photo credit: Tom Arnold, OD. Click image to enlarge. |
Intracorneal Ring Segments (ICRS)
These implants are used to flatten corneal curvature and reduce or create more “regular” astigmatism. Often, it is done in combination with CXL to help maintain the effect. There are many different approaches to this procedure with regard to the number of segments and location, and the outcomes vary.8 Undercorrection, overcorrection or residual refractive error can be remedied with optical devices; however, more serious complications need to be monitored during the long-term post-op phase. Some of these include neovascularization toward the incision, migration of a segment toward the wound, extrusion of the segment, stromal deposits, epithelial ingrowth and flap wrinkling.
Many times, there is elevation at the ring site; it is important to respect the tissue overlying the inserts and not allow too much touch or pressure from a lens. The contact lens practitioner must monitor the ICRS position, as mechanical trauma can cause the implants to erode at the insertion site or migrate forward. We must also document inflammation and deposits, since we may be the only professional monitoring these findings during the postoperative phase. Complications from the ring and/or contact lens must be monitored, since the insertion site can serve as an entry point for bacteria and lead to serious microbial keratitis, necessitating explantation of the device.
The goal of the procedure is for the topography to be “normalized” so that spectacles or soft toric lenses can correct these eyes if the astigmatism becomes more regular and shifted towards the central visual axis.9 Other patients will benefit from larger diameter corneal rigid lenses or hybrid lenses that have reverse geometry curves and can accommodate an oblate cornea. If a smaller diameter corneal GP is used, a tandem system with high Dk soft base can provide protection of the underlying ring. Undeniably, scleral lenses are an excellent option as they are easy to vault and protect the corneal tissue.10,11
Do not create too much clearance on these oblate corneas, though, as this can lead to hypoxic stress. Many patients who have been offered and underwent ICRS procedures are given the expectation that they will not require contact lenses. While it is true that spectacle vision is improved, most patients will still benefit most from the optics of a contact lens.12
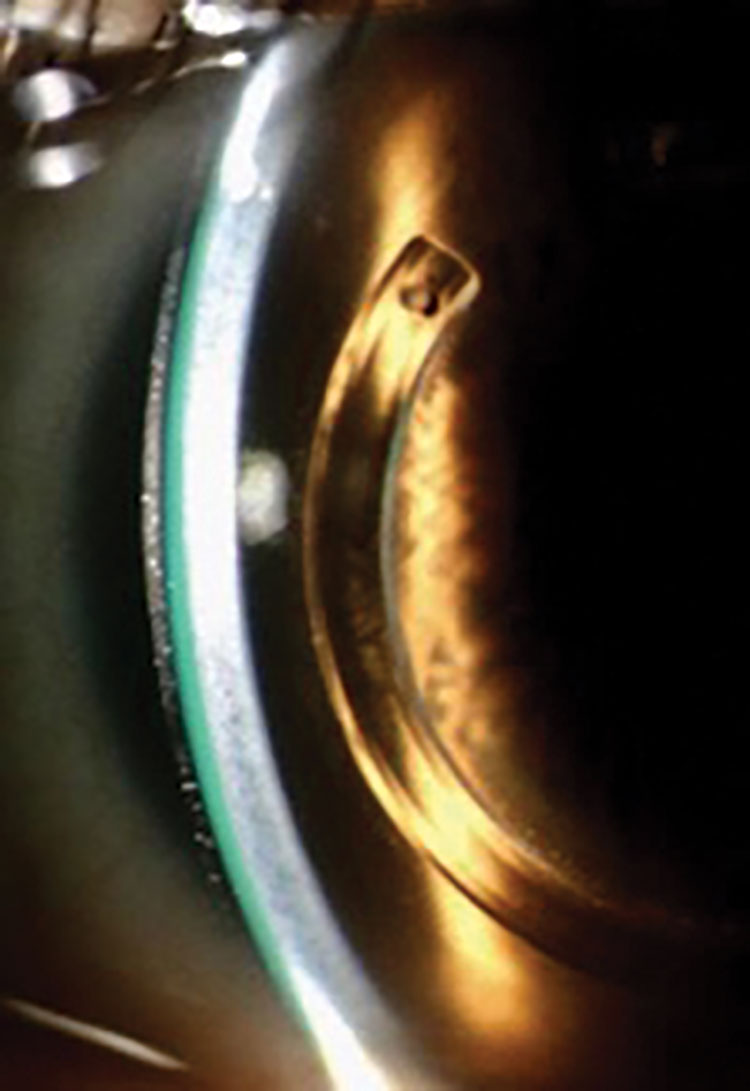 |
A scleral lens over an eye post-ICRS. Photo credit: Tom Arnold, OD. Click image to enlarge. |
Keratoplasty
Corneal transplantation procedures are typically reserved for advanced keratoconus or eyes that have suffered trauma, endothelial disease or scarring from infection. The recuperation process is much longer and complicated than the procedures listed above, as it requires the integration of donor tissue.
Postoperative astigmatism is very common; however, the sutures can be manipulated during various stages of the healing process to provide a more regular surface and ease the fitting process. The surgeon must determine proper diameter of the donor graft—usually 0.50mm larger than the recipient bed. It should be large enough to avoid the visual axis, yet small enough to avoid interaction with the limbal vessels so as not to promote rejection. Some surgeons may opt to go only 0.25mm larger so that, as the eye heals, the adhesion between host and donor causes stretching, leading to flattening that can increase hyperopia or decrease myopia, which may be a desired effect.
Typically, there are six to eight interrupted sutures placed during surgery to hold the tissue in place; these may be removed starting at three months after the procedure. An additional running or continuous suture at 45 or 90 degrees that encircles the cornea creates tension, promotes host-donor integration, can be altered early to change the tension and is typically removed after one year.
During the early phases, if an excessive amount of astigmatism is present, selective removal or loosening of the sutures can reduce it. A tight suture can be found in the plus cylinder axis and one can decrease the chord and radius of curvature to reduce toricity. A loose suture can be found in the minus cylinder axis and one can increase the chord and radius of curvature to reduce toricity. This may also be the location of edema or wound gap and may be transient or more serious. These points are mentioned because the fitting of a contact lens following a PKP may be dependent on the topography of the cornea. If modifications can be made early on, the long-term success can be improved by co-managing these opportunities.
 |
A well-fit scleral lens over an eye that has undergone a corneal transplant. Photo credit: Tom Arnold, OD. Click image to enlarge. |
It is important to set expectations for patients prior to surgery. Based on the type of procedure (full penetrating, partial lamellar or eccentric tectonic), etiology and surgical techniques, the outcomes may vary. Some patients may achieve success in spectacles; others will require contact lenses to attain the best visual outcome. It is safe to fit lenses at about 12 months after the procedure; however, many patients and surgeons desire earlier fitting (e.g., at six months) and this can be done as long as the following criteria are met:
• the cornea displays intactness of the wound
• antibiotic treatment is complete
• steroid use is minimal
• refraction and topography are stable
• the patient is psychologically ready
The latter is included because many patients are reluctant to interfere with their “new eye.” Many of these patients will require a contact lens, as irregular astigmatism is common. Typically, these surfaces require some form of a rigid design, and it is very important to respect the corneal host-graft junction. Most often, these patients have worn some form of contact lenses prior to surgery, so adaption is easy, but the ideal modality may differ from patient to patient.
Remember that the goal is to improve vision without doing any harm. Prior to the fit, make sure to document any remaining sutures, neovascularization, scars or erosions to rule out any contact lens-induced complications. Based on the healing, sutural technique and donor tissue, many graft topographies can result:
• a steep or proud graft is similar to a central keratoconus
• a tilted graft will result in local, eccentric ectasia
• a sunken graft may be more oblate in shape with a flat center and raised areas near the junction similar to a post-RK cornea
A rigid lens will center over the steepest part of the cornea, and since some of these eyes have irregular pupils, larger optical zones are needed to improve centration and reduce flare. Some benefit from fitting inside the graft, while others will find it easier to land on the peripheral host cornea or on the sclera. Smaller corneal GPs are often a challenge; larger intra-limbal designs are preferred so that they can rest on the host tissue. Scleral lenses avoid all corneal interaction, and hybrid designs for post-surgical corneas are also an option.
In general, when fitting patients who have undergone corneal transplantation, we must monitor not only the superficial cornea and respect the junction but also maintain the integrity of the endothelial layer to achieve optimal deturgescence. Pachymetry is essential, and endothelial cell counts can aid in determining continue viability of the graft tissue. It is also very helpful to monitor intraocular pressure, as many of these patients remain on steroids long-term. Although our focus is on the maintenance of the transplant, we must remember that it is attached to the rest of the eye and human body where many comorbidities exist, thereby optometrists are part of the transplant team for life.
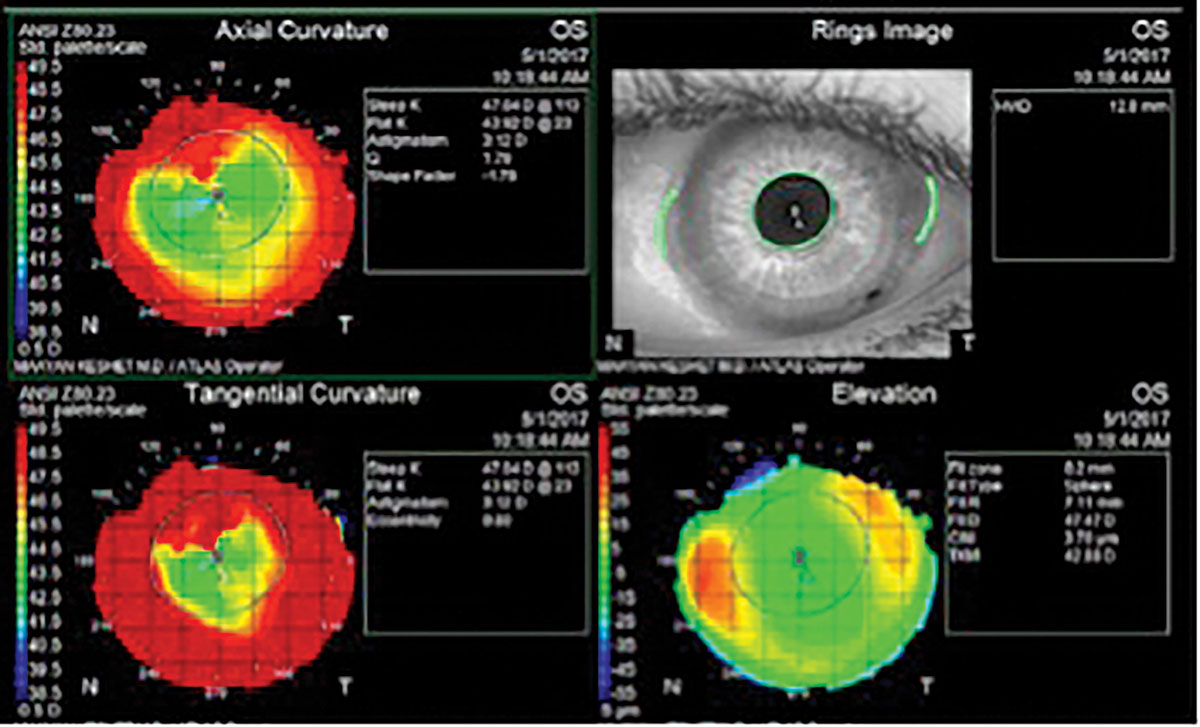 |
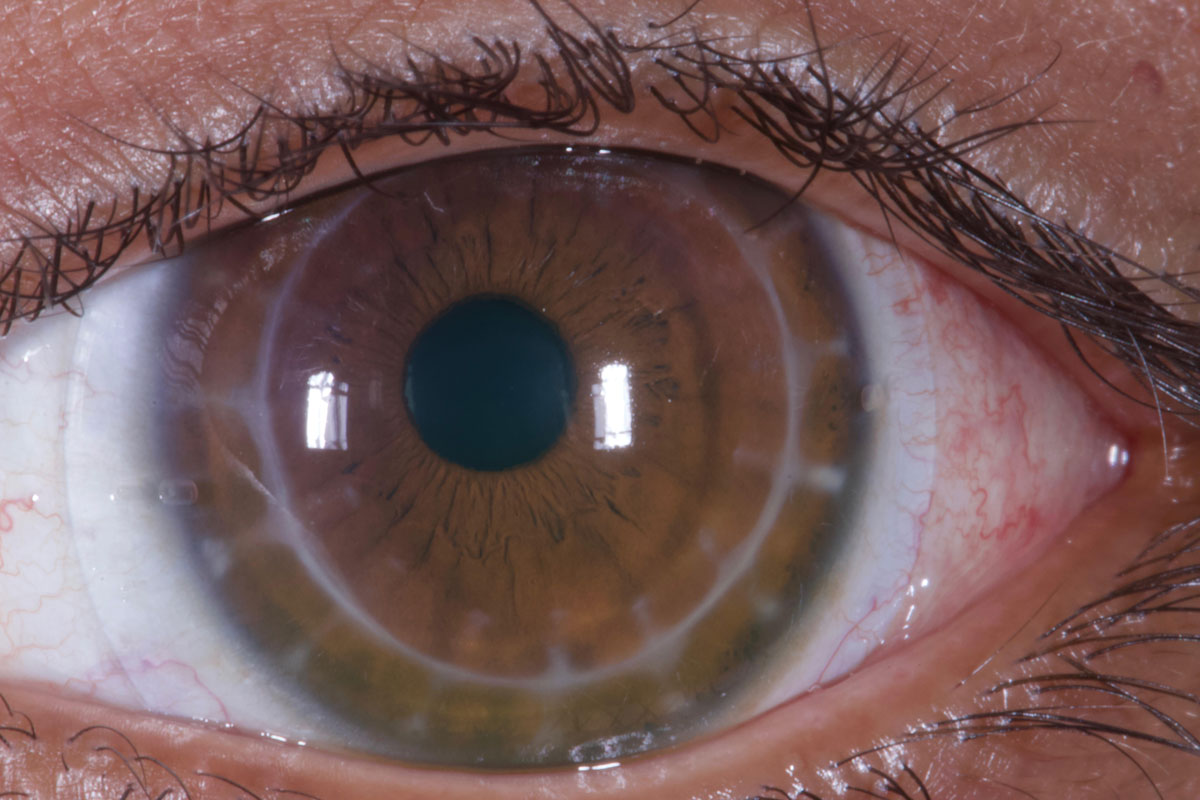
Topography shows relative central flat and steep periphery (reverse geometry) in a post-PK cornea. This patient was fit into an oblate-shaped (steep skirt) hybrid lens. Photo credit: Beth Summers, OD, and Maayan E. Keshet, OD. Click image to enlarge. |
Contact Lenses at the Core of KCN
Keratoconus patients are fortunate to have many interventions available that can induce long-term changes that lessen the disease’s visual burden. Medical management of disease progression from the procedures discussed above has already shown to have a positive impact on the natural course of the disease. ICRS, topography- and tomography-guided PRK all aim to reduce disease severity via their impact on corneal shape and thus both uncorrected and best- corrected visual acuity.
Still, to this day, the mainstay of visual rehabilitation and improved function for those who have suffered vision loss from keratoconus is contact lenses. They are relied on early in the disease course when surgery isn’t yet advisable and complete “the last mile” even after successful procedures have taken place. Each case should be evaluated individually to come up with the most appropriate contact lens treatment.
 |
| Click image to enlarge. |
Dr. Barnett is a principal optometrist at the Univ. of California, Davis Eye Center. She is chair of the AOA’s Contact Lens and Cornea Section, a fellow of the American Academy of Optometry, a diplomate of the American Board of Certification in Medical Optometry, a fellow and global ambassador of the BCLA and a board member of the GPLI and the International Society of Contact Lens Specialists. Dr. Barnett has consulting and/or lecturing relationships with ABB, Acculens, Bausch + Lomb, Contamac, CooperVision, EveryDay Contacts, Johnson & Johnson Vision Care, SynergEyes and Tangible Science.
Dr. Eiden is president and medical director of North Suburban Vision Consultants, president and founder of the International Keratoconus Academy of Eye Care Professionals and co-founder and president of EyeVis Eye and Vision Research Institute. He is a fellow of the American Academy of Optometry and the Scleral Lens Education Society. Dr. Eiden has consulting, lecturing and/or financial interests with the following companies: Alcon, Avellino, Bausch + Lomb, CooperVision, Oculus, Special Eyes, SynergEyes and VTI.
Dr. Sclafani is vice president of professional affairs for SynergEyes and sees patients at SoLo Eyecare in Chicago and the Illinois College of Optometry. She is a fellow of the Scleral Lens Society and associate member of the International Society of Contact Lens Specialists. Dr. Sclafani is vice president of professional affairs at SynergEyes.
1. Eye Bank Association of America 2016 Eye Banking Statistical Report. www.restoresight.org/wp-content/uploads/2017/04/2016_Statistical_Report-Final-040717.pdf. Accessed January 25, 2022. 2. Shah H, Pagano L, Vakharia A, et al. Impact of COVID-19 on keratoconus patients waiting for corneal crosslinking. Eur J Ophthalmol. 2021;31(6):3490-3. 3. Goh YW, Gokul A, Yadegarfar ME, et al. Prospective clinical study of keratoconus progression in patients awaiting corneal crosslinking. Cornea. 2020;39(10):1256-60. 4. Lombardo M, Serrao S, Rosati M, et al. Biomechanical changes in the human cornea after transepithelial corneal crosslinking using iontophoresis. J Cataract Refract Surg. 2014;40(10):1706-15. 5. Del Buey MA, Lanchares E, Cristóbal JÁ, et al. Immediate effect of ultraviolet-a collagen cross-linking therapy on the biomechanics and histology of the human cornea. J Refract Surg. 2015;31:70-1. 6. Li Z, Wang Y, Xu Y, et al. The evaluation of corneal fragility after UVA/riboflavin crosslinking. Eye Contact Lens. 2017;43(2):100-2. 7. Ozgurhan EB, Celik U, Bozkurt E, Demirok A. Evaluation of subbasal nerve morphology and corneal sensation after accelerated corneal collagen cross-linking treatment on keratoconus. Curr Eye Res. 2015;40(5):484-9. 8. Szczotka LB, Lindsay RG. Contact lens fitting following corneal graft surgery. Clin Exp Optom. 2003 Jul;86(4):244-9. 9. Moreira LB, Bardal RA, Crisigiovanni LR. Contact lenses fitting after intracorneal ring segments implantation in keratoconus. Arq Bras Oftalmol. 2013;76(4):215-7. 10. Park J, Gritz DC. Evolution in the use of intrastromal corneal ring segments for corneal ectasia. Curr Opin Ophthalmol. 2013;24(4):296-301. 11. Montalt JC, Porcar E, España-Gregori E, Peris-Martínez C. Visual quality with corneo-scleral contact lenses after intracorneal ring segment (ICRS) implantation for keratoconus management. Contact Lens Anterior Eye. 2019;42(1):111-6. 12. Szczotka-Flynn LB. Research review: How intracorneal rings affect lens fitting for keratoconus. Contact Lens Spectrum. May 1, 2010. Accessed January 30, 2022. |


