Irregular astigmatism can arise from a multitude of causes, and a variety of different lens designs can help manage it. Nonetheless, most practitioners consider gas permeable (GP) lenses the standard of care for rehabilitating vision due to irregular astigmatism. A GP-type lens, whether it be corneal GPs, hybrids or sclerals, works well to mask corneal irregularities and diminish higher-order aberrations.
One study reports that GP lenses provide superior visual performance and a greater reduction in third-order aberrations compared with soft toric contact lenses in keratoconus patients.1 GP lenses reduce corneal aberrations induced by irregular astigmatism by masking the irregular corneal surface with the regular refractive surface of the rigid GP lenses and a liquid tear lens.2,3
A GP contact lens is indicated in the presence of irregular astigmatism and when a manifest refraction does not yield acceptable visual acuity with no other ocular pathology present. Since irregular corneas are unique, there is no one lens type that will work for all. Thus, clinicians need to be proficient at fitting different specialty lens modalities to improve the likelihood of success. The three keys to contact lens success are:
- Maintaining corneal and anterior segment health
- Maximizing comfort
- Improving vision
Topography is essential to understanding corneal shape. It includes knowing the profile (prolate or oblate), symmetry, location, area and magnitude of curvature and elevation. To start, evaluate anterior segment health to collect baseline measurements and rule out complicating factors. An attempt at manifest refraction is also necessary. All this data will help determine an appropriate lens design and fitting method (diagnostic vs. empirical). Let’s see which options can best benefit your patients.
Corneal GPs
These lenses were the mainstay for irregular cornea management for decades, but developments with scleral and hybrid lens designs have demoted corneal designs to a secondary status. A recent survey indicated that 36% of practitioners fit corneal (including intralimbal) GP lenses on the majority of their keratoconus patients, second to scleral lenses at 39%.4
Fitting a corneal GP on a cornea with very mild irregularity or form fruste keratoconus is similar to fitting a normal cornea for refractive error. However, this task becomes increasingly difficult with increases in irregularity.
When fitting corneal GP designs, avoid heavy apical bearing. A mild touch that provides divided support and doesn’t result in corneal staining is appropriate. At the conclusion of the eight-year CLEK study, 31% of patients who wore flat-fitting lenses with apical touch developed corneal scarring, whereas only 9% of steep fits with apical clearance developed scarring.5 Along with lens discomfort, flatter fits were associated with an increased likelihood of penetrating keratoplasty.6 Therefore, avoiding apical bearing is crucial to avoid corneal complications and improve peripheral lens alignment.
Depending on the lens design, the diameter and curve widths can be variable or fixed. Small overall diameter (OAD) and back optic zone diameter (BOZD) lenses are best suited for relatively well-centered ectasias or irregularities (Figure 1).7 As irregularities such as decentered ectasias and mild pellucid marginal degeneration become steeper and more peripheral, they require an increasingly larger OAD and BOZD.
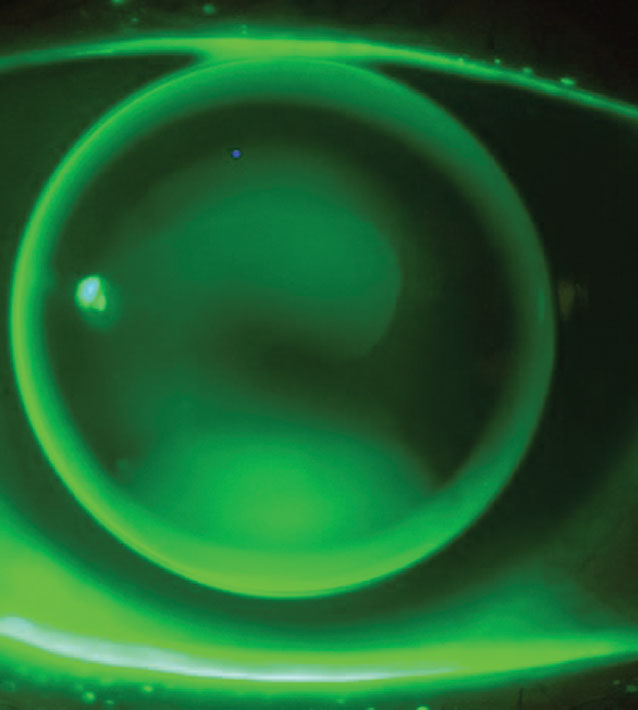 |
| Fig. 1. The “three-point touch” pattern of a small (9.2mm) OAD lens for a patient with keratoconus. Click image to enlarge. |
There are many ways you can choose your first diagnostic lens, but, as designs vary, it is typically best to follow the fitting guide. When in doubt, choosing a diagnostic lens with a base curve (BC) close to average keratometry value can be a good place to start. Let the lens settle so the fluorescein can dissipate for a few minutes and then evaluate the fluorescein pattern.
If apical clearance or bearing is present, modify the base curve in 0.50D to 1.00D steps until feather touch is achieved.7 A “three-point touch” pattern or minimal apical clearance is the goal. With three-point touch, there is light bearing in the periphery nasally and temporally (two points) and at the apex of the irregularity (third point) and definite peripheral clearance. With both smaller-diameter and intralimbal designs, you can customize the peripheral curves with toric or quadrant-specific curves to improve edge alignment and centration. Generally, an oblate cornea can be effectively fit with a reverse geometry curve.
When to choose this lens. Many irregular cornea patients are already habitual GP lens wearers. If they have acceptable vision, are well-adapted and maintain corneal health, continue. Corneal GPs work well for mild to moderate corneal irregularity and when there is less than 350µm of corneal elevation difference along the greatest meridian of change.8 This is a good option for challenging scleral obstacles to fit around, such as filtering blebs.
Piggyback Systems
Patients who desire the optics of a corneal GP with the comfort and protection of a soft lens underneath can consider this modality, which is often overlooked. Only around 2% of keratoconus patients use it, yet it can be a real problem-solver.9
There are two main fitting approaches for this modality. The first is to fit the corneal GP and then use a low-powered, low modulus, hyper-Dk soft lens underneath, which will minimally affect the fitting relationship and the power of the system. The second option is to fit the soft contact lens to artificially change the contour of the cornea to aid in the fitting process. Topography over the soft lens maps the new contour, and guides how to fit the GP lens on top.
Corneal GP lenses will tend to center on the steepest area of the cornea, therefore a moderate- to plus-powered (approximately +6.00D) soft lens with a thicker center can be beneficial in patients who have decentered irregularities or who have oblate corneas to bulk up the center to aid in GP lens centration (Figure 2).10 A mild minus soft lens (approximately -3.00D) may be more appropriate in the case of keratoconus, as it has an artificial flattening effect and will allow use of a flatter and lower power GP lens.11 The power effect from the soft lens will be much less than you would expect by just adding the powers of the two lenses together—the result will be 21% of the labeled soft lens power.12
The patient’s comfort and tolerability of the lenses largely determines a successful piggyback fit. The soft lens and GP should move independently of one another, and the GP periphery should align nicely with the soft lens to avoid both adherence and excessive edge lift.
If a standard disposable soft lens does not achieve an adequate fitting relationship, a custom soft lens may be necessary. This will allow for a custom diameter base curve and power to aid the piggyback system. When using custom soft lenses with a recessed cavity in the center, the recess should be larger and deeper than the diameter and thickness of the GP lens, which will facilitate some movement while keeping the lid interaction minimal and stable.
When to choose this lens. Choose this option when a corneal GP fits well and is the correct lens option, but awareness or difficulty adapting is preventing success. This can also improve the centration of the GP, protect a focal elevation, such as an apical nodule or scar, or prevent epithelial disruption from an otherwise well-fitting corneal GP.
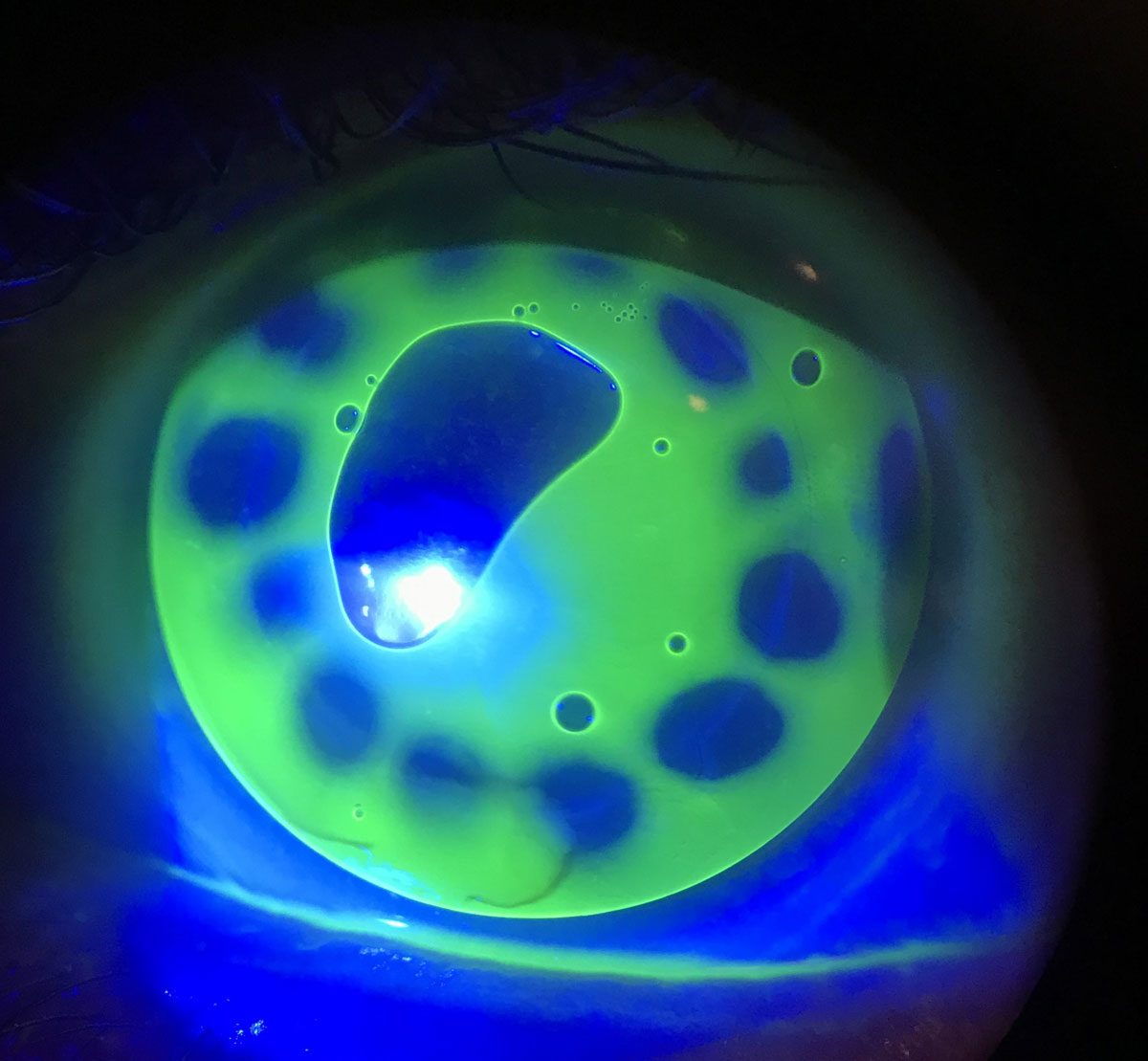 |
 |
| Fig. 2. Intralimbal GP on sunken corneal transplant. The steep central BC causes a central bubble, but midperiphery is aligned on the graft/host junction (top). The same GP piggybacked with a +7.00D silicone hydrogel soft lens (bottom). Click images to enlarge. |
Hybrids
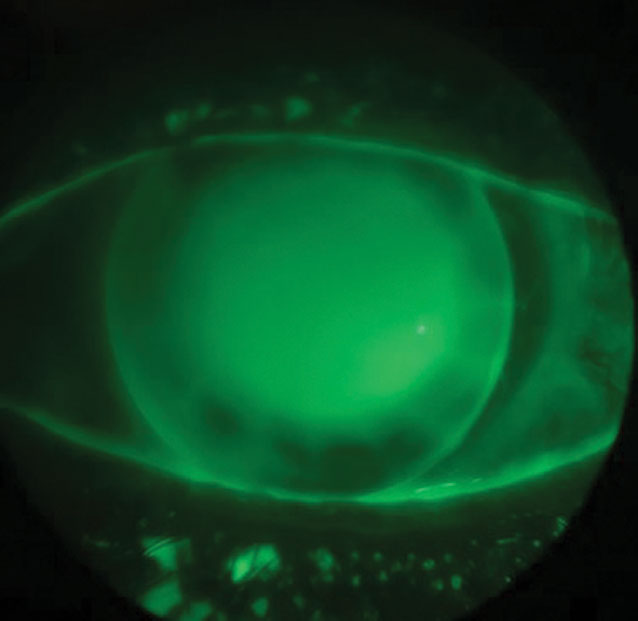
These lenses have a GP center hyper-bonded to a soft skirt. In the United States, there is only one manufacturer (SynergEyes) that offers multiple designs and geometries to accommodate a variety of corneal shapes, while the OAD and GP diameter is fixed. The GP portion of the lens uses variable base curves or sagittal depths to align with or vault the cornea, while the soft skirt has three to four different base curve radii that help facilitate movement, centration and tear exchange. The newer generation designs are available in higher oxygen-permeable materials for both lens portions and are designed specifically for vaulting the irregular cornea. This may reduce complications with neovascularization found in designs with low Dk materials.
An appropriately fitting hybrid lens will exhibit approximately 100µm clearance at insertion, as the lens may settle 30µm to 60µm after several hours of wear. The central GP portion should clear the cornea, with light touch on the mid-peripheral cornea at the GP-soft lens junction (the inner-landing zone) and land evenly on the soft skirt without fluting or impingement. The soft skirt (the outer landing zone) bears 80% of the weight of the lens system, making it more comfortable than corneal GPs.13,14 There should be movement upon blink initially, but movement after a few hours of wear may not be seen although there is tear exchange.
When to choose this lens. Hybrids serve as a great first-line option for mild to moderate central corneal irregularities or ectasias as well as for patients experiencing discomfort or centration problems with corneal GPs. It’s a logical transition for previous soft lens wearers who need a GP lens for improved vision, patients with a suboptimal experience with piggyback systems or those with complications from scleral lens wear, particularly lens reservoir fogging. Patients with significantly decentered irregularities, intracorneal rings, poor corneal rigidity (i.e., radial keratotomy), cornea transplants or those with significant ocular surface disease are less ideal candidates for hybrid lenses.
Sclerals
Scleral lenses are large diameter GP lenses that rest on the sclera, tucking under the lids and vaulting the cornea. This creates a tear reservoir behind the lens bathing the cornea in preservative-free saline, improving vision when other modalities were unsuccessful. These lenses are available with an abundance of modifications depending on the laboratory and their design.
Overall, diameters can be variable or fixed, and you can adjust their vault by changing their base curves or sagittal depths. Some designs compensate for changes to individual curves, allowing for a single parameter change to occur without affecting the rest of the fit. Many come in various geometries (oblate and prolate) with variable haptic designs (toric and quad-specific) to enhance scleral alignment and complete customization of the lens optics (sphere, front toric, multifocal). Some designs also incorporate additional customizations of notches, peripheral lifts, channels or microvaults to account for scleral obstructions.
There are three primary objectives in fitting a scleral lens—the lens must vault the cornea, clear the limbus and align with the sclera. A range of 100µm to 300µm of apical clearance and about 50µm over the limbus after settling is deemed acceptable. These lenses are primarily fit diagnostically.
When to choose this lens. This is the go-to for moderate to severe irregularities where there is significant asymmetry of the inferior and superior cornea. Sclerals are a good second-line option when patients fail with other lens modalities and are beneficial for patients with ocular surface disease and those suffering from contact intolerance due to dry eye.
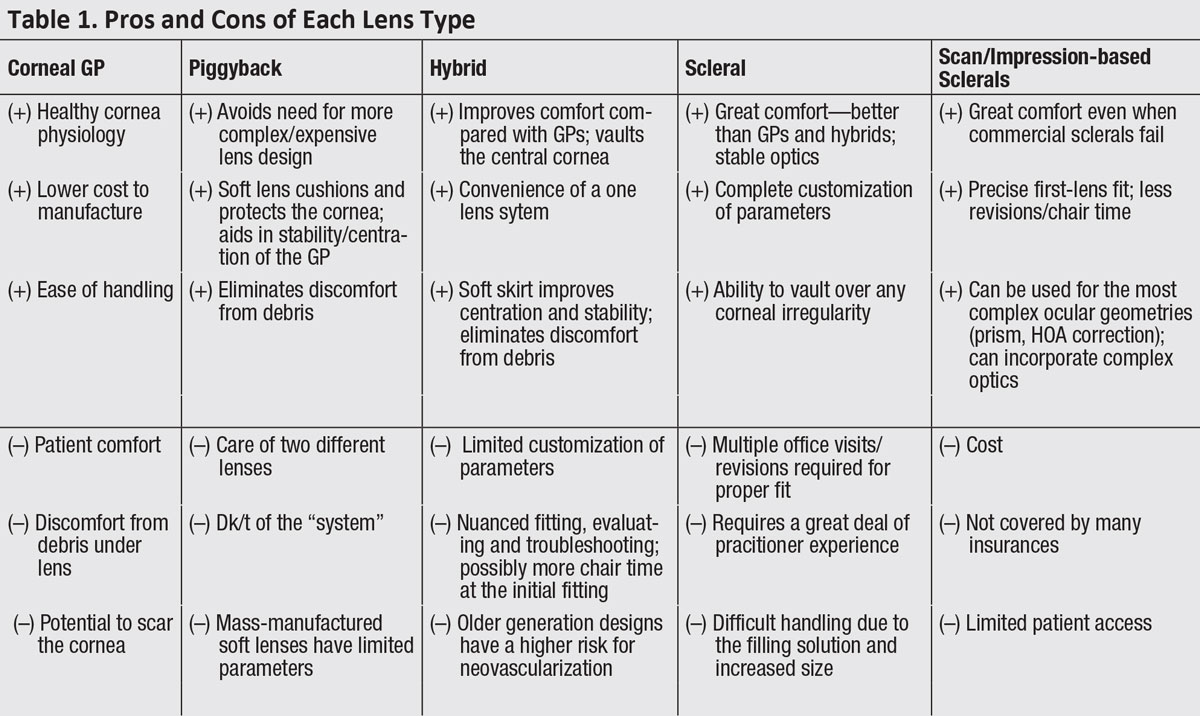 |
| Click table to enlarge. |
Scan/impression-based Sclerals
The availability of free-form, elevation-specific scleral designs allow practitioners to achieve an optimal fit on the most irregular and challenging cases.
An impression-based scleral prosthetic is developed in a process similar to those used in orthodontics. The impression is 3D-scanned, a model is generated, a points file is developed and the device is manufactured. A scan-based scleral uses a profilometer, similar to a wide field topographer.
This technology will drive empirical fitting of scleral lenses, such as the EyePrintPro, as well as further customization options. This is the ultimate in scleral technology and offers an option for those who have failed with traditional sclerals or for whom traditional sclerals are not an option. Currently, impression- and scan-based sclerals are limited to those practitioners who are certified and have the necessary devices.
When to choose this lens. If you have this option at your disposal, use it when a patient presents after being unsuccessful other commercially available scleral lenses. It can help patients who need a scleral lens but have significant time and/or travel constraints and cannot make the required multiple office visits sometimes necessary for the fitting of commercial scleral lenses.
This modality can benefit first-time scleral fits that have significant corneal irregularities, especially peripheral ectasias where decentering the optic zone can be key to achieving a successful fit, conjunctival abnormalities (such as pingueculae, pterygiums and/or filtering blebs) and/or asymmetric scleral contours. It is a great first-line option for patients who have especially complex anterior segment pathologies and are in immediate need of a perfect-fitting lens for ocular protection (i.e., Stevens-Johnson syndrome, persistent epithelial defect and other severe ocular surface disease). Lastly, it can be a last line of contact lens therapy before considering surgical intervention.
GP lenses are vital to vision rehabilitation for our irregular cornea patients. We are fortunate to have many options to offer them (Table 1). Being skilled in fitting different lens modalities will help clinicians make the best choices and meet the visual needs of these challenging but rewarding patients.
1. Jinabhai A, Radhakrishnan H, Tromans C, O’Donnell C. Visual performance and optical quality with soft lenses in keratoconus patients. Ophthalmic Physiol Opt. 2012;32(2):100-16. 2. Griffiths M, Zahner K, Collins M, Carney L. Masking of irregular corneal topography with contact lenses. CLAO J. 1998;24(2):76-81. 3. Kosaki R, Maeda N, Bessho K, et al. Magnitude and orientation of Zernike terms in patients with keratoconus. Invest Ophthalmol Vis Sci. 2007;48(7):3062-8. 4. Bennett ES. GP annual report 2019. Contact Lens Spectrum, 2019; 34(10):22-7. 5. Zadnik K, Barr JT, Steger-May K, et al. Comparison of flat and steep rigid contact lens fitting methods in keratoconus. Optom Vis Sci. 2005;82(12):1014-21. 6. Gordon MO, Steger-May K, Szczotka-Flynn L, et al. Baseline factors predictive of incident penetrating keratoplasty in keratoconus. Am J Ophthalmol. 2006;142(12):923-30. 7. Bennett ES, Barr JT, Szczotka-Flynn L. Keratoconus. In Bennett ES, Henry VA, eds., Clinical Manual of Contact Lenses (4th ed.). Philadelphia, Lippincott Williams & Wilkins; 2014:518-77. 8. Zheng F, Caroline P, Kojima R, et al. Corneal elevation differences and the Initial selection of corneal and scleral contact lens. Poster presented at the Global Specialty Lens Symposium. Las Vegas, January 2015. 9. Zadnik K, Barr JT, Edrington TB, et al. Baseline findings in the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study. Invest Ophthalmol Vis Sci. 1998;39(13):2537-46. 10. Bennett ES, Grohe RM, Anderson BW, et al. Piggyback applications in modern contact lens practice. Contact Lens Spectrum. 2007; 22(12):17. 11. Romero-Jiménez M, Santodomingo-Rubido J, González-Méijome JM, et al. Which soft lens power is better for piggyback in keratoconus? Part II. Cont Lens Anterior Eye. 2015;38(1):48-53. 12. Michaud L, Brazeau D, Corbeil ME, et al. Contribution of soft lenses of various powers to the optics of a piggy-back system on regular corneas. Cont Lens Anterior Eye. 2013;36(6):318-23. 13. Sclafani L, Alvis C. Utilizing technology instead of time to successfully fit the irregular cornea with hybrid lenses. Presented at the 2020 Global Specialty Lens Symposium. Las Vegas, NV. January 2020. 14. Nau AC. A comparison of synergeyes versus traditional rigid gas permeable lens designs for patients with irregular corneas. Eye Contact Lens. 2008;34(4):198-20. |


