Contact lenses remain one of the top choices for presbyopes when it comes to vision correction, especially considering the evolution of the multifocal contact lens. This modality has made significant strides in recent years, including better optics, improved materials, additional parameters and enhanced wearing schedules.
Still, once a patient is fit into a multifocal, retention often remains a hurdle.
“Vision and comfort are the two main challenges that I have in keeping presbyopes in contact lenses,” says optometrist Vince Zingaro of Malvern, PA. “Presbyopes tend to have dryer eyes than younger patients, so lens material and modality are important. I know if patients aren’t comfortable in their contact lenses, then there’s a good chance they’ll eventually drop out and become full-time glasses wearers.”
Here, contact lens experts offer guidance on how to tackle the three main challenges they see in multifocal dropout: vision, comfort and cost.
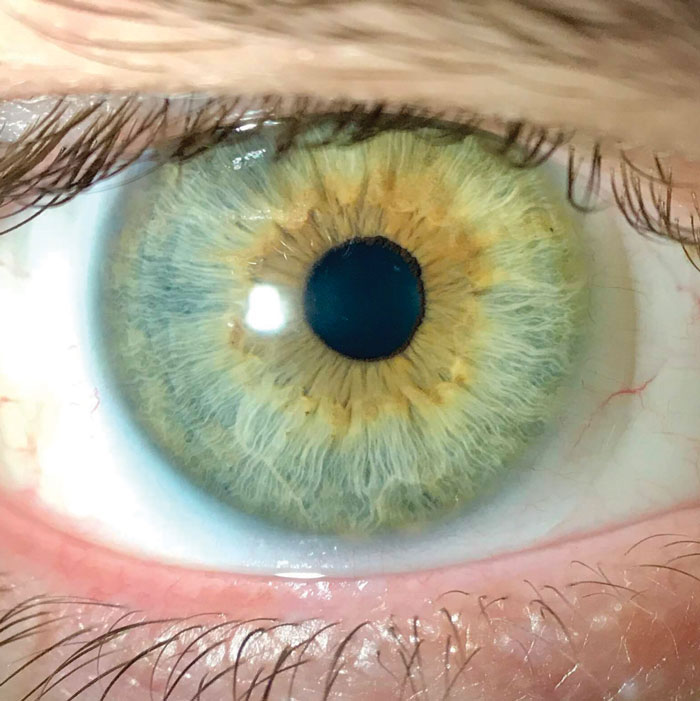 |
Soft multifocal contact lenses have made significant strides in recent years. Photo: Alex Nixon, OD, MS, and Erin Rueff, OD, PhD. Click image to enlarge. |
Issue #1: Vision
Good visual outcomes are of utmost importance when fitting presbyopes in multifocal contacts, explains Jennifer A. Dattolo, OD, of Woodstock, GA.
A recent study published in Optometry & Vision Science found poor vision was the main reason patients dropped out of multifocal lens wear.1 Another investigation found visual problems were most common among new multifocal contact lens wearers.2
Here are a few ways to optimize vision from start to finish:
Set expectations. Vision is the most important aspect in retaining contact lens wearers, Dr. Zingaro says. His method is as follows: “I explain to each presbyopic contact lens wearer that the technology is always getting better. If they were unsuccessful in a multifocal in the past, they may do better with today’s lenses.”
Dr. Zingaro also ensures the goal of a multifocal lens is clear to patients: get them through most of the day without the need for reading glasses. He notes that these lenses provide “softer” vision compared with glasses. He then reinforces to patients that they will still be able to see well without having to rely on readers, except when viewing small print or reading in dimly lit environments, for example. He focuses on the positives.
“With so many patients working on the computer for their job, I explain that they will no longer need to worry about tilting their head up and down to find the sweet spot in their vision as they often need to do with progressive glasses,” Dr. Zingaro says. “This is a great advantage to many patients, especially now with so many people working remotely on a computer all day.”
 |
Vision, comfort and cost remain barriers to multifocal contact lens wear in presbyopes. Photo: Erin Rueff, OD, PhD. Click image to enlarge. |
Setting realistic vision expectations from the beginning is essential, confirms David Anderson, OD, of Miamisburg, OH.
Dr. Anderson first asks a patient how they prioritize their daily activities. “I find out their pain points, visual challenges and areas of focus,” he says. Sometimes a multifocal doesn’t check every box, but using such a lens to give a patient freedom from glasses during an activity they enjoy, such as hiking or exercising, is a great start. “One pair of glasses isn’t always going to satisfy every visual need, and neither will one pair of contact lenses, so you may need to have different options for different activities,” he notes.
Be transparent with patients that multifocals aren’t perfect, but that there is usually—but not always—a way to achieve working vision at all distances, Dr. Dattolo follows up with.
“I believe if you tell patients the truth and set expectations from the beginning, they will be much more successful,” she explains.
Optimize the fit. Any practitioner who fits multifocals can affirm it’s often a step-by-step process, with several different lens parameters attempted before dispensing the final fit.
To ensure best visual outcomes, Dr. Zingaro always follows the manufacturer’s fitting guide. “I used to ‘wing it’ and try to fit multifocal contact lenses my own way, but I wasn’t very successful. I think using your resources wisely is important for the long-term success of the patient because they may be so desperate to not have to wear glasses in the short-term that they give up some vision in contacts just to have freedom from glasses,” he says.
Unfortunately, problems are also due to occur down the road when the presbyopia worsens, and the patient may opt to wear reading glasses and drop out of contact lens wear entirely since they no longer see value in the lenses.
“I’ve had patients tell me they used to wear monovision contacts or multifocal contacts but they ‘stopped working,’” Dr. Zingaro explains. “Rather than talk with their doctor about it, they just stopped wearing the lenses. If you follow the fit guide each time you examine the patient, you’re constantly optimizing their vision, which will keep them happy and reduce the chance of them giving up on contacts or, worse, finding a new doctor to help them.”
Adapt to changes. Flexibility is key in the multifocal process, especially if a patient’s visual needs change.
Dr. Anderson recently saw a patient who traded in her multifocal contacts for a pair of readers. Due to the pandemic, the patient was working in front of the computer more than she was driving, which was the initial reason for her distance multifocal lenses. With the switch-up in her daily routine, Dr. Anderson changed her multifocal lens to a center-near design.
For patients who don’t gain crisp and clear vision from standard soft multifocals, gas permeable multifocals tend to offer a higher quality of vision, says optometrist Andrew Fischer of Jasper, IN. There can be a steep learning curve associated with the adaption period, so he suggests guiding patients through the process.
“It’s important that we listen, ask the right questions and find solutions to solve patients’ problems,” Dr. Anderson says. “There are many different multifocal lens designs, and we shouldn’t get stuck fitting the same lens on every patient. While that may work for a large percentage of individuals, this approach won’t work on everyone, and it will open the door for more dropouts.”
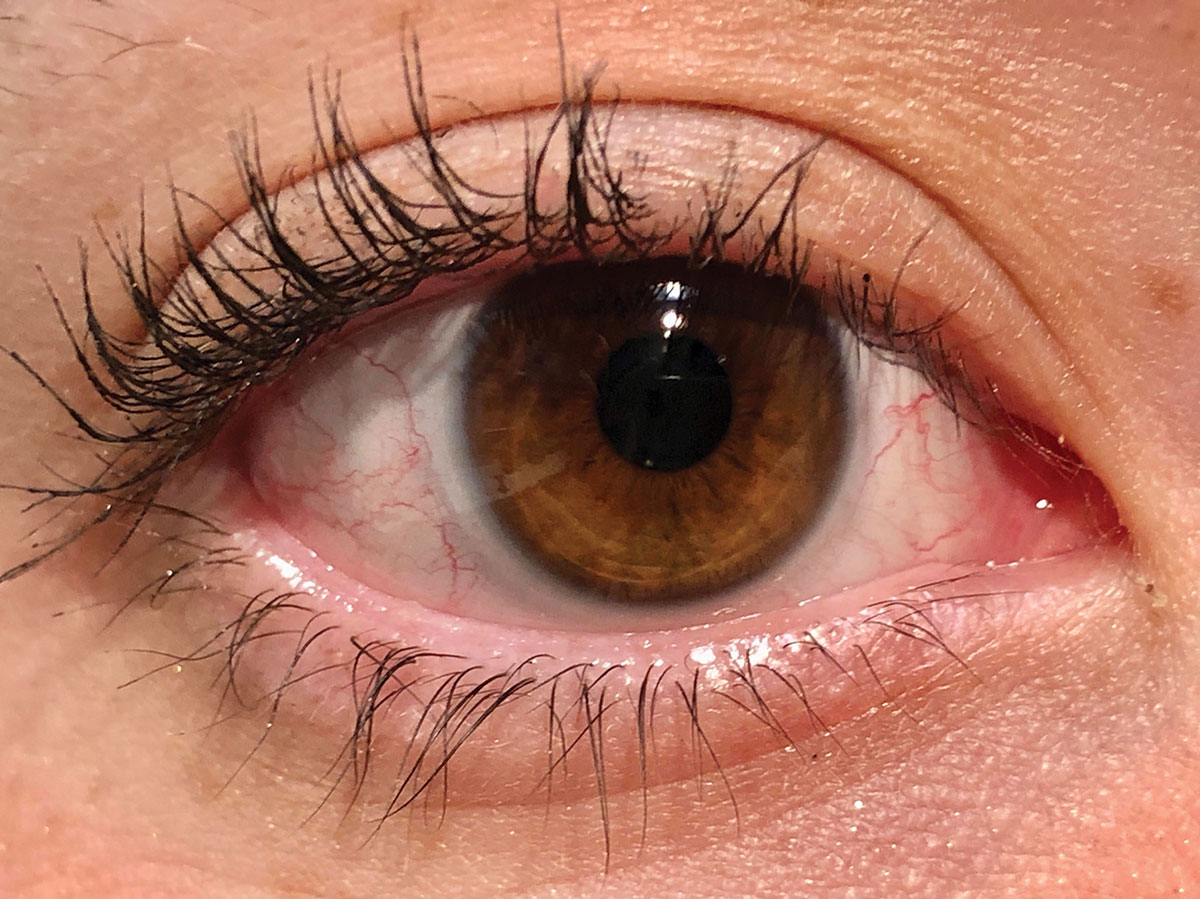
 |
Lens discomfort, commonly caused by dry eye, is a leading cause of dropout. Photo: Jalaiah Varikooty, Centre for Contact Lens Research, University of Waterloo, Ontario. Click image to enlarge. |
Issue #2: Comfort
Studies have reported that changes to the tear film and ocular surface can exacerbate lens discomfort—a key factor in lens dropout.3-5
Another leading cause of dropout is contact lens dryness. It is vital to address these issues with all contact lens patients, including presbyopes, at every visit, Dr. Fischer says.
Ocular surface health. “At times, despite wearing a well-fitting, highly breathable lens, patients just can’t seem to get comfortable. When this happens, I often hit pause on the contact lens fitting process and shift the focus to improving the ocular surface,” Dr. Fischer explains.
Part of this process involves a dry eye screening, which includes corneal and lissamine green staining, meibomian gland expression, lid margin evaluation and blink assessment. This can highlight problem areas that require improvement for optimum contact lens comfort.
“Sometimes even the best daily disposable contacts won’t provide all-day comfort because the problem isn’t with the contact, but instead with the ocular surface. When these issues are mitigated, comfortable contact lens wear can be achieved again,” Dr. Fischer suggests.
Studies have shown that early treatment for underlying comfort issues caused by dry eye may promote additional years of comfortable contact lens use.5
Replacement schedule. Dr. Fischer also considers lens modality if comfort issues arise. “If the patient is wearing a monthly or another frequent-replacement contact lens, switching to a high-quality daily disposable can help tremendously,” Dr. Fischer suggests.
Screen usage. If the patient is in a good contact lens and has no clear evidence of dry eye or ocular surface disease but is still experiencing discomfort, their work environment is often the culprit, Dr. Fischer says. “I find that patients who are on screens a majority of the day tend to have more comfort issues with contact lenses.” This may be due to a decreased blink rate or more incomplete blinks while on the computer, he explains. Other considerations include fans, drafty rooms and dirty or dusty environments.
“Changing the work environment can make all the difference,” Dr. Fischer says.
Patient meds. In addition to heavy screen use, Dr. Dattolo suggests another cause of discomfort: the dry eye–causing medications many presbyopic contact lens wearers take for conditions such as hypertension, high cholesterol, diabetes and thyroid issues.
In these cases, Dr. Dattolo instructs patients to make a conscious effort to blink while in front of electronic devices, hydrate throughout the day, take fish oils and maintain proper eyelid hygiene. She also recommends daily disposable contacts for patients who suffer from dry eye, as wearing fresh lenses every day helps lessen the role dry eye plays.
Coming Soon: Presbyopia-masking DropsPoised to enter the presbyopia-correcting market are half a dozen drops currently making their way through FDA approval. One of the more novel drops works to change the composition of the lens, while others are miotic in nature and constrict the pupil, creating a pinhole effect. Dr. Fischer believes these new drop options will offer an exciting alternative for presbyopes. “I think this will allow patients who don’t want to wear glasses or transition into multifocal contacts the opportunity to have clear near vision without correction,” he says. “I would imagine these drops would compete with presbyopia-correcting contact lenses. I am excited to get first-hand experience with these drops to see how patients respond to them.” Here’s what’s on deck: UNR844-Cl (Novartis) breaks disulfide bonds, which helps the lens become more elastic and regain some functionality.1 This drop, formerly known as EVO6, is in Phase II clinical trials.1 Allergan’s AGN-199201 and AGN-190584 are both miotic-based drops that work by constricting the pupil.2 In February 2021, Allergan submitted a New Drug Application (NDA) to the FDA for AGN-190584 for the treatment of presbyopia. The FDA is expected to act on the NDA by the end of 2021.1 Yolia’s True Vision Treatment combines customized contact lenses and specially formulated eye drops to provide a noninvasive, binocular treatment for presbyopia.2 The Liquid Vision PRX-100 (Presbyopia Therapies) drop contains aceclidine and low-dose tropicamide to create a miotic pupil without the accommodative effect.2,3 The CSF-1 drop (Orasis) is a parasympathomimetic agent with a nonsteroidal anti-inflammatory in an oil-based formulation that causes a miotic pupil and increases the eye’s depth of focus.2 FOV Tears affects the ciliary muscle, which causes a physiological accommodation and a dynamic pseudoaccommodation.2,3 These drops, once approved, may be ideal for patients who have difficulty with inserting and removing lenses, have prescriptions that don’t allow for ideal presbyopic multifocal wear or had laser vision correction and aren’t interested in wearing glasses or contacts again, Dr. Zagaro says. He believes the drops will compete with multifocals only if they are able to deliver the same visual outcomes. Still, not all doctors are sold. “I honestly don’t think I’ll be one of the first on board to try them with my patients,” Dr. Dattolo says. Many lens wearers cringe at the sight of eye drops, and for those who work long days, the question is whether the drops will be able to provide near vision for the entire duration, she notes.
|
Issue #3: Cost
The out-of-pocket expense for multifocal wearers can be a factor for some patients, especially if the lens isn’t meeting their expectations, Dr. Anderson says. “If the lens is working and the individual is free from glasses, then cost becomes less of a factor. But, truthfully, the cost is reasonable for what the lens is expected to do.” And a little bit of education and reassurance goes a long way.
To mitigate patients’ initial cost concerns, Dr. Zingaro lets his patients test drive a trial lens. He also explains the how and the why behind his selection of a particular lens specific to the patient and their individual needs. He believes this helps the patient realize the lens is a necessary medical device and not an arbitrary commodity.
Additionally, Dr. Zingaro takes time during the exam to explain insurance coverage and manufacturer rebates, both of which can bring down the cost.
“Finally, I assure the patient that I am available for them throughout the year should they feel that their vision is declining,” he says. If a patient’s lenses aren’t to their satisfaction or if their prescription changes before the next annual exam, Dr. Zingaro exchanges any unopened boxes. “They can order an annual supply of contact lenses without having to worry about getting stuck with ones they can’t wear,” he says.
Fortunately, many of Dr. Fischer’s patients don’t view cost as a barrier to vision correction. “After experiencing near vision difficulties, most of these patients understand that a more premium lens is necessary for them to reach their visual goals compared with their standard lenses,” he says.
When cost is more of a factor, Dr. Fischer explains that the more advanced optics of a multifocal contact lens are the reason for the higher price tag. He also provides a price comparison chart that details different lens options. This gives the patient some input in the fitting process, Dr. Fischer adds.
“I also make sure they are aware that the cheapest lens doesn’t always provide the best fit, best vision or safest lens for their eye. They should never sacrifice their eye health for cheaper lenses,” Dr. Fischer explains.
Cost tends to play the biggest role for patients who wear a daily disposable multifocal, Dr. Dattolo says. When the price becomes an issue, she suggests another wearing schedule option. The financial burden is also less significant for those who only wear the lenses for special occasions.
Takeaways
Despite the challenges many practitioners face in keeping their presbyopes in multifocals, this modality remains a go-to option.
“With the advancements made in contact lenses, both with better materials for increased comfort and improved designs for better vision, I still believe they are the way to go,” Dr. Dattolo says. “We can now successfully fit presbyopic astigmats in multifocal contacts. I look forward to seeing where multifocal contact lenses are in the next few years. I believe they will only get better.”
1 Rueff EM, Varghese RJ, Brack TM, et al. A survey of presbyopic contact lens wearers in a university setting. Optom Vis Sci. 2016;93(8):848-54. 2. Sulley A, Young G, Hunt C. Factors in the success of new contact lens wearers. Cont Lens Anterior Eye. 2017;40(1):15-24. 3. Dumbleton K, Woods CA, Jones LW, et al. The impact of contemporary contact lenses on contact lens discontinuation. Eye Contact Lens. 2013;39(1):93-9. 4. Richdale K, Sinnott LT, Skadahl E, et al. Frequency of and factors associated with contact lens dissatisfaction and discontinuation. Cornea. 2007;26(2):168-74. 5. Pucker AD, Jones-Jordan LA, Marx S, et al. Clinical factors associated with contact lens dropout. Cont Lens Anterior Eye. 2019;42(3):318-24. |


